Web Case Study - Leah Fite BSN, RN, CCRN
advertisement

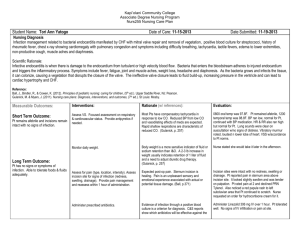
Running head: WEB CASE STUDY 1 Web Case Study Leah Fite Wright State University WEB CASE STUDY 2 Focused History and Physical Source Patient is pharmacologically sedated. Recently discharged pt, so medical records are the most reliable source. The patient’s healthcare power of attorney (POA), a friend of the patient, is at the bedside, and may not be very reliable. Chief Complaint “Vomiting, diarrhea, fever and weakness that started early this morning.” History of Present Illness V.S. is a 47 year old female who presents to the emergency department via ambulance with acute onset of vomiting, diarrhea, malaise and fever. She denies chest pain, shortness of breath, and abdominal pain. She is on immunosuppressive therapy (prednisone and mycophenolate mofetil) for her recent kidney transplant. Her abdomen is soft with a recent surgical incision with evident bruising, but no drainage or erythema noted. She complains of significant pain at this incision 10/10, unable to describe the quality. Yesterday, she was discharged from the hospital following cadaveric renal transplant with subsequent antibody mediated rejection (AMR). The AMR was treated with plasmapheresis, velcade and rituximab on post operative day six, and was well tolerated. Upon discharge, she was feeling fine, creating urine, and had no signs or symptoms of infection. She denies any contact with anyone ill since discharge home. Initially in the ED, pt was alert and oriented, hemodynamically stable, with no evident distress. However, within two hours of her care, she acutely decompensated, requiring increasing oxygen and multiple fluid boluses to maintain adequate perfusion. The transplant WEB CASE STUDY 3 team was notified of her arrival and current condition and she was transferred to the intensive care unit. Upon admission to the ICU the patient further decompensated requiring intubation and mechanical ventilation. High dose vasopressors were initiated and multiple fluid boluses were given to improve hemodynamic instability. The advanced practice nurse (APN) ordered labs, blood and urine cultures, chest x-ray, and 12-lead EKG. A bedside echo was performed by the APN to evaluate cardiac function. A computerized tomography (CT) of the abdomen was ordered but unable to be complete due to the instability of the patient. Within hours of admission to the ICU, the wound ecchymosis had doubled in area and subcutaneous emphysema had developed around the incision. Past Medical History End Stage Renal Disease (ESRD) secondary to diabetes mellitus (DM), hemodialysis three days/week x one year, hypertension, obesity, urinary tract infection with recent treatment of ciprofloxacin. Past Surgical History Cholecystectomy 2010, Cadaveric kidney transplant April 2012 Family History Mother deceased secondary to myocardial infarction. Unknown history regarding father due to estrangement. No siblings or children. Social History WEB CASE STUDY 47 year old female who lives alone. She is a retired customer service clerk, who quit working full time after developing renal failure requiring hemodialysis. Denies smoking, drinking, and illicit drug use. For exercise, she rides a stationary bike daily for 30 minutes, and enjoys taking her puppy outside for play. The patient has been eating a more “healthy” diet since before receiving her kidney transplant. She denies being around anyone who is ill. She also denies being in a relationship or any recent sexual activity. Allergies Vancomycin-rash Medications Amaryl 3mg PO daily Lantus 35 units subcutaneous daily Metoprolol Tartrate 25mg PO twice a day Norvasc 10mg PO daily Mycophenolate Mofetil 1000mg PO twice a day Prednisone 20mg PO daily Review of Systems General: Prior to intubation, pt reports fever, malaise, and nausea. Height 5’6”, current weight 178 lbs 4 WEB CASE STUDY Neurological: Pharmacologically sedated. Previously reported alert and oriented, with complaints of generalized weakness and lethargy. HEENT: Unable to obtain. Skin: Unable to obtain. CV: Prior to intubation, denied chest pain or palpitations Respiratory: Prior to intubation, denied cough, wheezing, or shortness of breath Abdomen: Prior to intubation, complaints of nausea, vomiting, and diarrhea. Also had complaints of increasing abdominal pain, 10/10 unable to describe the quality, with nothing making it better or providing relief. M/S: Prior to intubation, complaints of generalized weakness, but denied muscle and joint pain. Physical Examination Vital Signs: Temperature 102 degrees Fahrenheit, HR 120 beats per minute (bpm), BP 94/57 (on pressors), RR 16 breaths/min (on ventilator), Oxygen saturation 99% General: Pharmacologically sedated well nourished, well developed caucasion female. Neurological: Pharmacologicallly sedated with propofol and fentanyl. Opens eyes to name. Able to weakly follow commands. RASS -2. HEENT: Head is midline and normocephalic. Atraumatic. No masses or lesions palpated. Sclera white, conjunctiva pink, no hemorrhages or exudates noted. Pupils 4mm, 5 WEB CASE STUDY 6 constricting to 3mm, and equal and reactive to light and accommodation. Bilateral tympanic membranes pearly gray. Nasal mucosa pink and moist with no exudates. Dentition in good health. Trachea midline and thyroid smooth, without nodules. No lymphadenopathy. Unable to view throat due to presence of endotracheal tube. Skin: Skin is pale, hot, and dry. Non-tenting skin. Nails without cyanosis. Recent surgical incision with significant ecchymosis that has grown in size over the past several hours. Subcutaneous emphysema noted around the incision. Otherwise no rashes or erythema noted. CV: Apical pulse palpated at fifth intercostal space, six centimeters lateral to midsternal line. Tachycardic on monitor at 120 beats/min. S1 and S2 normal without S3 or S4, no murmurs, rubs, or gallops noted. No jugular venous distention noted. 1+ bilateral lower extremity edema noted. Pulses 2+ bilaterally, radial, brachial, posterior tibial, and dorsalis pedis. Respiratory: Intubated and mechanically ventilated. Lung expansion symmetric. Respiratory effort regular and unlabored on ventilator. Diffuse rhonchi auscultated in all lung fields. Resonance over majority of lung fields with percussion. Dullness to percussion noted bilateral lower lung fields. Abdomen: Active bowel sounds in four quadrants. Soft, non-distended, but firm 2cm around incision. + grimace to palpation around healing surgical incision. Guarding noted with deep palpation. No hepatosplenomegaly or palpable masses. Subcutaneous emphysema and ecchymosis around incision. WEB CASE STUDY M/S: 7 No erythema, warmth, or crepitus noted on extremeties. Unable to fully assess muscle strength or range of motion due to current patient condition. Laboratory Findings Tissue pathology obtained during surgical exploration and debridement remains the standard for diagnosis of necrotizing fasciitis (Stevens et al., 2005). To further distinguish necrotizing fasciitis (NF) from other soft tissue infections, the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) uses an objective scoring system based on standard lab testing including total white blood cell count (WBC), hemoglobin, sodium, creatinine, glucose, and Creactive protein (Wong, Khin, Heng, Tan, & Low, 2004) (See Appedix A for LRINEC). Each lab value is given a point, which is added to a total. A point value of 6-7 indicates an intermediate risk for NF, while 8 points or more indicate a high risk of NF (Wong et. al, 2004). Due to the rapid progression of disease, and the immunocompromised status in this patient, initial treatment should not be delayed. According to the lab values, this patient presents with a LRINEC of 9. Table 1. Complete Blood Count, Coagulation, and Renal Panel Complete Blood Count WBC Results 2.8 cells/mL RBC 2.23 cells/mL Hemoglobin 8.8 g/dL Hematocrit 25.7% Normal Values 3.8-10.8 Kcells/mL 3.8-5.10 cells/mL 11.7-15.5 g/dL 35.0-45.0% MCV 79.0 fL 80.0-100.0 fL Renal Panel Results Sodium 140 mmol/L Potassium 3.7 mmol/L Chloride 101 mmol/L Carbon Dioxide BUN 20 mmol/L 140 mg/dL Normal Values 135-146 mmol/L 3.5-5.3 mmol/L 98-110 mmol/L 21-23 mmol/L 7-25 mg/dL WEB CASE STUDY 8 MCH 26.0 pg/cell MCHC 31.0 g/dL RDW 11.0% 27.0-33.0 pg/cell 32.0-36.0 g/dL 11.0-15.0% Creatinine 8.8 mg/dL Glucose 187 mg/dL Calcium 10.0 mg/dL 0.50-1.20 mg/dL 65-99 mg/dL Platelet 82 K/uL 140-400 K/uL Phosphorus 5.0 mg/dL 8.6-10.2 mg/dL 2.5-4.5 mg/dL MPV 7.9 fL 7.5-11.5 fL Magnesium 2.1 mg/dL 1.5-2.5 mg/dL Neutrophils Relative Bands Relative Lymphocytes Relative Monocytes Relative nRBC 46% 40.0-80.0% Albumin 2.9 g/dL 3.6-5.1 g/dL 44% 0.0-9.0% Total protein 5.8 g/dL 6.2-8.3 g/dL 5% 15.0-45.0% PT 20.8 seconds 5% 0.0-12.0% INR 1.9 11.6-14.4 seconds 0.9-1.1 1 0.0/100 WBC PTT 42.5 seconds 25-35 seconds Neutrophils Absolute Lymphocytes Absolute Monocytes Absolute Bands Absolute 1288 /uL 1500-7800/uL 140 /uL 850-3900/uL 140/uL 200-950/uL 1232/uL 0-750/uL Table 2. Arterial Blood Gas and Other Laboratory Findings Arterial Blood Gas (ABG) Results Normal Values pH 7.26 7.35-7.45 pCO2 pO2 45 mmHg 76 mmHg HCO3 18 mmol/L CO2 content 17.5 mmol/L 35-45mmHg 80100mmHg 2226mmol/L 23-27 mmol/L Other Laboratory Findings Alkaline Phosphatase CRP Lactic Acid Results Normal Values 62 U/L 40-115 U/L 21.2 mg/dL 6.5 mmol/L AST 23 U/L <0.8 mg/dL 0.5-2.2 mmol/L 14-65 U/L ALT 65 U/L 13-69 U/L WEB CASE STUDY Base Excess 9 -12.5 -2.0-3.0 Carboxyhemoglobin 1.2 Unknown Methoglobin Reduced Hemoglobin %HBO2 0.4% 1.2% 0.0-1.5% 0.0-5.0% 95.5% 95.0-98.0% Direct Bilirubin Total Bilirubin ESR 0.1 mg/dL 0.4 mg/dL 42 mm/hr 0.0-0.2 mg/dL 0.2-1.2 mg/dL <15mm/hr Diagnostic Data 12-lead EKG reveals sinus tachycardia with left axis deviation. Ventricular rate is 120 bpm, with no Q waves or ST abnormalities. Chest xray shows no evidence of pulmonary edema, however small bilateral pleural effusions are noted. CT of chest, abdomen and pelvis was unable to be completed due to instability of patient. Bedside echo shows increased wall thickness in a pattern of mild left ventricular hypertrophy (LVH), with no regional wall abnormality. Mitral valve with mildly calcified annulus and mildly thickened leaflets. Ejection fraction (EF) is 55%. Urine culture shows no growth. No growth to date from blood cultures. Differential Diagnoses The presenting symptoms of fever, pain, and rapid deterioration in the recently discharged immunocompromised patient with surgical incision lead to differential diagnoses of gangrenous cellulitis, abscess, necrotizing fasciitis (NF), and infectious myositis (Lipworth, Saavedra, Weinberg, & Johnson, 2012). Given that the patient had diarrhea, fever, and bandemia, acute infection of Clostridium difficile should be ruled out. Immunocompromised patients are at high risk for acquiring infections, which can cause life-threatening complications in this population. Clinical assessment and early recognition of the severity of infection is important, especially in this patient, to decrease the incidence of mortality. WEB CASE STUDY 10 Systemic toxicity as presented by fever, tachycardia, hypotension and renal failure are clinical signs that accompany soft tissue infection (Stevens et. al, 2005). Initial signs of skin inflammation, such as pain, edema, and erythema may be present in less serious conditions such as cellulitis, but pain disproportionate to the degree of inflammation, firm tissue around incision, and skin ecchymosis are hallmark signs of NF (Anaya & Dellinger, 2007). Violaceous bullae, cutaneous hemorrhage or ecchymosis, skin sloughing, skin anesthesia, rapid progression, and gas in the tissue are other clues to deep soft-tissue infection (Stevens et al., 2005). Necrotizing fasciitis is the likely diagnosis for this patient. She presents with systemic toxicity, pain consistent with diagnosis, and ecchymosis at the site of recent surgery with subsequent crepitus at and around the incision. Immunosuppressive drug therapy, recent surgery, and diabetes also led to susceptibility and vulnerability of this infection (Anaya & Dellinger, 2007). Plan Clinical guidelines for the management and treatment of NF are currently being updated, but the recommendations are consistent in that to achieve optimal outcomes, aggressive and timely resuscitation, prompt and appropriate administration of antibiotic therapy, and early surgical debridement are required to decrease mortality (May et al., 2009). NF may be monomicrobial or polymicrobial, involving both aerobic and anaerobic bacterial flora (Stevens et al., 2005). Polymicrobial infections are most common, especially in immunocompromised individuals (Anaya & Dellinger, 2007), therefore treatment must include therapies efficient against both aerobes and anaerobes. WEB CASE STUDY 11 Initiation of appropriate antibiotic therapy should depend on medical history and allergies of the patient, as well as suspected pathogens and progression of the infection. Broad spectrum antibiotics are indicated to cover aerobic and anaerobic gram-negative and gram-positive pathogens, as well as resistant gram-positive bacteria such as MRSA, especially in the immunocompromised patient experiencing toxicity (Stevens et al., 2005). The antibiotic regimen to be initiated in this patient will be Piperacillin-tazobactam (3.375g I.V. over 4 hours, every 12 hours, for 7-14 days), Clindamycin (600mg I.V. every 8 hours, for 10-14 days), and Linezolid (600mg I.V., every 12 hours, for 10-14 days). Complete debridement of the infected tissue and early empiric broad spectrum antibiotic coverage allow for future recovery in the patient with NF (Anaya & Dellinger, 2007). In addition to these interventions and close monitoring, further treatments are indicated. These treatments include adequate organ support, aggressive fluid resuscitation, tight glycemic control, and transfusion of appropriate blood products (Anaya & Dellinger, 2007). When appropriate, enteral nutritional support should be started to increase wound healing and control catabolic response (Anaya & Dellinger, 2007). Drug Therapy Drug and Dose Drug to Drug Interactions Piperacillintazobactam (Zosyn) Increased Effect/Toxicity: Floxacillin, Methotrexate, Vecuronium, Vitamin K Antagonists Decreased Effect: Aminoglycosides, BCG, 2.25g/50mL 3.375g/50mL 4.5g/100mL Adverse Effects/Precaution s Adverse Effects: Insomnia, headache, fever, agitation, pain, anxiety, hypertension, chest pain, edema, diarrhea, constipation, nausea, vomiting, Follow-up Monitoring Cost CBC with differential, BUN, Creatinine, Coags, serum electrolytes, LFTs. Monitor for signs of anaphylaxis with initial dose. Zosyn (per dose) 2.25g/50m L: $18.31 3.375g/50 mL: $27.47 WEB CASE STUDY 12 Mycophenolate, Sodium Picosulfate, Typhoid Vaccine Levels of Piperacillin/tazobac tam may be decreased by Tetracycline Derivatives Clindamycin (Cleocin) Cleocin in D5W: 300mg/50mL 600mg/50mL 900mg/50mL dyspepsia, rash, pruritis, increased AST, local reaction at site of injection, pharyngitis, dyspnea, moniliasis Precautions: Use with caution in patients with renal impairment. Dose adjustments are recommended. Use with caution in patients with a history of seizure disorder; high levels may increase risk of seizure. Avoid concomitant Adverse Effects: use with BCG and Cardiac arrest Erythromycin (rare), hypotension Increased (rare), StevensEffect/Toxicity: Johnson Syndrom Neuromuscular(rare), erythema Blocking Agents. multiforme (rare), Decreased Effect: pruritis, rash, BCG, Erythromycin, urticaria, Sodium Picosulfate, abdominal pain, Typhoid Vaccine. diarrhea, Levels/effects of esophagitis, Clindamycin may be nausea, vomiting, decreased by pseudomembrane Kaolin. colitis, agranulocytosis, eosinophilia (transient), neutropenia (transient), thrombocytopenia, jaundice, abnormal LFTs, thrombophlebitis at injection site, Precautions: Use with caution in patients with 4.5g/100m L: $34.81 CBC, renal function, and hepatic enzymes. Observe for changes in bowel frequency and monitor for colitis. Cleocin in D5W (per dose) 300mg/50 mL: $11.89 600mg/50 mL: $18.20 900mg/50 mL: $22.24 WEB CASE STUDY Linezolid (Zyvox) 600mg/300mL 13 hepatic impairment. Dosage adjustments may be necessary based on hepatic enzymes Increased Adverse Effects: Effect/Toxicity: Insomnia, Antihypertensives, dizziness, Antipsychotics, headache, nausea, Apraclonidine, diarrhea, vomiting, Atomoxetine, Beta2- increased serum Agonists, lipase, increased Betahistine, ALT and AST, Bezafibrate, increased serum Brimonidine, bilirubin, rash, Bupropion, increased BUN and Clozapine, creatinine Dexmethylphenidate Precautions: Use , Dextromethorphan, in caution with Diethylpropion, patients with Domperidone, cardiovascular Doxapram, disease due to the Doxylamine, mild MAO Epinephrine, inhibitor Hydrocodone, properties. Avoid Hydromorphone, use with Hypoglycemic sympathomimetic Agents, and dopaminergic Isometheptene, agents. May cause Levondordefrin, thrombocytopenia Lithium, (use caution in Meperidine, patients with Methadone, thrombocytopenia). Methyldopa, Methylene Blue, Methylphenidate, Metoclopramide, Mertazapine, Morphine, Nefazodone, Norepinephrine, Oxycodone, Pizotifen, Reserpine, SSRIs, Serotonin 5HT1D Receptor CBC and platelet count, especially in patients at risk for bleeding. Monitor for myelosuppression (anemia, leukopenia, pancytopenia, and thrombocytopenia) in patients receiving Linezolid for >2 weeks. Zyvox I.V. (per dose) 600mg/300 mL: $216.54 Zyvox tablets (20) 600mg: $2807.52 WEB CASE STUDY 14 Agonists, Serotonin Modulators, SerotoninNorepinephrine Reuptake Inhibitors, Sympathomimetics, Trazodone, Tricyclic Antidepressants Levels/Effects of Linezolid may be increased by: Altretamine, Anilidopiperidine, Buspirone, Carbamazepine, COMT inhibitors, Cyclobenzaprine, Levadopa, MAO Inhibitors, Maprotiline, Oxymorphone, Tapentadol, Tetrabenazine, Tramadol, Tryptophan Decreased Effect: Domperidone Drug information retrieved from Lexicomp 2014 Advanced Practice Nurse (APN) Authority to Prescribe APNs who hold a current certificate to prescribe (CTP) in the state of Ohio may prescribe many drugs that fall within their scope of practice, unless there are listed exclusions or additional parameters specified within the formulary (Ohio Board of Nursing, 2014). In this case, according to the formulary by the Ohio Board of Nursing (2014), the APN has the authority to prescribe Clindamycin and Piperacillin-tazobactam without physician collaboration. Prescribing Linezolid, however, requires the APN with a CTP to have prescribing designation addressed in the standard care arrangement with the collaborating physician(s) in order to initiate treatment WEB CASE STUDY 15 (Ohio Board of Nursing, 2014). Due to the complexity of the patient’s history and current status, collaboration with a physician specializing in infectious disease would be most beneficial for optimal outcomes. Clinical Studies Current guidelines recommend several antibiotics for the treatment of polymicrobial necrotizing fasciitis (Stevens et al., 2005). No current literature supports recommendations of one regimen over another in severe infections with NF (May et al., 2009). With the increase in incidence over the past decade of antibiotic resistance gram-positive cocci (MRSA), especially in the immunocompromised patient, additional antibiotics must be considered (Yue, Dong, Yang, Chen, Wu, & Liu, 2013). Vancomycin and Linezolid are commonly used in the treatment of MRSA complicated skin and soft tissue infections (SSTIs) (Yue et al., 2013). A Cochrane Review of nine randomized control trials (RCTs) was conducted to evaluate and compare the treatment of SSTIs with Linezolid and Vancomycin (Yue et al., 2013). 3114 participants of the 4496 were diagnosed with SSTI; five trials enrolled people with MRSA, while the other four trials enrolled those with gram-positive bacterial infection; eight of the nine RCTs included adults age greater than 18 (Yue et al., 2013). In all trials with adult participants, doses of the drugs were similar, in that Linezolid 600mg I.V. administered every 12 hours, and Vancomycin 1000mg I.V. every 12 hours, with the exception of one RCT where participants were randomized to receive oral or I.V. Linezolid 600mg every 12 hours, or Vancomycin 15mg/kg every 12 hours (Yue et al., 2013). Investigators evaluated the clinical cure, microbiological cure, SSTI-related mortality, and treatment-related mortality, with secondary evaluation of adverse events, duration of hospital WEB CASE STUDY 16 stay, duration of treatment, and cost (Yue et al., 2013). In participants with suspected or proven MRSA infection (2659 participants), clinical cure (resolution of signs and symptoms) was evaluated, while in those with confirmed MRSA at baseline (1289 participants), microbiological cure (elimination of bacteria on wound culture) was evaluated. Linezolid was proven to have statistically significant clinical and microbiological cure rate when compared to Vancomycin (Yue et al., 2013). Other outcomes which were evaluated showed no significant difference in mortality between the two groups with SSTI. Linezolid participants showed lower incidence of red man syndrome, pruritis, and rash, but was also associated with increased incidence of thrombocytopenia and nausea. Inpatient treatment cost of Linezolid was higher than inpatient treatment cost of Vancomycin, however, the length of hospital stay was three days shorter, proving that the total cost of treatment with Linezolid is less than that of Vancomycin (Yue et al., 2013). Several limitations with the RCTs used in this Cochrane review were addressed. First, although the studies included were randomized, none of the studies mentioned the method of randomization. In the majority of the studies reviewed, the treatment allocation was not concealed, which may lead to an overestimation of treatment effect. Also, in seven of the nine RCTs, it was not reported, or is unclear of the dropout rate of the studies, which can cause problems with false-positives or negatives regarding the data. Lastly, all of the trials reviewed were funded by the pharmaceutical company which manufactures Linezolid, leading to biased publication and a potential miscalculation of the effects of Linezolid (Yue et al., 2013). WEB CASE STUDY 17 Issues Several considerations are necessary when developing the plan of treatment in this patient. This patient was recently discharged status post kidney transplant, has a listed allergy to vancomycin, and was admitted with a serum creatinine of 8.8mg/dL. Thorough evaluation of the patient, including medical and social history, along with complex physical assessment and progression of infection will aid the APN to the appropriate treatment. Although anti-rejection drugs and corticosteroids are indicated for all solid organ transplants, in the case of severe infection such as this, all anti-rejection and immunosuppression medications should be stopped to allow for adequate immune response to fight the infection. Collaboration between the APN and the transplant team would be necessary to determine when to restart this therapy based on patient status. Based on the patient weight and admitting serum creatinine, the creatinine clearance of this patient is 7.8 mL/min (Mdcalc, 2014). According to this calculation, dosage adjustment for the Piperacillin-tazobactam must be made to ensure no further renal injury occurs. Current guidelines recommend treating SSTI with 3.375g I.V. every 6-8 hours, however, with this patients renal impairment, extended infusion dosing of 3.375g I.V. over 4 hours every 12 hours is safe and effective (Lexicomp, 2014). This patient also has a listed allergy to Vancomycin, which is the first line treatment for MRSA-associated NF. Given this allergy, Linezolid or Daptomycin would otherwise be considered. Since this patient also has acute renal injury to the newly transplanted kidney, Daptomycin could be administered 4mg/kg I.V. every 48 hours, but should be avoided to decrease the risk of further renal injury due to its renal clearance (Lexicomp, 2014). Although WEB CASE STUDY 18 Linezolid has been shown to increase BUN and creatinine levels, it is not cleared renally, and no dosage adjustment is required in the patient with renal impairment. Linezolid does have thrombocytopenic side effects and the risk versus benefit should be considered in this patient who presents with an already decreased platelet count. Linezolid is also a better option due to the ability to change from I.V. therapy to oral therapy if the patient required further antibiotic treatment upon discharge. Drug to drug interactions should always be taken into consideration when prescribing medications. Since the immunosuppressive therapy in this patient will be stopped, the APN does not need to consider these drugs with interactions, but may need to when the patient has recovered from the infection, and it is time to restart those medications. Linezolid is the only current medication that may cause drug to drug interactions. This patient is requiring high doses of pressors upon admission to the ICU, and it is likely that she was receiving both norepinephrine and epinephrine for blood pressure support. Both of these medications may have increased effects/toxicity when used in combination with Linezolid, so dosage adjustments to those pressors may need to be made in accordance to patient response. This patient has rapidly deteriorated since admission, so education regarding treatment plan and economic concerns are of decreased importance until the patient recovers from the severe, life-threatening infection. Once recovery has been gained, patient education should include methods to prevent contraction of another opportunistic infection. If the patient requires antibiotics upon discharge, teaching regarding side effects and signs of infection should be considered. Economical considerations can be discussed at that time, with referral to drug assistance companies if needed. WEB CASE STUDY 19 Ethical and Legal Considerations When implementing a treatment plan, ethics must always be taken into consideration. Non-maleficence is being practiced in this patient by providing prompt treatment with surgical intervention and appropriate antibiotic therapy. It is the goal of the APN and healthcare team to do no harm. Beneficence is practiced by using the most up-to-date guidelines to treat this patient, however, there is a concern of risk versus benefit. This patient is severely immunocompromised with a complicated, life-threatening illness, so the APN must decide what would be best for the patient regarding continuing to treat. This patient has a lack of autonomy in her care since she is incapacitated due to medications and severity of the illness. It is up to her POA to decide what the patient would want, and may not feel comfortable in ending treatment if the APN and treatment team continue to provide additional “life-saving” therapies. With all instances of patient care and treatment, confidentiality and privacy must be maintained. Prior to initiating a treatment plan, it is essential to know and understand the Ohio Revised Code and Administrative code for APNs. Legal action for the APN may take place if adverse events occur as a result of failure to recognize contraindications, poor monitoring, or inadequate follow-up (Lawriter, 2013). WEB CASE STUDY 20 References Anaya, D., & Dellinger, P. (2007). Necrotizing soft-tissue infection: Diagnosis and management. Clinical Infectious Disease, 44, 705-710. doi: 10.1086/511638 Lawriter (2013). Administrative rules for prescribing drugs and therapeutic devices (Report no. 4723.50). Retrieved from Ohio laws and rules: http://codes.ohio.gov/orc/4723.50 Lexicomp, Inc. (2014). Lexi-Drugs. Retrieved from http://webstore.lexi.com/PDA-Softwarefor- Nurses Lipworth A.D., Saavedra A.P., Weinberg A.N., Johnson R (2012). Chapter 179. Necrotizing Soft Tissue Infections: Necrotizing Fasciitis, Gangrenous Cellulitis, and Myonecrosis. In Goldsmith L.A., Katz S.I., Gilchrest B.A., Paller A.S., Leffell D.J., Wolff K (Eds), Fitzpatrick's Dermatology in General Medicine, 8e. Retrieved February 06, 2014 from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bo okid=392&Sectionid=41138906. May, A., Stafford, R., Bulger, E., Heffernan, D., Guillamondegui, O., Bochicchio, G., & Eachempati, S. (2009). Treatment of complicated skin and soft tissue infections. Surgical Infections, 10(5), 467-499. doi: 10.1089/sur.2009.012 Mdcalc. (2014). Creatinine Clearance (Cockcroft-Gault Equation). Retrieved from http://www.mdcalc.com/creatinine-clearance-cockcroft-gault-equation/ WEB CASE STUDY 21 Ohio Board of Nursing (2014). The formulary developed by the Committee on Prescriptive Governance. Retrieved from http://www.nursing .ohio.gov/practice/jan-62014_Formulary.pdf Stevens, D., Bisno, A., Chambers, H., Everett, D., Dellinger, P., Goldstein, E., Gorbach, S…Wade, J. (2005). Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clinical Infectious Diseases, 41, 1373-1406. Wong, C., Khin, L., Heng, K., Tan, K., & Low, C. (2004). The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: A tool for distinguishing necrotizing fasciitis from other soft tissue infections. Critical Care Medicine, 32(7), 1534-1541. Yue J, Dong B., Yang M., Chen X., Wu T., Liu G. (2013). Linezolid versus vancomycin for skin and soft tissue infections. Cochrane Database of Systematic Reviews, 7, 1-62. doi: 10.1002/14651858.CD008056.pub2 WEB CASE STUDY 22 Appendix A. Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score Variable, Units Score C-Reactive Protein, mg/L <150mg/L 0 >150mg/L 4 White Blood Cell count, per mm^3 <15 0 15-25 1 >25 2 Hemoglobin, g/dL >13.5 0 11-13.5 1 <11 2 Sodium, mmol/L >135 0 <135 2 Creatinine, mg/dL <1.6 0 >1.6 2 Glucose, mg/dL <180 0 >180 1 Adapted from: “The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: A tool for distinguishing necrotizing fasciitis from other soft tissue infections” (Wong et al., 2004). WEB CASE STUDY 23 Discussion Questions 1. Initial tissue pathology came back positive for gram-positive cocci in chains resembling Group A-bega hemolytic Streptococcus, as well as thick gram-positive bacilli resembling Clostridium Perfringens, and gram-negative rods resembling Escherichia coli. How would antibiotic treatment differ? Consider mechanism of action, drug interactions, side-effects, and monitoring. 2. There are adjunctive therapies that have been proposed for treatment of NF in combination with surgical debridement and antibiotics. Discuss these therapies, including benefits, risks, and current recommendations.