The Role of Social Support in Reducing Psychological Distress
advertisement

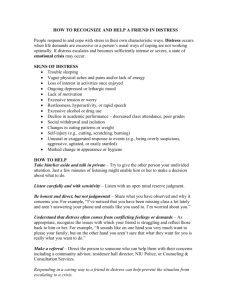
Canadian Institute for Health Information 1 The Role of Social Support in Reducing Psychological Distress 2 What Is Distress? • Psychological distress (distress) – A non-specific negative state of mental health that includes feelings associated with both depression and anxiety1 • Distress involves – A perceived inability to cope effectively, change in emotion, discomfort, communication of discomfort and temporary or permanent harm to the individual as a result2 3 What Is Known About • How distress affects health? – Living with distress is associated with developing other mental health conditions3, 4 – Distress is also associated with increased risk of chronic and severe physical illness5–8 • Who is more likely to experience distress? – An elevated distress level or greater risk of the onset of distress is more common among women, those with low income or lower levels of education, unemployed populations and people with compromised physical health9–12 • What can help distress improve? – Research consistently shows that social support is a protective factor against being or becoming distressed; however, evidence on the role of social support in reducing distress is lacking 4 What This Study Adds • Highlights an analysis of population-based data and demonstrates how social support can contribute to improvements in people’s experience of distress – The role of social support depends on whether structures or functions of support are considered, as well as which populations are studied • Presents examples of interventions that can influence distress and other mental health issues through social support–related activities 5 Methods • Data Source: National Population Health Survey (NPHS) • Analyses are based on Canadians age 18 and older who reported high distress at the start of any two-year cycle and had a distress score at follow-up two years later, over the decade beginning in 1998–1999 • 2,440 pairs of pooled observations: 1,660 reports by females and 780 by males • Logistic regression analysis was used to assess the factors associated with reporting a transition from high distress to low distress two years later 6 Methods (cont’d) • Distress was measured using a six-item scale (K6)3 – Respondents were asked whether in the past month they felt sad, nervous, restless or fidgety, hopeless, worthless or that everything was an effort • The Medical Outcomes Study (MOS) was used to assess social support3, 13 • Types of support – Positive interaction: for example, someone to have a good time with, to get together with for relaxation – Affectionate support: for example, having someone to hug you and make you feel wanted – Emotional support: for example, having someone to give you advice or suggestions, to share your private worries with 7 Results • There was no significant difference between men and women in reporting improvements in distress • Supports were significant in predicting transitions out of distress, even after taking into account such factors as being in a lower-income population or having a physical health limitation • Structures of social support—like being married— and functions of support—like having someone to provide emotional support—were linked to transitions out of distress • The relationship between social support and distress differed for women and men 8 Factors Predicting Transition • Women who reported having regular social interactions and the ability to talk with or confide in someone were more likely to transition out of distress – Women without those social supports were less likely to transition out of distress • For men in states of high distress, the structure of relationships (for example, marriage) was important in transitions out of distress – Being married was not protective for women 9 Factors Predicting Transition From High to Low Distress Two Years Later Restricted Physical Activity (vs. No Restriction) – Middle Income (vs. Lower) + High Income (vs. Lower) + – Affection Support (High vs. Lower) Positive Interaction (High vs. Lower) + Emotional Support (High vs. Lower) + Married/Common-Law (vs. Widowed/Separated/Divorced) – + Single (vs. Widowed/Separated/Divorced) Notes + More likely to transition. – Less likely to transition. Source CIHI Analysis of National Population Health Survey, 1998–1999 to 2008–2009, Statistics Canada. 10 What Is It About Social Support? • Women who felt they had opportunities for the social support components all or most of the time were significantly more likely to report improved distress two years later than women who reported having the selected support component less often • No single question was clearly linked with later improvements in distress among men • The only item not significant for women (someone to have a good time with) was the only question that approached significance for men (p = 0.06) 11 How Does Distress Improve if You Have Someone to . . . Do Something Enjoyable With * Confide in or Talk to About Yourself or Your Problems * Share Your Most Private Worries and Fears With * Do Things With to Help Get Your Mind off Things * Get Together With for Relaxation * Count on to Listen to You When You Need to Talk * Turn to for Suggestions About How to Deal With a Problem * Give You Information to Help You Understand a Situation * Understand Your Problems * Give You Advice About a Crisis * Give Advice * Have a Good Time With 0.0 0.2 0.4 0.6 0.8 1.0 1.2 1.4 1.6 1.8 Odds of Experiencing Improvement in Distress Based on Perceptions of Having the Specified Support Available All or Most of the Time if Needed Males 2.0 Females Note * Indicates support questions that are significantly associated with experiencing improvements in distress in the full model compared with having the supports less than all or most of the time, after adjusting for age, marital status, income, employment, activity restriction and consulting on mental health (p<0.05). Source CIHI Analysis of National Population Health Survey, 1998–1999 to 2008–2009, Statistics Canada. 12 Conclusion: What We Know • Analyses showed that the role of social support in predicting improvements in distress differed based on the type of support and the sex of the population • Successful interventions can influence distress and other mental health issues through social support; effective approaches include – Focusing on individuals’ skills at relating – Providing opportunities for interaction • In some cases, interventions can be integrated with existing health services 13 Conclusion: What We Still Don’t Know • Opportunities exist for building better evidence on social support and distress by – Measuring different dimensions of support where possible – Considering sex and gender differences in population, clinical or evaluation studies • The impact of income source and changes in income on improvements in mental health may be avenues for future research 14 References 1. B. P. Dohrenwend et al., “Nonspecific Psychological Distress and Other Dimensions of Psychopathology: Measures for Use in the General Population,” Archives of General Psychiatry 37, 11 (1980): pp. 1229–1236. 2. S. H. Ridner, “Psychological Distress: Concept Analysis,” Journal of Advanced Nursing 45, 5 (2004): pp. 536–545. 3. R. C. Kessler et al., “Short Screening Scales to Monitor Population Prevalences and Trends in Non-Specific Psychological Distress,” Psychological Medicine 32, 6 (2002): pp. 959–976. 4. J. Cairney et al., “Evaluation of 2 Measures of Psychological Distress as Screeners for Depression in the General Population,” The Canadian Journal of Psychiatry 52, 2 (2007): pp. 111–120. 5. P. J. Puustinen et al., “Psychological Distress Predicts the Development of the Metabolic Syndrome: A Prospective Population-Based Study,” Psychosomatic Medicine 73, 2 (2011): pp. 158–165. 6. J. Caron and A. Liu, “A Descriptive Study of the Prevalence of Psychological Distress and Mental Disorders in the Canadian Population: Comparison Between Low-Income and Non-Low-Income Populations,” Chronic Diseases in Canada 30, 3 (2010): pp. 84–94. 7. S. A. Stansfeld et al., “Psychological Distress as a Risk Factor for Coronary Heart Disease in the Whitehall II Study,” International Journal of Epidemiology 31, 1 (2002): pp. 248–255. 15 References (cont’d) 8. F. Rasul et al., “Psychological Distress, Physical Illness, and Risk of Coronary Heart Disease,” Journal of Epidemiology & Community Health 59, 2 (2005): pp. 140–145. 9. T. Stephens, C. Dulburg and N. Joubert, “Mental Health of the Canadian Population: A Comprehensive Analysis,” Chronic Diseases in Canada 20, 3 (1999): pp. 118–126. 10. J. Caron and A. Liu, “Factors Associated With Psychological Distress in the Canadian Population: A Comparison of Low-Income and Non-Low-Income Sub-Groups,” Community Mental Health Journal 47, 3 (2010): pp. 318–330. 11. A. Marchand and M. E. Blanc, “The Contribution of Work and Non-Work Factors to the Onset of Psychological Distress: An Eight-Year Prospective Study of a Representative Sample of Employees in Canada,” Journal of Occupational Health 52, 3 (2010): pp. 176–185. 12. H. Orpana, L. Lemyre and R. Gravel, “Income and Psychological Distress: The Role of the Social Environment,” Heath Reports 20, 1 (2009): pp. 1–9. 13. C. D. Sherbourne and A. L. Stewart, “The MOS Social Support Survey,” Social Science & Medicine 32, 6 (1991): pp. 705–714. 16 Peer Reviewers • Heather Orpana, PhD, Senior Research Analyst, Public Health Agency of Canada • Mike O’Shea, Mental Health Lead, North East Local Health Integration Network, a representative on the CCIM—CAP-MH Advisory Group 17 About Us 18 About the Canadian Institute for Health Information (CIHI) • Established in 1994 as independent, not-for-profit corporation • Vision: Better data. Better decisions. Healthier Canadians. • Mandate: To lead the development and maintenance of comprehensive and integrated health information that enables sound policy and effective health system management that improve health and health care • Data holdings: 27 databases of health information • Range of stakeholders in health system and beyond – Government organizations (for example, Health Canada, Statistics Canada), ministries of health, regional health authorities, non-government organizations, private-sector organizations, professional associations, health facilities 19 About the Canadian Population Health Initiative (CPHI) • CPHI is a branch within CIHI • CPHI’s mission: To support policy-makers and health system managers in Canada in their efforts to improve population health and reduce health inequalities through research and analysis, evidence synthesis and performance measurement • Work is guided by the CPHI Council, which includes representatives from government organizations, regional health authorities, and research and academic institutes 20 Thank You! 21