ADULT ECHOCARDIOGRAPHY ABBREVIATIONS
advertisement

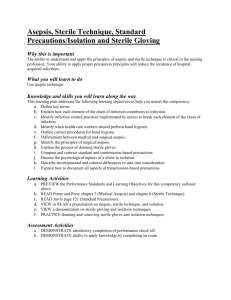
ADULT ECHOCARDIOGRAPHY Lecture 4 Technique and Patient Care Harry H. Holdorf PhD, MPA, RDMS, RVT, LRT, N.P. Technique • High gain destroys resolution • The goal is even brightness of tissue throughout the image. Patient care • Electrical Safety – Always use proper grounded electrical devices with threeprong plugs. – Avoid the use of extension cords. – Do not use any device with frayed cords. – Inspect systems routinely. – During an ECG, patient should not be grounded, but chassis of ECG machine should be grounded. Patient relations, confidentiality & Assessment • In 1996, Congress enacted the Health Insurance Portability and Accountability Act, or HIPAA. • The primary purpose was continuity of health insurance coverage if you change jobs, but is also provided for standards for health information transactions and confidentiality and security of patient data. This confidentiality portion will most affect the day-to-day workflow among health care professionals. Privacy • Privacy is somewhat different than confidentiality. It refers to individuals’ right to keep some information to themselves and to have it used only with their approval. Under HIPAA, physicians must use and disclose only the minimum necessary amount of patient information needed fro the purpose in question. The institution may use and disclose patient information for treatment, payment, and health care operations without patient authorization. Most other uses and disclosures of patient information require such an authorization. • Liability – Holds each individual responsible for their actions. • Negligence – Doing something that a reasonable person will not do or Not doing something that a reasonable person would do. • Informed consent – Protects doctor from claims of unauthorized procedure. In order to be legally binding, patient must be capable of giving consent (before given morphine, etc.) For invasive procedures, informed consent should be given to operating physician or cardiologist. • Interpretation of exams – Sonographers cannot provide interpretation of exam to patient. Interpretation must come from physician. • Malpractice – Claims can be avoided by effective communication between patients and medical personnel. • Denial – The refusal to acknowledge the existence or severity of unpleasant external realities or internal thoughts and feelings. • Initial assessment – Including vitals, are used to establish a baseline to compare future results. • Wheelchair – Moving a patient in or outbrakes engaged, footrests retracted. Foley Catheter • An indwelling Foley catheter is a flexible plastic tube that is inserted through the urethra into the bladder, to drain urine. • To keep the catheter for slipping out, it as a balloon on the end that is inflated with sterile water or saline once the end is inside the bladder. • Keep the urinary drainage bag below the level of he bladder to keep the fluid flowing from the bladder into the collection bag. If the bag is elevated above the bladder, urine will collect in the bladder. Sterilization • Sterilization is the elimination of all transmissible agents (such as bacteria and viruses) from a surface or a piece of equipment. This is different from disinfection, where only organisms that can cause disease are removed by a disinfectant. • In general, any instrument that enters an already sterile part of the body (such as the blood, or beneath the skin, should be sterilized. This includes equipment like scalpels, hypodermic needles, and artificial pacemakers. • Pathogens or infectious agents are biological agents that causes disease or illness to its host. Pathogens disrupt the normal physiology or an animal or plant. The term pathogen is derived from the Greek “Birth of Pain”. • The human body has many natural defenses against some of the more common pathogens in the form of the human immune system and by some helpful bacterial present in the human body’s normal flora. • However, if the immune system or good bacteria is damaged, pathogenic bacteria that were being controlled can multiply and cause harm to the host. Such cases are called opportunistic infections. • Flora- Mucus membranes, such as the intestinal lining, are constantly in contact with environmental organisms and become readily colonized by various microbial species, called flora. • Pathogens are responsible fro massive amounts of casualties and have harmful effects on affected groups. (AIDS) Methods of Sterilization Preferred principle for sterilization is through heat and pressure. There are also chemical methods of sterilization. 1. Autoclaves A widely-used method for heat sterilization is the autoclave. Autoclaves use steam heated to 121 degrees C (250 F)and pressure at 103 kPa (15 psi) above atmospheric, for 15 minutes. The steam and pressure transfer heat into organisms to kill them. Useful parameters – time and temperature. 2. Chemical Sterilization Chemicals are also used for sterilization. Although heating provides the most effective way to destroy transmissible agents, it is not always appropriate, because it destroys objects such as fiber optics, electronics, and plastics. Ethylene oxide (EO) gas is commonly used to sterilize objects that cannot survive temperatures greater than 60 degrees C, such as plastics, optics, and electrics. • Sepsis – Means to soil or dirty. “A” means without. • Aseptic means without microorganisms. Aseptic technique refers to practices that reduce post procedure infection in patients by decreasing the likelihood that microorganisms will enter the body during clinical procedures. Sterile Fields • A sterile field is an area created by placing sterile towels or surgical drapes around the procedure site and on the stand that holds sterile instruments used during the procedure. • The doctor’s sterile area is the only area that should come in contact with the sterile field. Only sterile objects and personnel may be allowed in the sterile field. The sterile area should be draped starting from the area closest to the person and extending outward. • • • While a sterile field is created around a procedure site, items below the level of the draped client are outside the field and are not sterile. A properly gowned and gloved person’s sterile area extends from the chest to the level of the sterile field. Sleeves are sterile from 5 cm ( 2 inches) above the elbow to the cuff. Once a sterile object comes in contact with a non-sterile object or person or with dust or other airborne particles, the object is no longer sterile. If even one non-sterile object or person enters the sterile field, the field is no longer sterile. For example, sterile objects become contaminated if you touch the object with your bare hand, if the object comes into contact with dust or other airborne particles, or if the object is held below the level of the sterile field. The spike of an IV set is sterile and must not come in contact with non-sterile objects. To maintain the Sterile Field 1. Do not place sterile items near open window or doors 2. Place only sterile items within the sterile field 3. Do not contaminate sterile items when opening, dispensing, or transferring them 4. Consider items located below the level of the drape to be unsterile. 5. Do not allow sterile personnel to reach across unsterile areas or to touch unsterile items. 6. Do not allow unsterile personnel to reach across the sterile field or to touch unsterile items. 7. Recognize and maintain the provider’s sterile area. 8. Recognize that the edges of a package containing a sterile item are considered unsterile. 9. Recognize that a sterile or high-level disinfected (HLD) barrier that has been penetrated (wet, cut, or torn) is considered contaminated 10. Be conscious of where your body is at all times, and move within or around the sterile or HLD field in a way that maintains sterility or HLD status. Radiopaque objects: block radiation and appear white on a x-ray film. Bodily Fluid Spills • Care must be taken with blood, vaginal secretions, saliva in dental procedures or any body fluid that is visibly contaminated with blood. In addition, care must be taken in situations where it is difficult or impossible to differentiate between body fluids. • Universal precautions in emergency situations suggest that all body fluids are potentially infected material (PIM). Infectious fluids can enter our bodies through: • • • • • Absorption through mucus membranes covering the body openings Through an open, bleeding wound Through damaged areas of the skin, caused by other severe skin diseases. Mucus membranes are much thinner than normal skin. Microscopic cuts in the membranes can allow germs to cross the membrane and enter the blood stream. Also, fluids can be absorbed through these membranes even without any cuts or breaks. Normal skin is much thicker than mucous membranes and provides a good barrier to blood diseases. Infectious fluids cannot be absorbed through skin that is intact. Have these materials on hand for cleaning up spills: • A durable container to store the clean up supplies • Several biohazard labeled bags • Disinfectant-freshly prepared 10% solution of household breach ( 1 part bleach and 9 parts water, or add ½ cup bleach to 1 quart water) or other commercial chlorine or iodine based disinfectant • Inert absorbing material (Kitty litter) • A small dust pan and hand brush • Personal protective equipment, including several pairs of latex gloves, goggles, face masks, coveralls, and paper boots. • A roll of paper towels • Antiseptic wipes Cleaning a Blood Spill 1. If blood has spilled onto you, it should be thoroughly washed off as soon as possible. If the material has spilled on your clothing and soaked through so that that is skin contact, the cloths must be removed. Following removal, wash those areas where exposure is evident, even to the point of taking a shower. If blood or PIM has come into contact with any of the mucous membranes (eyes, nose, lips) they need to be thoroughly rinsed. If there is contact with open wounds or cracks (chapped skin) in the skin, there is a risk of exposure. Immediately and thoroughly wash your hands with water and soap or an antiseptic cleaner if contaminated with a body fluid. 2. When clean up involves blood or a flat surface, you should first delineate and mark the spill area so that others do not inadvertently enter the area until clean up is complete. 3. Soak the area for at least 20 minutes with a disinfectant (freshly prepared 10% bleach solution). You can be liberal with disinfectant but don’t apply so heavily that it begins to run. 4. Allow at least 20 minutes with a disinfectant to complete the decontamination. You can use the small hand broom and dustpan to clean up the spill. 5. Deposit all clean up material in bio-waste disposal bag and close tightly. The bag should be secured in a biohazard BURN BOX. Carefully remove gloves, coveralls, and boots (if used) and discard in a biowaste bag. If used, the facemask should also be disposed. Goggles can be disinfected, rinsed, and reused. The dustpan and broom can be disinfected and reused. 6. Record and report the incident to your supervisor. End Lecture four NEXT: THE AORTIC VALVE