Chapter 21- Respiratory
advertisement

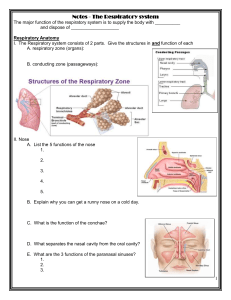
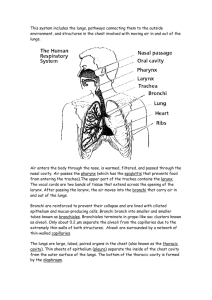
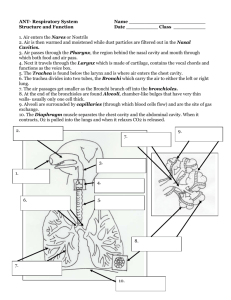
Respiratory System Chapter 21 Human Anatomy • One will die without oxygen in a matter of minutes. To avoid death the respiratory system brings oxygen into the body and the circulatory system delivers it to the tissues. The function of the respiratory system is to provide the body with oxygen and get rid of carbon dioxide. This system is also involved with vocalization and smell. • • • I. Functional Anatomy and Respiratory SystemWe will look at the components necessary for the four steps of respiration: 1. Pulmonary ventilation- Applying inhaling mechanisms to bring oxygen into the lungs • 2. External respiration- Transferring oxygen from the lungs to the blood and removing carbon dioxide from the blood so it enters the lungs. • 3. Transport of respiratory gases- Using the circulatory system to transport the oxygen to the tissues and to bring carbon dioxide to the lungs. • • 4. Internal respiration-exchange of oxygen from blood to tissue cells at the capillaries and of carbon dioxide from tissue cells to the blood. Structures of the respiratory system are divided into the respiratory zone (structures involved in gas exchange) and conducting zone (passage ways for air to travel to the lungs). • 5. Cellular respiration- the use of oxygen byt he cell’s mitochondria to metabolize nutrients for energy • Structures of the respiratory system are divided into respiratory zone (structures involved in gas exchange) and conducting zones (passage ways for air to travel to the lungs). • A. The nose and Paranasal SinusesThese two structures are within the conducting zone • 1. The nose- has three major functions: air treatment, voice resonance, and smell. It is divided into the external nose and nose cavity. • a. Nose functions: airway for respiration, warms, moistens, and filters the air, serves as a resonating chamber for speech, and contains the olfactory receptors for smell. • b. External nose: frontal bone (nose root) and nasal bone (nose bridge), sphenoid and ethmoid (nose roof), maxillary bones for the sides and hyaline cartilage forming the lateral, septal, and alar cartilage inferiorly (also see page 149 & 159). Dense connective tissue forms the inferior lateral side of the nostrils (external nares). Skin covers the surface of the external nose. • c. Nasal Cavity: formed by the inner side of the external nose and lies posterior to it. It is divided into left and right by the nasal septum (formed by: ethmoid bone, vomer, and septal cartilage). • When air first enters it passes through the external nares and the vestibule (area superior to nostrils). Air then enters the nasal cavity which contains nasal hairs to filter out small particles. The cavity continues into the nasopharynx via the internal nares (nasal conchae). The nasal cavity is lined with epithelial tissue that makes a mucus membrane called olfactory mucosa because it has smell receptors. All other mucus membranes that line respiratory structures are called respiratory mucosa. ). • The nose cavity also contains the superior, middle, and inferior nasal conchae. The conchae are spiral projections of bone and the meatus are grooves in between the conchae. As air rushes into the nose it moves through the conchae and this helps to increase its contact with mucus membranes which helps to trap particles in the air. The conchae also heat and moisten inhale air and reclaim heat and moisture from exhaled air. These structures also improve our sense of smell. •Respiratory mucosa is made up of pseudostratified ciliated columnar cells that also have goblet cells for mucus production and serous cells for production of liquid containing lysozyme. This forms a thin sheet of mucus that lines the respiratory tract trapping particles and moistening the air. The mucus traps particles and the cilia beat to gently move the mucus out of the respiratory tract. • 2. The paranasal Sinuses- mucosa lined air filled cavities that surround the nasal cavity and open into it. They are located in the maxillary, sphenoid, ethmoid, and frontal bone. They treat the air like the nasal cavity does and they drain into the nasal cavity. See page 163 and study disarticulated skulls in lab. • B. The pharynx- muscular passage way that connects the nasal cavity to the mouth and runs posterior to the mouth to connect to the larynx. It can be divided into three sections: • 1. Nasopharynx- cavity directly posterior to nasal cavity, it is lined with pseudo stratified ciliated columnar epithelium. During swallowing it is closed off by the soft palate and the uvula to prevent food from entering the nasal cavity. This area also contains the pharyngeal tonsils. • 2. Oropharynxlies posterior to the oral cavity and connects to it through the fauces, it runs from the soft palate to the epiglottis. It is lined with stratified squamous epithelium. When food is swallowed it passes through the oropharynx to enter the esophagus. This area also contains the palatine tonsils and the lingual tonsils. • 3. Laryngopharynxinferior to the oropharynx it is continuous with the esophagus and the larynx, thus it allows both food and air to pass by. It is lined with stratified squamous epithelium. • C. The larynx- small area also called the voice box that attaches to the hyoid bone, opens into the laryngopharynx, and ends at the trachea. It routes the air and food and produces one’s voice. It is composed of nine cartilage pieces, the largest is the thyroid cartilage. The thryroid cartilage has a ridge called the laryngeal prominence which is seen as the Adam’s apple. The larynx also contains the cricoid cartilage, and it has three other cartilages that anchor the vocal cords. The final cartilage piece is the epiglottis which helps to direct food and air into the correct passage way. • 1. Swallowing- when one swallows the larynx is pulled superiorly and the epiglottis covers the opening to the larynx thus food is steered into the esophagus. The position of the larynx is optimal for voice production but also increases the chances of choking. When food enters the larynx it stimulates the cough reflex and it can be released from this area. However, sometimes food moves in to the respiratory tract far enough to cause the person to choke to death. • 1. Voice production- The vocal cords are formed by ligament bands and are called true vocal cords, the space between is the rima glottidis and together they make up the glottis. Directly superior to these lies the false vocal cords which are mucosal folds not involved in sound production but enhance high frequency sounds. exhaled air make the cords vibrate and produce sounds, pitch is varied by tightening (high pitch- faster vibration) or loosening (low pitch-slower vibration) the vocal cords. Men have longer cords because of a large pharynx thus they vibrate slower and produce lower pitch sounds. Loudness depends on how fast air rushes through. Structures involved in voice resonance are the pharynx length, sinuses, and nasal cavity. The structures involved in shaping soud are the pharynx, tongue, soft palate, and lips enhance voice quality. Hoarseness is caused by inflammation of the vocal cords or interruption to normal innervation. • 2. Sphincter function of larynx- vocal cords can prevent passage of air thus no exhalation occurs. This is mostly activated when one contracts the abdominal muscle to increase abnominal pressure such as is needed when lifting and straining to defecate. • 3. Innervation of the larynx- the vagus nerve reaches the larynx and damage to it disrupts speech. The path of the nerves that reach the larynx runs below the apex of the lungs, lung cancer can compress the nerve and cause hoarseness. • D. The trachea- This structure is also known as the windpipe. It runs from the larynx to the bronchus. It has 16-20 C shaped cartilaged rings held together by fibroelastic connective tissue that prevents the trachea from collapsing. It is adjacent to the esophagus and the open “C” part faces the esophagus, it is lined with smooth muscle. The entire trachea is lined with pseudostratified ciliated columnar epithelium. The trachea can be divided into three layers: mucosa (inner epithlium), submucosa( goblet cells and serous cells), and adventitia (contains hyaline cartilage). At the carina the trachea branches into the bronchi. • E. The bronchi and subdivisions: the bronchial tree- The bronchi are extensions of the trachea that divide into left and right to enter the corresponding lung. As they branch they become more and more narrow. • 1. Bronchi in the conducting zone- The primary bronchus has the largest diameter and is the tube that first divides into left and right bronchus. The right is wider and shorter than the left. They enter the lungs at the hilus (medial depression). Once in the lungs the primary bronchi divide into secondary bronchi (lobar bronchi), three on the right and two of the left. The secondary bronchi divide into the tertiary bronchi (segmented bronchi) which continue to divide into more numerous but narrower branches. The bronchioles are the smallest and most narrow and do not contain cartilage. The terminal bronchioles are yet smaller, they end at the respiratory bronchioles. All aspect of the bronchi are lined with smooth muscle which constricts to reduce air flow or relaxes to increase air flow. As the branching continues the epithelial tissue also changes, as the bronchi branch the tissue it becomes thinner and is not ciliated. • 2. The respiratory zone- The conducting zone is made up by all the components tha carry the air into the lungs, the cite of gas exchange is the respiratory zone. At the end of the respiratory tree is the alveoli which makes up the lungs. The terminal bronchioles lead into the respiratory bronchioles which contain scattered alveoli the respiratory bronchioles end at the alveolar ducts that connect to the alveolar sacs ( a group of alveoli). Alveoli provide a large surface area for gas exchange, about 1500 square feet. • a. Alveolar structure: each alveolus is made up of a single squamous epithelial cell layer called Type I cells. They are in close contact with capillaries. The type I cell walls and the capillary cell walls together form the respiratory membrane. This thin membranes allows for diffusion of gasses to happen easily. The type II cells are cuboidal epithelial cells that are scattered throughout the Type I and release surfactant. This substance is a detergent-like material that prevents the alveiolar cells from sticking together. • b. Alveolar significant features: Alveoli are surrounded by elastic fibers. Alveolar pores connect adjacent alveoli to equalize pressure throughout the lung. Particles that managed to get to the lungs are removed by alveolar macrophages that circulate through air spaces (dust cells). • F. The lungs and pleurae: these are membranes that line the lungs and pleural cavity. • 1. The pleura- a serous membrance sac surrounds the lungs (pleura) within the pleural compartment; the heart, trachea, and primary bronchi lie within the medistinum. The parietal layer is on the outer surface and covers the entire surfaces of the thoracic cavity. The pleural cavity is a space between the parietal and visceral layer that is filled with pleural fluid, thus reducing friction and allowing the lungs to adhere to the thoracic wall. Close to the lung lies the visceral layer. • 2. Gross Anatomy of the lungs- the lungs are light, spongy, elastic organs that weight about 1.25 lbs. The walls of the lungs are in contact with the ribs. The lungs have an apex, a base, and a hilus at which the bronchi and pulmonary veins and arteries enter. The left lung has the cardiac notch in order to make room for the heart apex, it also has two lobes (upper and lower) separated by the oblique fissure. The right lung is larger and has three lobes (upper, middle, and lower) separated by the horizontal and oblique fissure. The lobes are further divided into bronchopulmonary segments (see page 597.) • 3. Blood supply and innervation- Pulmonary arteries lie posterior to the bronchi and branch in the same manner as the bronchi, they end at the pulmonary capillary networks the surround the alveoli. Oxygenated blood is carried by the pulmonary veins which lie anterior to the bronchi. Lung tissuehas its own blood supply that drains into bronchial arteries and veins. The nerves that control lung activity make up the pulmonary plexus. The sympathetic division dilates tubes, the parasympathetic division constrict tubes, and visceral sensory fibers send signals about sensation in the lungs. Anterior view of lungs Medial view of lungs • II. Ventilation • This includes the mechanism for breathing and how it is regulated by the brain. • A. The mechanism of ventilation- breathing consist of two phases and involves the intercostals muscles and the diaphragm. • 1. Inspiration: to inhale the volume of the thoracic cavity is increased by expanding it causing the pressure within it to drop. Contraction of the diaphragm (“flattens” the diaphragm/moves inferior) and external intercostals (raise the ribs) increases the cavity size. As the pressure decreases air rushes in to fill the lungs. • 2. Expiration: a normal exhale results from the reverse process of inspiration and occurs just by allowing the diaphragm and the intercostals muscles to relax. When the size of the cavity decreases pressure increases and air rushes out of the lungs. In forceful exhaling some abdominal and back muscles are contracted to create more pressure. • B. Neural control of ventilation- respiration is controlled in the medulla oblongata, the rhythum can be influenced by emotions or by chemoreceptors in the medulla or aortic bodies that sense a drop of oxygen in the blood • III. Disroders of the respiratory system-read on your own and ask questions in lecture. Go over the section on lung cancer (pg 60-605) Healthy Lung Emphysema Lung Cancer