Beta-lactam Antimicrobial Agents
advertisement

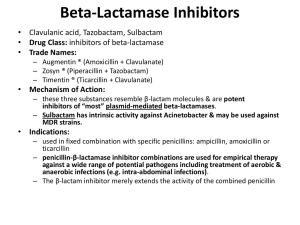
BETA-LACTAM ANTIMICROBIAL AGENTS Alan M. Stamm, M.D. astamm@uabmc.edu October 23, 2002 Beta-lactams • Each agent has this 4-member ring which is essential for antibacterial activity. Outline • • • • • • Mechanism of action. Mechanisms of resistance. Pharmacology. Adverse effects. Classes of beta-lactams. Clinical uses. Mechanism of Action - 1 • Interference with cell wall synthesis: prevention of cross-linking of linear peptidoglycan strands by inhibition of transpeptidase, carboxypeptidase, or endopeptidase. • Inhibition occurs by competitive binding to enzyme located beneath cell wall on inner surface of cell membrane. Mechanism of Action - 2 • Structural weakening leads to cell death. • Effect is bactericidal or lethal, not bacteriostatic or inhibitory. • However, the effect depends on: – active multiplication/division of bacteria – beta-lactam penetration of cell wall – affinity of beta-lactam for enzyme, a.k.a. penicillin binding protein (PBP) – activation of autolytic system of bacteria Mechanisms of Resistance - 1 • Production of beta-lactamase: bacterial enzyme catalyzing hydrolysis of betalactam ring. – chromosomal vs. plasmid DNA – one vs. multiple in a single bacterium – dozens exist with varying spectrums • e.g., Staphylococcus aureus - penicillinase Mechanisms of Resistance - 2 • Decreased access of drug to target penicillin binding protein. – exclusion by outer membrane protein channels = porins – augmented efflux mechanisms • e.g., Enterobacter species • e.g., Pseudomonas aeruginosa Mechanisms of Resistance - 3 • Alteration of penicillin binding protein: decreased affinity, less effective competitive inhibition. – clinical isolates are often broadly resistant to antibacterial agents • e.g., drug resistant Streptococcus pneumoniae • e.g., methicillin resistant Staph. aureus (MRSA) • e.g., vancomycin resistant Enterococci (VRE) Pharmacology - 1 • Absorption: some are acid stable and absorbed in the duodenum - peak serum level in 1-2 hours; many are administered only intravenously. • Half-life: most are short, ~1 hour; with serious disease, these must be administered 4-6 times per day or as a continuous infusion. Pharmacology - 2 • Elimination: primarily by glomerular filtration and tubular secretion; decreased in patients with renal impairment; reduce dose if creatinine clearance <40-50 ml/min. • Biliary excretion is predominant for nafcillin and significant for ureidopenicillins. Efficacy • A principal determinant is T>MIC = the proportion of time for which betalactam level at the site of infection exceeds the minimal inhibitory concentration of the bacterium. Adverse Effects - 1 • IgM-mediated erythematous, maculopapular, trunkal rash. • Diarrhea, Clostridium difficile colitis. • Hemolytic anemia, neutropenia, thrombocytopenia, bleeding. • Fever. • Interstitial nephritis. • Anicteric hepatitis, cholestatic jaundice. • Seizures. Adverse Effects - 2 • • • • Comparatively safe. Safe in pregnancy. Phlebitis from IV administration. Superinfection from alteration of normal flora. – e.g., thrush (oral candidiasis) • Selection of resistant bacteria. – particularly 3rd generation cephalosporins Allergy • IgE-mediated urticaria, anaphylaxis. • From 1-10% report allergy to penicillin; 10-30% of these have a positive skin test. • Cross-reactivity occurs with other betalactams: 10% with cephalosporins. • Detection: history, skin testing - penicilloylpolylysine and penicillin G. • Management: avoidance, substitution, desensitization - PO or IV. Penicillins - 1 • Natural penicillins: – for streptococci, normal oral flora, meningococci, anaerobes – benzylpenicillin = penicillin G • aqueous Na+ or K+ crystalline IV • procaine IM • benzathine (Bicillin) IM – phenoxymethylpenicillin = penicillin V PO Penicillins - 2 • Penicillinase resistant penicillins: – for methicillin susceptible Staphylococcus aureus (MSSA) – nafcillin IV – cloxacillin PO – dicloxacillin PO Penicillins - 3 • Extended spectrum penicillins: – more broadly active against gramnegatives – aminopenicillins • ampicillin IV • amoxicillin PO – ureidopenicillins (acylaminopenicillins) • piperacillin IV Penicillins - 4 • Penicillin + beta-lactamase inhibitor combinations: – even more active against gram-negatives – ampicillin + sulbactam (Unasyn) IV – piperacillin + tazobactam (Zosyn) IV – amoxicillin + clavulanate (Augmentin) PO Cephalosporins - 1 • 1st generation: – active against streptococci, methicillin susceptible staphylococci, some gramnegatives – cephapirin (Cefadyl) IV – cefazolin (Ancef, Kefzol) IM, IV – cephalexin (Keflex) PO Cephalosporins - 2 • 2nd generation: – more broadly active against gram-negatives – cefuroxime (Kefurox, Zinacef) IV, (Ceftin) PO • 2nd generation: – added activity against anaerobes – cefotetan (Cefotan) IV Cephalosporins - 3 • 3rd generation: – much broader and better activity against gram-negatives (but less vs. staphylococci) – ceftriaxone (Rocephin) IV – cefotaxime (Claforan) IV – few have added activity against Pseudomonas aeruginosa, e.g., ceftazidime (Ceptaz, Fortaz, Tazicef, Tazidime) IV Cephalosporins - 4 • 4th generation: – activity against a broader range of gram-negative bacilli; better penetration of outer membrane and less affinity for beta-lactamases – cefepime (Maxipime) IV Cephalosporins - 5 • Cephalosporins are not useful in the treatment of infections due to methicillin resistant Staphylococcus aureus (MRSA), Enterococci, or Listeria monocytogenes. Carbapenems • The most broadly active of antibacterial agents - streptococci, MSSA, gramnegatives, anaerobes: – imipenem/cilastatin (Primaxin) IV – meropenem (Merrem) IV • Induce production of beta-lactamases by gram-negative bacilli. • Hold in reserve – do not use routinely. Carbacephems • Greater chemical stability in solution. • Activity similar to 2nd generation cephalosporin cefuroxime: – lorcarbef (Lorabid) PO • No need to use this class. Monobactams • Active against aerobic gram-negative bacilli; resistant to hydrolysis: – aztreonam (Azactam) IV • An alternative to an aminoglycoside. • Do not induce production of betalactamases. • Minimal risk of reaction in those allergic to penicillins. Selection of Antibiotics - 1 • Patient factors: – history of antibiotic allergy – pharmacogenomic profile – recent antibiotic exposure – age and organ dysfunction – status of host defenses – disposable income Selection of Antibiotics - 2 • Infectious disease factors: – source of acquisition - community, travel, occupation, nosocomial – site of infection - likely pathogens and their usual susceptibility patterns – severity of infection Selection of Antibiotics - 3 • Antibiotic factors: – cidal vs. static – route of administration & schedule of dosing – tissue penetration – spectrum of antimicrobial activity – local pattern of antimicrobial resistance or proven susceptibility – potential adverse effects & drug interactions Selection of Antibiotics - 4 • Public health considerations: – prevention of transmission – induction of resistance – cost Respiratory Infections • Pharyngitis due to Streptococcus pyogenes (Group A streptococci): – penicillin V or amoxicillin 250 mg PO tid x 10 days • Community acquired pneumonia: – ceftriaxone 2 g IV qd (often with a macrolide) initially if hospitalized Urinary Tract Infections • Pyelonephritis: – ceftriaxone 2 g IV qd initially if hospitalized Sexually Transmitted Diseases • Gonorrhea: – ceftriaxone 125 mg IM once • Syphilis: – early stages - benzathine penicillin G 2.4 million units IM once – neurosyphilis - aqueous penicillin G 3 million units IV q 4 hours x 10 days Skin / Soft Tissue Infections • Cellulitis: – nafcillin 1 g IV q 4 hours initially if hospitalized or cephalexin 500 mg PO qid • Diabetic foot infection: – cefotetan 2 g IV q 12 hours or piperacillin/tazobactam 3.375 g IV q 6 hours Central Nervous System Infections • Meningitis: – ampicillin 2 g IV q 4 hours + ceftriaxone 2 g IV q 12 hours + vancomycin initially pending results of cultures and susceptibility tests Endocarditis • Due to viridans Streptococci: – ceftriaxone 2 g IV qd + gentamicin x 2 weeks • Due to Enterococcus fecalis: – ampicillin 2 g IV q 4 hours + gentamicin x 4-6 weeks Surgery - Prophylaxis • Cardiovascular: – cefazolin 1 g IV once 30-60 minutes prior to procedure Summary • Beta-lactam antibiotics are often the treatment of choice because of their efficacy and safety. • Learn how to use one agent from each of the classes. • Adjust your practice in accordance with changes in susceptibility.