The Respiratory System - Maria Regina High School
advertisement

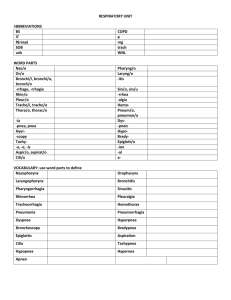
THE RESPIRATORY SYSTEM Chapter 13 Pgs 436-463 Functional Anatomy Basics Nose Pharynx Larynx Trachea Bronchi Bronchioles Alveoli Detailed Anatomy Upper Respiratory Tract Homeostatic Imbalance: Cleft Palate – failure of the bones forming the palate to fuse medially. Results in breathing difficulties and oral cavity functions such as chewing and speaking. Rhinitis – inflammation of the nasal mucosa. Causes nasal congestion and postnasal drop Sinusitis – sinus inflammation. Difficult to treat and may cause changes in voice quality. Blockage of the sinus cavities may result in sinus headache Tonisillitis – inflammation of tonsils, often the pharyngeal tonsil Choking leading to need for Heimlich Maneuver or tracheostomy Anatomy and Functions of Lungs Occupy entire thoracic cavity except for the mediastinum Apex is narrow and superior, base is broad and rests on the diaphragm Left lung: two lobes Right lung: Three lobes Surface of each lung coated in pulmonary (visceral) pleura and the walls of the thoracic cavity are lined with the parietal pleura Both produce pleural fluid There is no actual space between membranes but it can exist in pathological conditions Homeo. Imbalance: Pleurisy – insufficient or overproduction of pleural fluid Anatomy of thoracic cavity Functional Anatomy of Lungs Cont. Respiratory zone includes respiratory bronchioles, alveolar ducts, alveolar sacs and alveoli. This is the only location for gas exchange All other respiratory passages are conducting zone structures that serve as conduits Most of the lungs are air space and the stroma is mostly elastic CT that passively recoils during exhalation Respiratory Membrane Walls of alveoli are simple squamous epithelium Alveolar pores connect alveoli to provide alternate air routes The alveolar surface is covered with capillaries The respiratory membrane (air-blood barrier) is the alveolar and capillary walls, their fused BMs and occasional elastic fibers Respiratory Membrane All gas exchange via diffusion Alveolar macrophages present in alveoli Additional cuboidal cells produce surfactant Lung surface area ~50-70 m2 SE Micrographs of Rat Lung 3D Image of conducting zone and respiratory zone structures Respiratory Physiology – 4 Events Pulmonary ventilation – a.k.a. breathing. Air moves in and out of lungs for refreshment of air supply 2. External respiration – gas exchange between alveoli and pulmonary blood. The lumen of the alveoli are technically on the body exterior 3. Respiratory gas transport – blood transport of gases 4. Internal respiration – gas exchange between systemic capillaries and tissue Note: The actual use of oxygen and carbon dioxide production is part of cellular respiration 1. Breathing Mechanics Basic concept: Volume changes lead to pressure changes, which lead to the flow of gases to equalize the pressure Breathing is entirely mechanical: When the volume of the space increases, gas particles spread out to fill the space and pressure drops in the space. Relates to inspiration When the volume of the space decreases, gas particles are compressed together and the pressure in the space increases. Relates to expiration Intrapleural pressure, (pressure between visceral and parietal pleura) is always negative. If it equalizes, the lungs will collapse completely Inspiration Diaphragm and external intercostals contract and increase the size of the thoracic cavity The height of the cavity increases The rib cage lifts and sternum moves forward increasing diameter of cavity A pressure decrease ensues as the intrapulmonary volume increases, this sucks air into the lungs like a vacuum until the pressure equalizes Expiration A passive process that depends mostly on elasticity of lung tissue As the diaphragm and intercostals relax, intrapulmonary volume decreases and pressure increases above atmospheric pressure, thus air leaves the lungs until pressure equalizes Only during forced expiration are the internal intercostal muscles and abdominal muscles used to force air out. May be necessary during respiratory illness Pressure and Volume Changes Close up View of Pleura Intrapleural pressure is negative upon inspiration and positive with expiration The Interplerual pressure (IPP) is always negative. If it weren’t, the lungs would collapse Homeostatic Imbalance Atelectasis – lung collapse Occurs when air enters the pleural space through a chest would or rupture of the visceral pleura Presence of air in the intrapleural space is referred to as pneumothorax Lungs reinflate by using chest tubes in the intrapleural space to draw out the air Description of Lung Volume Measurements Respiratory capacity is affected by: - Age, body size, sex, physical conditions Tidal Volume (TV): Normal breathing moves about 500 mL of air into and out of the lungs with each breath Lung Volumes Continued Inspiratory reserve volume (IRV) – the amount of air that may be forcibly inhaled after TV Expiratory reserve volume (ERV) – amount that may be forcibly exhaled after TV Residual volume – the amount that stays in the lungs and may never be exhaled. Allows continuous gas exchange in between breaths and keeps alveoli inflated Vital Capacity – total amount of exchangeable air. TV + IRV + ERV. ~3100 mL in women, 4800 in men Dead space volume – amount of air stuck in conducting system that is never involved in gas exchange. About 150 mL in normal tidal breath. Functional volume (TV) is about 350 mL Another Idealized tracing of respiratory volumes Nonrespiratory Air Movements Usually result from reflex activity, though some may be voluntary Cough – clears lower respiratory passageways. A deep breath followed by closing of the glottis and a subsequent forceful burst of air passed the glottis Sneeze – similar to the cough. Clears upper respiratory area. The uvula depresses and closes pharynx forcing air out through nasal cavities Crying – inspiration followed by a number of short expirations. Emotionally induced Laughing – same as crying movement-wise Hiccups- sudden inspirations resulting from spasms of the diaphragm; initiated by irritation of the diaphragm or phrenic nerves Yawn – deep inspiration with jaws wide open. Ventilates all alveoli Respiratory Sounds Bronchial sounds – produced as air rushes through the large respiratory passageways Vesicular breathing sounds – air filling the alveoli. Very very quiet. Homeostatic Imbalances: diseased tissue may produce abnormal sounds in presence of mucus, inflammation or pus. Crackle – bubbling sound Wheezing – whistling sound Rales – bronchial sounds produced by presence of mucus or exudate in the lung passages or by thickening of the bronchial walls Gas Exchange External respiration – exchange of gas between alveoli and blood Internal respiration – exchange between systemic blood and tissues All gas exchange is based on diffusion Gas Transport in the Blood Oxygen carried in RBCs as oxyhemoglobin. Carbon dioxide mostly transported as bicarbonate ion (HCO3 ), which is part of the blood buffer system Formation of this molecule occurs in the RBCs, then the ion diffuses into plasma Very small amount is dissolved in plasma A small amount (20-30%) of CO2 is carried bound to hemoglobin in the RBCs For CO2 to be exhaled, the bicarbonate reaction must be reversed in the RBC and freed CO2 diffuses from the blood into the alveoli Reversal: H+ ions bind with HCO3- to form carbonic acid: H2CO3, which quickly splits into water and CO2 Homeostatic Imbalances Hypoxia – impaired oxygen transport. Skin and mucous membranes take on a bluish hue, a.k.a.: cyanotic. May result from anemia, pulmonary disease, or impaired or blocked blood circulation Carbon monoxide poisoning – CO competes with oxygen for the same binding sites on hemoglobin, and binds with higher affinity, thus oxygen can’t be transported and tissues become hypoxic Leading cause of death from fire Gas Transport in the Blood Cont. Internal respiration – as CO2 diffuses out of cells, it reacts with water to form carbonic acid (H2CO3), with quickly releases the bicarbonate ions, HCO3-, in the RBCs via carbonic anhydrase Conversely, oxygen diffuses out of the RBCs, through the plasma and into the cells Neural Regulation of Respiration The phrenic and intercostal nerves control the basic rhythm of breathing by stimulating the diaphragm, respiratory muscles and external intercostals. The neural centers are located in the pons and medulla Contains pacemaker called the ventral respiratory group (VRG) The medulla also contains a center to modify the pacemaker rhythmically; the pons smoothes out the basic rhythm Normal breathing is called eupnea; 12 – 15 bpm Bronchioles and alveoli have “stretch receptors” that kick in via vagus nerve when the lung begins to overinflate Hyperpnea – vigorous breathing due to increased physical activity The rate of breathing may not increase, but the volume of air exchange may Respiration becomes more active and abdominal muscles, along with others, may be used to assist expiration Homeostatic Imbalance- high doses of central nervous system depressants may inhibit the respiratory center of the medulla causing death Breathing control Centers Nonneural Regulators of Respiration Physical factors – talking, coughing, exercising, increased body temperature, etc. Volition – conscious control, may be overridden Emotional factors- gasping, holding breath in anticipation, breathing quickly from fear, etc. Chemical factors – the blood buffer system; CO2 levels rising causes the blood pH to drop and CNS receptors take notice. Changes in oxygen are picked up by chemoreceptors in the carotid arteries (carotid bodies) but are secondary to CO2 concentrations Homeostatic Imbalances of Regulators People who have chronically high levels of CO2, such as those with emphysema, are not able to use those levels for regulation, thus low oxygen becomes the stimulus for breathing Patients with these disorders are put on low-oxygen air flow, otherwise they will cease respiration Acidosis and alkalosis occur when the blood becomes to acidic or alkaline Hyperventilation – occurs with deep, rapid breathing and is used to “blow off” extra carbon dioxide (due to increased carbonic acid) to prevent or correct acidosis Hypoventilation – shallow, slow breathing allows carbon dioxide to build up in the blood, lowering pH and prevents or corrects alkalosis Respiratory Disorders Chronic obstructive pulmonary diseases – exemplified by chronic bronchitis and emphysema Almost always linked to smoking Dyspnea – difficulty/labored breathing becomes increasingly worse Cough and frequent pulmonary infections Most COPD victims are hypoxic, retain CO2, and have respiratory acidosis Lung cancer Squamous cell carcinoma – 25-30% of cases, arises from epithelial linings Adenocarcinoma- 40%, arises from solitary nodules in bronchial glands and alveolar cells Small cell carcinoma – 20%, lymphocyte-like cells that start in main bronchi and spread aggressively to mediastinum forming grapelike clusters Extremely difficult to treat. New therapies include using antibodies to target and/or deliver toxic drugs to the tumor, 2) cancer vaccines, 3) gene therapy Developmental Aspects of the Respiratory System It takes about 2 weeks post-birth for the infant respiratory system to become fully functional due to the production of surfactant Necessary for lowering surface tension and preventing lung collapse between breaths Does not develop in sufficient quantity until the 28-30 weeks of pregnancy Premature babies at risk for Infant respiratory distress syndrome (IRDS) Cystic fibrosis – the most common lethal genetic disease: 1/2400 births. Oversecretion of mucus due to lack of Cltransporters Treatment: Antibiotics, “clapping the chest,” mucus-dissolving drugs Homeostatic Imbalances Sudden infant death syndrome – exact cause unknown. Possible causes: problem with neural control of respiration or reinhalation of expired air Asthma – chronic inflammation and hypersensitivity of airways. May be caused by allergens, pathogens, environmental changes, physiological changes Sleep apnea – disruption of the pressure in the pharynx, which is necessary for keeping the glottis open during sleep, allows the glottis to slide back closing off the trachea, preventing inspiration until neural gas sensors force inspiration. Sufferers become hypoxic during sleep and exhibit a wide array of symptoms during wakeful hours