Histology Ch 21 647-655 [4-20
advertisement

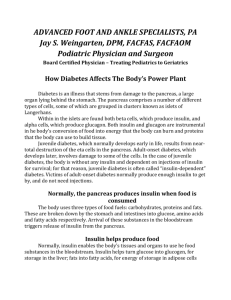
Histology Ch 21 647-655 Pancreas -Pancreas is elongated gland having a head, body, and a tail; head expanded portion lies in the C shaped curve of duodenum; joined to duodenum by connective tissue -body of pancreas crosses midline, and tail extends toward hilum of spleen -pancreatic duct extends through length of gland and empties into duodenum at the hepatopancreatic ampulla of vater (where common bile duct also enters duodenum) -the hepatopancreatic sphincter of Oddi surrounds ampulla and regulates flow of bile/pancreatic juice into duodenum and also prevents reflux of intestinal contents into the pancreatic duct -an accessory pancreatic duct is sometimes present as well -layer of loose CT encapsulates pancreas, and septa extend from capsule to divide pancreas into lobes, where loose CT surrounds parenchymal units Pancreas is an exocrine and endocrine glands – pancreatic exocrine component synthesizes and secretes enzymes into duodenum that are essential for digestion in the intestine -endocrine component synthesizes and secretes hormones insulin and glucagon into the blood to regulate glucose, lipid, and protein metabolism -exocrine pancreas found throughout the organ, and within exocrine pancreas, distinct cell masses called islets of Langerhans are dispersed and constitute endocrine pancreas Exorine Pancreas is a Serous Gland – resembles parotid gland; secretory units are acinar or tubuloacinar in shape and are formed by simple epithelium of pyramidal serous cells -these cells produce the enzyme precursors -pancreatic acini are unique among glandular acini… the intercalated duct leading from acinus, actually begins INSIDE the acinus, known as centroacinal cells -acinar cells characterized by distinct basophilia in basal cytoplasm and by acidophilic zymogen granules in apical cytoplasm (most numerous in fasting people) Zymogen granules contain variety of digestive enzymes in an inactive form – pancreatic enzymes digest most foods; the inactive enzymes (proenzymes) contained in pancreatic zymogen granules are: 1. proteolytic endopeptidases (trypsinogen, chymptrypsinogen) and exopeptidases (procarboxypeptidase, proaminopeptidase) – digest proteins by cleaving internal or external peptide bonds 2. Amylolytic Enzymes (α-amylase) – digests carbohydrates by cleaving glycosidic bonds 3. Lipases – digest lipids by cleaving ester bonds of triglycerides 4. Nucleolytic enzymes (deoxyribonuclease/ribonuclease) – digest nucleic acids -pancreatic digestive enzymes are activated only after they reach lumen of small intestine; initially, proteolytic activity of enterokinases in glycocalyx of microvilli of small intestine enterocytes convert trypsinogen trypsin, which then catalyzes conversion of other inactive enzymes as well as digestion of proteins in chyme. -Acinar cells are joined together by junctional complexes at their apical poles, forming an isolated lumen into which small microvilli extend from apical surfaces of acinar cells into which zymogen granules are released by exocytosis Duct system of pancreas – centroacinar cells are beginning of duct system of exocrine pancreas, and are intercalated duct cells located inside the acinus -intercalated ducts are short and drain into intralobular collecting ducts -intralobular ducts drain into larger interlobular ducts which are lined with low columnar epithelium in which enteroendocrine cells and goblet cells can be found -these drain directly into the main pancreatic duct running parallel to gland Intercalated ducts add HCO3 and H2O to Exocrine Secretion – pancreas secretes 1L of fluid/day, equal to hepatic bile secretion -although acini secrete small volume of protein-rich fluid, the intercalated duct cells secrete large volume of Na and HCO3; HCO3 neutralizes acidity of chyme that enters duodenum from stomach and establishes optimal pH for activity of pancreatic enzymes Pancreatic exocrine secretion is under hormonal and neural control – two hormones secreted by enteroendocrine cells of duodenum: secretin and cholecystokinin (CCK) are principal regulators of exocrine pancreas; acidity of chyme in duodenum stimulates release of hormones into the blood -Secretin – polypeptide hormone stimulates duct cells to secrete large volume of fluid with high HCO3 concentration but little enzyme -CCK – causes acinar cells to secrete their proenzymes -coordinated action of these two hormones results in large volume secretion of enzyme-rich, alkaline fluid into duodenum -pancreas also receives autonomic innervation: sympathetic fibers regulate pancreatic blood flow, parasympathetic fibers stimulate activity of acinar as well as centroacinar cells Endocrine Pancreas – diffuse organ secreting hormones that regulate blood glucose levels -the islets of Langerhans are scattered throughout the organ in cell groupings of varying size (1 million – 3 million exist and constitute 2% of pancreatic volume) -divided into A (α), B (β), and D (δ) cells A cells stain Red B cells stain brown-orange D cells stain blue -B cells are 70% of pancreatic islets containing insulin -A cells are 20% of islets and congain glucagon -D cells constitute 7% of pancreatic endocrine tissue and secrete somatostatin -G cells called gastrin cells secrete gastrin (tumor of which is involve din Zollinger-Ellison Syndrome) Functions of Pancreatic Hormones – all regulate metabolic functions -Insulin – decreases blood glucose levels, increases storage of glucose by activating glycogen synthase and subsequent glycogen synthesis, and phosphorylates glucose affects liver, muscle, and adipose -absence of insulin is involved in diabetes mellitus, and reduction is involved in Alzheimers -Glucagon – secreted second to insulin, INCREASES blood glucose levels and acts opposite to insulin; stimulates gluconeogenesis and glycogenolysis; also stimulates proteolysis and fat mobilization -Somatostatin – identical to hypothalamic hormone, regulates insulin/glucagon secretion Regulation of Islet Activity – blood glucose above 70mg/dL stimulates glucose release and uptake/storage by liver/muscle -the decrease in glucose sotps insulin secretion -increased fatty acids also stimulate insulin, as well as gastrin, CCK, and secretin -CCK and glucagon released by A cells act as paractin secretions to stimulate B cell secretion of insulin -below 70mg/dL, glucagon is stimulated until blood glucose rises; inhibited by fatty acids -insulin inhibits glucagon -islets have both sympathetic and parasympathetic innervation -parasympathetic (cholinergic) stimulation increases insulin/glucagon -sympathetic (adrenergic) stimulates glucagon but inhibits insulin -Blood supply to pancreas provides a cascading perfusion of islets and acini – capillaries first perfuse into A and D cells before reaching B cells -large efferent capillaries leave islets into capillary networks surrounding acini of exocrine pancreas -insulin, vasoactive intestinal peptide, and CCK stimulate exocrine secretion -glucagon, PP and somatostatin inhibit exocrine secretion Insulin Production and Alzheimer’s Disease – expression of insulin and IGFI and II in nerve cells is present. -insulin resistance of diabetes is linked to neural degeneration, cognitive dysfunction, and dementia -reduced rate of insulin secretion in brain leads to degeneration of neurons alzheimers -alzheimers could be manifestation of type 3 diabetes Functional Considerations: Insulin Synthesis – insulin produced by B cells consisting of 2 chains joined by disulfide bonds -first synthesized as preproinsulin required to entire rER; as it enters rER, it is cleaved to proinsulin -proinsulin is single polypeptide connected by 2 disulfide bonds -during packaging and storage by golgi, a cathepsin-like enzyme cleaves proinsulin to a two chain (A and B chain) insulin and a C peptide -C peptide lasts in blood longer, so it is an important blood marker for B cell secretion -C peptide can distinguish between type 1 and 2 diabetes