John Lynch - Hamilton Health Sciences
advertisement

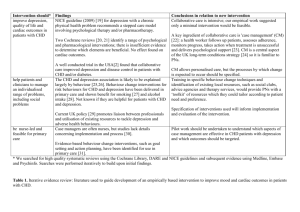
Social Inequality, Psychosocial Factors and CHD: What Have We Learned from the Research in Rich Countries? John Lynch Department of Epidemiology, Biostatistics and Occupational Health McGill University, Montreal, Canada PURE - Dubai, January 2006 What have we learned from social epidemiology? CHD Rate / 100K The Social Gradient in CHD Social Disadvantage Social Advantage The First Whitehall Study 5 4 *Adjust for smoking, blood pressure, cholesterol, overweight etc 4.0 RR 3.2 3 2.6 2.1 2 2.3 35% Clerical Other 1.8 1 0 Administrative Professional Rose and Marmot. Br Heart J (1981) “The social class difference was partly explained by known coronary risk factors: men in the lower grades smoked more and exercised less, they were shorter and more overweight, and they had higher blood pressures and lower levels of glucose tolerance. Most of the difference, however, remains unexplained. It seems that there are major risk factors yet to be identified, …” Rose and Marmot (1981, p.13) “… if these aspects of lifestyle account for less than a third of the social gradient in mortality, what accounts for the other two thirds? The second question occupies the rest of this book.” (p. 45 of 320) Marmot (2004) Implications (1) 1. There must be other mechanisms at the individual and contextual level that generate social gradients in CHD such as stress, job control, autonomy, social participation, neighborhood effects, social capital, etc. i.e., a range of psychosocial factors Psychosocial factors in social epidemiology Type A Behavior Pattern Stress Cynical Distrust Sense of Coherence Anger/Anger-in/Anger-out/ Hardiness Hostility Optimism Social Isolation John Henryism Social Support Job Strain Control Ways of Coping Sense of Control Anxiety Mastery Self esteem Hopelessness Resilience Depression Social cohesion Social capital CHD Implications (2) 2. Interventions focused on health behaviors and conventional risk factors are unlikely to appreciably reduce the social gradient in health. For instance, a 1998 JAMA study that has been cited more than 200 times (Web of Science), stated that, “Thus, public health policies and interventions that exclusively focus on individual risk behaviors have limited potential for reducing socioeconomic disparities in mortality.” (p. 1707) Behaviours do not matter Behaviours matter but they are just not the “big story” The downplaying of behaviours and their physiological correlates in understanding social inequalities in CHD influences research, funding, interventions and policy. Social Inequality Control Depression Stress behaviours P-N-E Immune Function Traditional Risk Factors INTERHEART: PAR ~ 75% CHD What have we learned from CHD epidemiology? • Conventional risk factors – smoking, hypertension, dyslipidemia and diabetes do explain most CHD in populations • INTERHEART study (2004) show PAR for 4 conventional risk factors is 76% • Emberson, Whincup, et al (2005) in BRHS show smoking, blood pressure and cholesterol account for 81% PAR (adjusted for regression dilution bias) • Stamler (1992,1999) and Greenland (2003) show that 75-100% of all CHD cases occur among those exposed to at least one conventional risk factor A Paradox? So how can it be that the factors accounting for most CHD in a population do not seem to account for most of the social gradient in CHD, when the social gradient simply emerges from sub-grouping the population according to some indicator of social position? A Paradox? Lipids, hypertension, smoking, diabetes 1000 cases of CHD Most educated 100 Middle educated 300 Least educated 600 700 600 500 400 300 200 100 0 Le a s t E duc a t e d M o st E duc a t e d An Illustration • Population sample of 2,682 Finnish men – Kuopio IHD Study • Stratified the population into lower and higher risk groups based on standard clinical definitions - current smoking, hypertension, dyslipidemia and prevalent diabetes • 34.7% were current smokers, 58.7% had hypertension, 42.7% had dyslipidemia, 6.5% had diabetes, and 84.9% had at least one of these risk factors • Fatal (ICD9 codes 410-414) and nonfatal CHD, classified according to MONICA criteriia • There were 425 CHD events (108 fatal, 317 non-fatal) during an average follow-up of 10.5 years. Lynch, Davey Smith, Harper, Bainbridge. J Epidemiol Community Health (in press) Accounting for Cases of CHD in this Population • Of the 425 total cases - 402 (94.6%) occurred among men exposed to at least one of the four conventional risk factors • 70%+ of cases occurred in men with at least 2 risk factors • PAR ~ 70% • Similar to INTERHEART (PAR ~ 75%) and with US cohorts where 90%+ of cases occur among those exposed to at least one conventional risk factor Thus these results are consistent with the idea that conventional risk factors DO EXPLAIN the vast majority of CHD cases Accounting for the Social Gradient in CHD in this Population • Social gradient in CHD comparing high to low education is RR = 1.90 • After adjustment for conventional risk factors RR = 1.68 • This corresponds to a 24% reduction in the excess RR Thus these results are consistent with the idea that conventional risk factors DO NOT EXPLAIN the social gradient in CHD What would population levels and social gradients in CHD look like if there were no conventional risk factors in this population? Whole KIHD Population N = 2,682 N (%) Low Risk Segment of KIHD Population N = 404 (15.1%) No. of Risk RR Cases (per Risk (%) K) N (%) ER (per K) No. of Risk RR Cases (per Risk (%) K) ER (per K) Education Education 1,121 218 (41.8) (51.3) 194 1.83 88 < Primary 122 8 school (30.2) (34.8) 66 1.63 25 Some high 1,128 161 school (42.1) (37.9) 143 1.35 37 Some high 184 11 school (45.5) (47.8) 60 1.46 19 433 46 (16.1) (10.8) 106 1.0 0 High school graduate 41 1.0 0 2,682 158 - - Total 57 - - < Primary school High school graduate Total 425 98 4 (24.3) (17.4) 404 23 250 Excess Risk (whole pop) Excess Risk (“low risk” pop) CHD Risk / 1000 200 150 194 RR = 1.8 = 88 per 1000 = 25 per 1000 Make it a low risk pop = 72% reduction in the excess risk of social inequality in CHD 143 100 50 0 106 66 RR = 1.6 60 Low risk population Low risk population Least Educated 41 Low risk population Most Educated In a low risk population with no smoking, hypertension, dyslipidemia and diabetes • Relative social gradient in CHD remains RR = 1.8whole vs 1.6low risk • Absolute social gradient is reduced by 72% ER = 88whole vs 25low risk per 1,000 Which social inequality is “better”? Original social inequality in CHD CHD Rate / 100K Give the disadvantaged the same risk factor levels as the most advantaged If we intervened to substantially reduce risk factors in all social groups Social Disadvantage Social Advantage • Within an absolute risk framework, there is no paradox between the observations from CHD and social epidemiology. Conventional risk factors do account for most CHD and for most of the absolute social gradient in CHD (72% of the excess risk). • However, when explaining relative social gradients in CHD, the apparent paradox may arise that the factors which explain most cases of CHD do not explain the relative social gradient. • Adjustment for conventional risk factors only reduced the relative social gradient in CHD by 24%. This is normally interpreted to mean that most of the effects of social inequality on CHD do not work through mechanisms linked to conventional risk factors. What does it take to be a confounder? • The extent to which a 3rd variable reduces the RR in an exposure-outcome association (an indication of confounding of the association) depends on the relative distributions of the exposure over strata of the 3rd variable and the strength of its association with the outcome. • In this case there is a more extreme relative distribution of education over strata of hopelessness than over strata of the conventional risk factors (partly because the prevalence of conventional risk factors is high), and so hopelessness/depression appears to be a stronger confounder (in this case interpreted as a mechanism) of the association between education and CHD. Depression Education 28% Social Gradient RR=1.9 24% Conventional Risk Factors CHD on the basis of the adjusted RR analysis we would normally interpret hopelessness/depression as an important mechanism in the causation of the social gradient in CHD How important are these 2 mechanisms? • intervene to eliminate hopelessness / depression reduces the relative social gradient 28% eliminates 14% of CHD cases (confounded estimate) • intervene to eliminate smoking, hypertension, dyslipidemia and diabetes smaller reduction in the relative social gradient – 24% eliminate 90%+ of CHD cases and 72% of the absolute social gradient • 72% reduction in ER is an underestimate because “low risk” population is not really low risk • No differences in blood pressure and have higher BMI • but low risk population has ex-smokers, higher cholesterol and LDL, and are 5 cm shorter • Deciding on the “importance” of various risk factors for elucidating the mechanisms behind social gradients in CHD cannot be done on the basis of relative comparisons alone. • As Geoffrey Rose commented: “Relative risk is not what decision-taking requires … relative risk is only for researchers; decisions call for absolute measures.” p. 19, Strategy of Preventive Medicine. Black – White Inequality in Infant Mortality 3 Relative Inequality 300 2 250 200 150 2.5 1.5 Black 1 100 50 White 0 1900 1910 1920 1930 1940 1950 1960 1970 1980 1990 0.5 0 Infant Mortality per 1,000 Infant Mortality per 1,000 350 400 Relative Disparity 400 200.0 180.0 160.0 140.0 120.0 350 300 250 200 Black 150 100 50 White Absolute Inequality 0 1900 1910 1920 1930 1940 1950 1960 1970 1980 1990 100.0 80.0 60.0 40.0 20.0 0.0 Abs olute Dis parity over the 20th Century, USA Age-specific Mortality Differences between the Richest and Poorest 20% of the World’s Population 100 Poorest 20% Mortality Rate per 1000 RR 9 80 7 60 5 40 Richest 20% 20 0 3 1 4 0- Gwatkin (2000) 14 5- 9 -2 5 1 4 -4 0 3 9 -5 5 4 9 -6 0 6 70 + RR • Explaining and reducing relative social gradients in CHD is a legitimate and important focus of research and intervention because it can help reveal novel CHD risk factors and mechanisms that are unevenly distributed across social groups. • However, explanations for relative social gradients need to be understood within the context of what causes most cases of CHD. Otherwise they may deflect attention from the most important population-level causes. • Rose – if everyone in the population smoked we would be finding that radon or asbestos were the most important causes of lung cancer • In populations where the prevalence of conventional risk factors is high, it is possible that there are no or small social gradients in those risk factors such that they cannot account for relative CHD differences across social groups but contribute substantially to the absolute risk of CHD in all social groups. • In the Whitehall Study there are small social differences in blood pressure and no social differences in total cholesterol • So reducing major, high prevalence risk factors from the population may have little effect on the relative social gradient but a large effect on the absolute social gradient as indicated by a reduction in the excess risk. • Importantly, this also means that whatever proximal (CRP) and distal factors (social capital) are identified as causes of the relative social gradient in CHD, if their behavioral and biological mechanisms do not involve conventional risk factors then they probably account for a small proportion of CHD cases. Social Inequality Control Depression Stress behaviours P-N-E Immune Function ? Traditional Risk Factors INTERHEART: PAR ~ 80% CHD Income Inequality, Poverty and Heart Disease: 1900-2000, USA 700 80 poverty income inequality heart disease 60 500 50 40 400 30 300 20 200 1900 1910 1920 1930 1940 1950 1960 1970 1980 1990 10 2000 gini coefficient/poverty rate per 100,000 600 70 Race-specific Voting Participation in Presidential Elections and age-adjusted, all-cause mortality, USA, 1968 - 1998 1,700.00 70.0 1,600.00 65.0 White Voting 1,400.00 60.0 1,300.00 Black Mortality 1,200.00 55.0 1,100.00 50.0 1,000.00 White Mortality Black Voting 900.00 % Voting in Presidential elections All-cause mortality per 100,000 1,500.00 45.0 800.00 700.00 40.0 1968 1970 1972 1974 1976 1978 1980 1982 1984 Year 1986 1988 1990 1992 1994 1996 1998 Lynch and Davey Smith (2003) Sex-Specific Smoking Trends and Heart Disease, 1900-1998, USA 800 3000 700 2500 2000 AADR 500 400 1500 300 1000 200 Male Smoking Female Heart Disease 500 Female Smoking 100 0 1900 0 1910 1920 1930 1940 1950 1960 1970 1980 1990 2000 Per Capita Consumption Male Heart Disease 600 Sex-Specific Smoking Trends and Income Inequality, 1900-1998, USA 100 3000 Male Smoking 90 2500 80 Income Inequality 2000 Female Smoking 60 Gini Per Capita Consumption 70 50 1500 40 1000 30 20 500 10 0 1900 1910 1920 1930 1940 1950 1960 1970 1980 1990 0 2000 Sex-Specific Cholesterol Trends and Income Inequality, 1980-2002, USA 47 5.6 46 5.5 45 5.4 44 43 Male Cholesterol 5.3 42 Gini 5.2 41 40 5.1 Female Cholesterol 39 5 38 37 4.9 1980 1985 1990 1995 2000 Total Cholesterol Trends from Minnesota Heart Survey: Arnett et al. Circulation (2005) Conclusion • We should re-affirm that smoking, hypertension, dyslipidemia and diabetes are the most important causes of CHD in populations and of social gradients in CHD. • If our concern is to reduce the overall population health burden of CHD and the population health burden of CHD inequalities, then reducing conventional risk factors will do the job. • Eliminating the social gradient in CHD attributable to non-traditional risk factor mechanisms will make a modest contribution to improving overall population health because the magnitude of the between social group CHD differences is small relative to the total risk variation in the population and to that due to traditional risk factors. Conclusion We should increase our efforts to find ways to influence the multiple pathways from international, national and local policy through to individual behaviour that will reduce conventional risk factors among current and future generations in richer and poorer countries. Individual and Population Level Causation Issues for PURE Black Africans 700 600 500 Coloured White CHD “Heart Disease” SEP 400 300 Risk Factors 200 All Stroke 100 SEP 0 ? Stress SEP INTERHEART Psychosocial – CHD CHD PAR ~ 30% Psychosocial Steyn, et al Circulation (2005) PURE Social, economic, demographic, behavioural transition Major Risk Factors Social Inequality CHD Psychosocial Factors Reporting Tendency Thank you Triangulating Epidemiology Populations Disease Trends Sub-groups Populations Individuals Sub-groups Biology Individuals Genetics Biology Disease Genetics Which social inequality is “better”? CHD Rate / 100K 1) Original population levels and social inequality in CHD 2) Social inequality and levels of CHD after reduction in social inequality and/or psychosocial causes? 3) Social inequality and levels of CHD after population-wide reductions in risk factors? Social Disadvantage Social Advantage Implications for Research on Human Growth and Development • in terms of CHD and probably many other diseases as well, we should focus on the developmental influences (political, economic, social, psychological, biological, genetic) on population levels and social inequalities in the major health behaviors in rich and poor countries Important to reiterate Geoffrey Rose • The causes of individual cases of CHD. The positive predictive value for individual risk prediction is very low because lots of people with conventional risk factors don’t get CHD – what makes people susceptible to the risk factors? Vs Risk of CHD and Lung Cancer by Smoking Status CHD (fatal or non-fatal) Lung Cancer Death Current or Former Smoker 172 / 1000 15 / 1000 Never Smoker 12 / 1000 0 Vs • The causes of population levels of CHD Almost all cases of CHD do have the conventional risk factors and so population levels almost completely accounted for 3-4 conventional risk factors Thus eliminating the risk factors eliminates the disease “If causes can be removed, then susceptibility ceases to matter” Geoffrey Rose Extensions 1. Understand why a relative social gradient (RR=1.6) remains even in a low risk population 2. Given the differential distribution of exposure to at least 1 risk factor across educational groups, is the exposure distribution enough to account for the greater disease burden generated among the low educated? Greater exposure or greater susceptibility? % exposed to 1+ High ed. 77 Mid ed. 84 Low ed. 89 CHD Risk per 1,000 65 15% 83 128 97% (1997)