Assessment of mutant homozygosity in
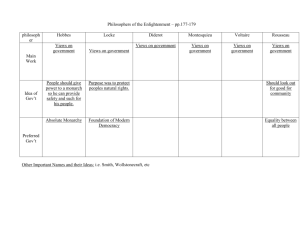
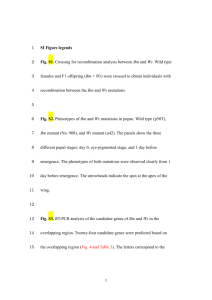
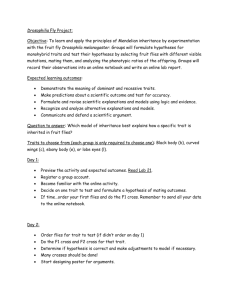
advertisement

Assessment of Mutant Homozygosity in Gastrointestinal Stromal Tumors Michelle Wallander1, Carlynn Willmore-Payne1 and Lester Layfield1,2 Institute for Clinical and Experimental Pathology, ARUP Laboratories, Salt Lake City, UT 2Department of Pathology, University of Utah, Salt Lake City, UT Introduction Results C G T A 30 Homoduplexes Heterozygote Melting Curve T G C Mutant GISTs (%) Mutant zygosity has not been extensively studied in gastrointestinal stromal tumors (GISTs), which are characterized by activating mutations in the receptor tyrosine kinases C-KIT or PDGFRA. We reviewed a series of mutant GISTs, which were previously analyzed by high resolution melting analysis (HRMA) and DNA sequencing. The percentage of mutant homozygosity in C-KIT exons 9, 11, 13, 17 and PDGFRA exons 12 and 18 was determined. Mutant homozygosity was also correlated with tumor location, size and CKIT (CD117) immunohistochemistry. Fluorescence Activated kinases such as EGFR, BRAF and C-KIT are associated with multiple human malignancies. Gain-of-function deletions, insertions or point mutations cause constitutive kinase activation, which stimulates cell proliferation and survival. Given the presumed dominance of the mutation, it is not surprising that the majority of activating mutations are heterozygous. However, homozygous CKIT and BRAF mutations have been reported in melanoma. The zygosity of kinase activating mutations may have important implications for oncogenesis or treatment response. 100 25 80 60 40 20 0 Heteroduplexes C-KIT exon 11 A C-KIT exon 9 C-KIT C-KIT PDGFRA PDGFRA exon 13 exon 17 exon 18 exon 12 Figure 1. High resolution melting analysis (HRMA) of heterozygous and homozygous DNA. The heterozygote melting curve is a combination of all four possible duplexes. The base pair mismatches in the heteroduplexes are unstable, resulting in a lower Tm that is easily detectable. Distinguishing between the two homoduplexes can be difficult since the Tm is dependent on the base pair change and nearest neighbor thermodynamics. Figure 4. Correlation of GIST mutant zygosity with mutation location. Distribution of heterozygous GIST mutations (blue) and homozygous GIST mutations (red) in all six tested exons. Homozygous mutations were detected in exon 11 (n = 36), exon 13 (n = 1), exon 18 (n = 3) and exon 12 (n = 2). 5 Homozygotes Figure 7. Correlation of GIST size with mutant heterozygosity and homozygosity. The mean heterozygous tumor size (when specified) was 7.84 6.73 cm (n = 34). The mean homozygous tumor size (when specified) was 11.52 9.63 cm (n = 16). P-Value = 0.181. Outlier samples = *. The majority of GIST mutant homozygosity occurred in C-KIT exon 11 (86%), which harbors the most GIST mutations (Figure 4). No homozygous mutations were detected in C-KIT exons 9 or 17. There was no correlation between CD117 IHC and GIST mutant homozygosity (Figure 5). 80 Fluorescence Mutant GISTs (%) 70 Homozygous GIST mutations were more prevalent than heterozygous GIST mutations, as a percentage, in metastatic sites like the liver and pancreas (Figure 6). 60 50 40 30 There was no significant correlation between tumor size and mutant homozygosity (Figure 7). 20 10 0 CD117 positive Temperature Figure 2. HRMA of a C-KIT K642E heterozygous sample (blue), a K642E homozygous sample with limited “contaminating” wild-type DNA (red) and a wild-type control (black). CD117 weak or focal CD117 negative CD117 not specified Figure 5. Correlation of CD117 (C-KIT) IHC with GIST mutant heterozygosity (blue) and homozygosity (red). Mutant GISTs (% Each Tumor Site) # of Mutant GISTs 80 200 150 100 70 60 50 40 30 20 50 Discussion Our results in 267 mutant GISTs suggests that the majority are heterozygous. However, homozygous mutations are more difficult to detect by HRMA and may therefore be slightly underrepresented. To improve homozygous mutant detection, known mutant genotypes could be mixed with the sample post-PCR to facilitate heteroduplex formation. Homozygous GIST mutants would be predicted to contain 100% mutant C-KIT or PDGFRA homodimer. This would increase KIT signaling by four-fold as compared to a heterozygous GIST mutant, which may result in a more aggressive tumor. We had limited data on tumor size and no data on patient outcome. We did see a greater frequency of homozygous mutations located in metastatic body sites, suggesting that tumors with homozygous GIST mutations may be more aggressive. Patient follow-up data will be critical for determining the prognostic value of a GIST homozygous mutation. 100 250 10 0 References Figure 3. GIST mutant homozygosity. Forty-two (16%) GISTs demonstrated mutant gene homozygosity. ifi ed tic ot s Willmore-Payne C, Holden JA, Hirschowitz S, Layfield LJ. BRAF and c-kit gene copy number in mutation-positive malignant melanoma. Human Pathology, 2006; 37:520-527. N et M pe c as ta ol on C tr a- G e tin Sm al St li nt es om Forty-two (16%) GISTs harbored homozygous mutations as determined by sequencing (Figure 3). Ex Homozygous h Heterozygous I 0 ac Homozygous mutant samples with limited “contaminating” normal DNA can be difficult to distinguish from the wild-type control (Figure 2). 10 Heterozygotes 90 High resolution melting analysis (depicted in Figure 1) detected 267 mutant GISTs. 15 Temperature A series of 267 GISTs with known mutations in C-KIT or PDGFRA were reviewed. Mutational analysis was originally performed at ARUP Laboratories. Briefly, formalin-fixed paraffin embedded tumor tissue was microdissected and DNA was extracted by proteinase K digestion. Crude DNA extract was used directly in PCR to amplify C-KIT exons 9, 11, 13 and 17 and PDGFRA exons 12 and 18. After amplification on the LightCycler (Roche Diagnostics, Indianapolis, IN), samples were briefly heated to 95°C and then cooled to 40°C. Samples were transferred to the HR-1 high-resolution DNA melting analysis instrument (Idaho Technology, Salt Lake City, UT) and heated at 0.3°C/sec to generate melting curves. Normalized and temperature-shifted melting curves were compared to wildtype DNA, which was used as a negative control. Results 20 0 Materials and Methods All samples with an abnormal melting curve were sequenced. Electropherogram peak height and the percentage of tumor in the sample were used to classify mutations as heterozygous or homozygous. Tumor location, size and CD117 immunohistochemistry (IHC) were obtained from the surgical pathology files at the University of Utah. The use of human tissue for this analysis was approved by the University of Utah Institutional Review Board (#11903). GIST Tumor Size (cm) 1ARUP Figure 6. Correlation of GIST location with mutant heterozygosity (blue) and homozygosity (red). Extra-GI includes the omentum, soft tissue, mesentary and peritoneum. Metastatic sites include the liver and pancreas. Holden JA, Willmore-Payne C, Coppola D, Garrett CR, Layfield LJ. High-resolution melting amplicon analysis as a method to detect c-kit and platelet-derived growth factor receptor alpha activating mutations in gastrointestinal stromal tumors. American Journal of Clinical Pathology, 2007; 128:230-238.