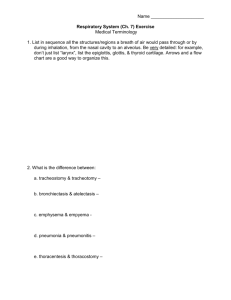
Respiratory System
advertisement

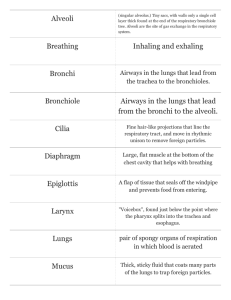
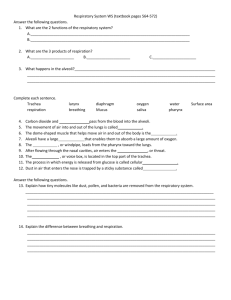
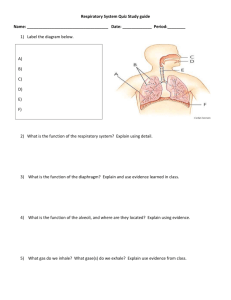
Respiratory System Respiration • Pulmonary ventilation (breathing): movement of air into and out of the lungs • External respiration: O2 and CO2 exchange between the lungs and the blood • Transport: O2 and CO2 in the blood • Internal respiration: O2 and CO2 exchange between systemic blood vessels and tissues Respiratory system Circulatory system Respiratory System: Functional Anatomy • Major organs – Nose, nasal cavity, and paranasal sinuses – Pharynx – Larynx – Trachea – Bronchi and their branches – Lungs and alveoli Nasal cavity Nostril Oral cavity Pharynx Larynx Trachea Carina of trachea Right main (primary) bronchus Right lung Left main (primary) bronchus Left lung Diaphragm Figure 22.1 Functional Anatomy • Respiratory zone: site of gas exchange – Microscopic structures: respiratory bronchioles, alveolar ducts, and alveoli • Conducting zone: passageway to gas exchange sites – Includes all other respiratory structures • Respiratory muscles: diaphragm and other muscles that promote ventilation • Functions – Provides an airway for respiration – Moistens and warms the entering air – Filters and cleans inspired air – Serves as a resonating chamber for speech – Houses olfactory receptors • Mucosa – Pseudostratified ciliated columnar epithelium – Cilia move contaminated mucus posteriorly to throat Paranasal Sinuses • In frontal, sphenoid, ethmoid, and maxillary bones • Lighten the skull and help to warm and moisten the air Pharynx • Muscular tube that connects to the – Nasal cavity and mouth superiorly – Larynx and esophagus inferiorly Nasopharynx Oropharynx • From the base of Laryngopharynx the skull to the level of the sixth cervical vertebra (b) Regions of the pharynx Larynx • Attaches to the hyoid bone and opens into the laryngopharynx • Continuous with the trachea • Functions 1. Provides an airway 2. Routes air and food into proper channels 3. Voice production Hyaline cartilage keeps larynx and trachea open Epiglottis: elastic cartilage; covers the larynx during swallowing Epiglottis Body of hyoid bone Thyrohyoid membrane Cuneiform cartilage Corniculate cartilage Arytenoid cartilage Arytenoid muscles Cricoid cartilage Thyrohyoid membrane Fatty pad Vestibular fold (false vocal cord) Thyroid cartilage Vocal fold (true vocal cord) Cricothyroid ligament Cricotracheal ligament Tracheal cartilages (b) Sagittal view; anterior surface to the right Figure 22.4b Base of tongue Epiglottis Vestibular fold (false vocal cord) Vocal fold (true vocal cord) Glottis Inner lining of trachea Cuneiform cartilage Corniculate cartilage (a) Vocal folds in closed position; closed glottis (b) Vocal folds in open position; open glottis Figure 22.5 Voice Production • Speech: intermittent release of expired air while opening and closing the glottis • Pitch is determined by the length and tension of the vocal cords • Loudness depends upon the force of air • Chambers of pharynx, oral, nasal, and sinus cavities amplify and enhance sound quality • Sound is “shaped” into language by muscles of the pharynx, tongue, soft palate, and lips Trachea • Windpipe Mucosa: ciliated pseudostratified epithelium with goblet cells Rings of Hyaline Cartilage Posterior Mucosa Submucosa Esophagus Trachealis muscle Lumen of trachea Seromucous gland in submucosa Hyaline cartilage Adventitia Anterior (a) Cross section of the trachea and esophagus Figure 22.6a Conducting Zone Structures • Trachea right and left main (primary) Trachea bronchi • Each main bronchus enters one lung Middle lobe of right lung Superior lobe of left lung Left main (primary) bronchus Lobar (secondary) bronchus Segmental (tertiary) bronchus Inferior lobe of right lung Inferior lobe of left lung – Right main bronchus is wider, shorter, & more vertical than the left Superior lobe of right lung Conducting Zone Structures • From bronchi through bronchioles, structural changes occur – Cartilage rings give way to plates; cartilage is absent from bronchioles – Epithelium changes from pseudostratified columnar to cuboidal; cilia and goblet cells become sparse – Relative amount of smooth muscle increases Respiratory Zone • Respiratory bronchioles, alveolar ducts, alveolar sacs (clusters of alveoli) • ~300 million alveoli account for most of the lungs’ volume and are the main site for gas exchange Alveoli Alveolar duct Respiratory bronchioles Terminal bronchiole (a) Alveolar duct Alveolar sac Three Types of Cells found in alveoli - Type I Cells – simple squamous cells; allow for gas diffusion - Surfactant Cell (Type II) – produce an oily secretion; it reduces surface tension so lungs don’t collapse - Alveolar Macrophages – Clear/swallow 2 million dust cells out of your lungs/hour. Type II Cell Macrophage Red blood cell Nucleus of type I (squamous epithelial) cell Alveolar pores Capillary O2 Capillary CO2 Alveolus Alveolus Type I cell of alveolar wall Macrophage Endothelial cell nucleus Alveolar epithelium Fused basement membranes of the Respiratory alveolar epithelium membrane and the capillary Red blood cell endothelium Alveoli (gas-filled in capillary Type II (surfactantCapillary air spaces) secreting) cell endothelium (c) Detailed anatomy of the respiratory membrane Figure 22.9c Right lung Right superior lobe (3 segments) Left lung Left superior lobe (4 segments) Right middle lobe (2 segments) Right inferior lobe (5 segments) Left inferior lobe (5 segments) Figure 22.11 Blood Supply • Pulmonary circulation (low pressure, high volume) – Pulmonary arteries deliver systemic venous blood • Branch profusely, along with bronchi • Feed into the pulmonary capillary networks – Pulmonary veins carry oxygenated blood from respiratory zones to the heart Blood Supply • Systemic circulation (high pressure, low volume) – Bronchial arteries provide oxygenated blood to lung tissue • Arise from aorta and enter the lungs • Supply all lung tissue except the alveoli – Pulmonary veins carry most venous blood back to the heart Mechanics of Breathing • Pulmonary ventilation consists of two phases 1. Inspiration: gases flow into the lungs 2. Expiration: gases exit the lungs Caused by changes between atmospheric gas pressure (14.7 psi) and gas pressure in the lungs Atmospheric pressure Movement of air always flows from higher gas pressure to lower gas pressure Thoracic wall 756 760 Lung Diaphragm Intrapleural pressure 756 mm Hg (–4 mm Hg) Intrapulmonary pressure 760 mm Hg (0 mm Hg) Figure 22.12 Pulmonary Ventilation • Inspiration and expiration • Mechanical processes that depend on volume changes in the thoracic cavity – Volume changes pressure changes – Pressure changes gases flow to equalize pressure Boyle’s Law • The relationship between the pressure and volume of a gas • Used to explain the mechanics of breathing • Under constant temperature, Pressure (P) varies inversely with volume (V): P1V1 = P2V2 P=1/V • Lungs can change volume, so air pressure in lungs will also change Inspiration • An active process – Inspiratory muscles contract – Lungs are stretched and volume increases – Air pressure in lungs drops – Air flows into the lungs Sequence of events Changes in anteriorposterior and superiorinferior dimensions Changes in lateral dimensions (superior view) 1 Inspiratory muscles contract (diaphragm descends; rib cage rises). 2 Thoracic cavity volume increases. Ribs are elevated and sternum flares as external intercostals contract. 3 Lungs are stretched; External intercostals contract. intrapulmonary volume increases. 4 Intrapulmonary pressure drops. 5 Air (gases) flows into lungs down its pressure gradient until intrapulmonary pressure is 0 (equal to atmospheric pressure). Diaphragm moves inferiorly during contraction. Figure 22.13 (1 of 2) Expiration • Quiet expiration is normally a passive process – – – – – Inspiratory muscles relax Thoracic cavity volume decreases Elastic lungs recoil and volume inside lungs decreases Pressure inside lungs increases Air flows out of the lungs • Note: forced expiration is an active process: it uses abdominal and internal intercostal muscles Sequence of events Changes in anteriorposterior and superiorinferior dimensions Changes in lateral dimensions (superior view) 1 Inspiratory muscles relax (diaphragm rises; rib cage descends due to recoil of costal cartilages). 2 Thoracic cavity volume Ribs and sternum are depressed as external intercostals relax. decreases. 3 Elastic lungs recoil External intercostals relax. passively; intrapulmonary volume decreases. 4 Intrapulmonary pres- sure rises. 5 Air (gases) flows out of Lungs. Diaphragm moves superiorly as it relaxes. Figure 22.13 (2 of 2) Lung Volumes Tidal volume Inspiratory reserve volume Expiratory reserve volume Vital Capacity Residual Volume Total Lung Capacity Tidal volume – normal breath in and out Vital Capacity – total amount of air you can forcefully inspire and expire in one respiratory cycle Physical Factors Influencing Pulmonary Ventilation • Inspiratory muscles consume energy to overcome three factors that hinder air passage and pulmonary ventilation 1. Airway resistance 2. Lung compliance 3. Lung Elasticity Airway Resistance • As airway resistance rises, breathing movements become more strenuous • Severely constricting or obstruction of bronchioles – Can prevent life-sustaining ventilation – Can occur during acute asthma attacks and stop ventilation • Epinephrine dilates bronchioles and reduces air resistance Air Resistance • Friction in the respiratory passageways, decreases the flow of gases. • I.e. Asthma attack, constriction of bronchiole tubes • Accumulation of mucus (infections) • Cystic Fibrosis - mutation on chromosome #7 where lungs produce too much mucus – Leads to poor gas exchange since mucus blocks diffusion of gases. Lung Compliance • The ease at which lungs stretch • Decrease in Lung compliance occurs when: – Smaller passageways are blocked • Diminished by – Nonelastic scar tissue (fibrosis) – Reduced production of surfactant – Decreased flexibility of the thoracic cage Lung Elasticity • The lungs’ ability to recoil • I.e. Emphysema – Air sacs enlarge and lose their elasticity; lungs remain over inflated