Slide 1 - Clinical Departments - Medical University of South Carolina
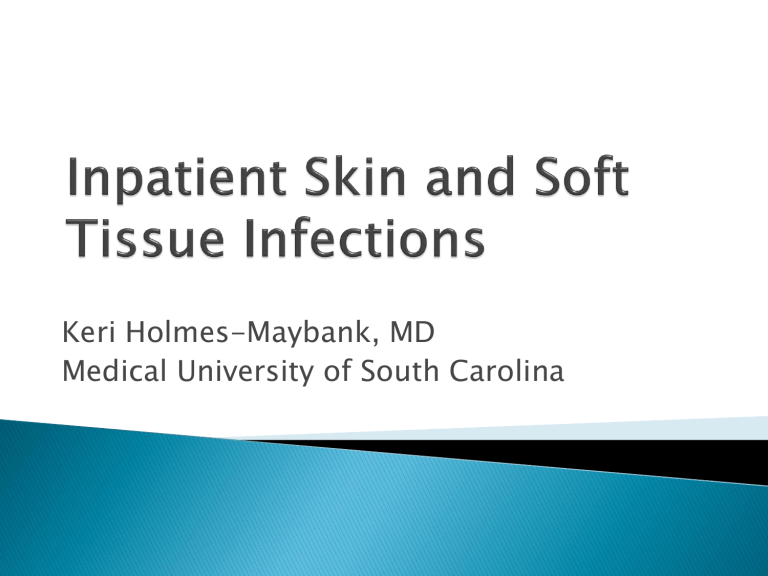
Keri Holmes-Maybank, MD
Medical University of South Carolina
Cellulitis
Impetigo
Erysipelas
Abscess
Animal bite
Human bite
Surgical site infection
Necrotizing fasciitis
Increasing ER visits and hospitalizations
29% increase in admissions, 2000 to 2004
Primarily in age <65
Presume secondary to community MRSA
50% cellulitis and cutaneous abscesses
Estimated $10 billion SSTI 2010
“Practice guidelines are systematically developed statements to assist practitioners and patients in making decisions about appropriate health care for specific clinical circumstances.”
Reduce emergence of resistant organisms
Reduce hospital days
Reduce costs:
◦ Blood cultures
◦ Consultations
◦ Imaging
◦ Hospital days
2011-Implementation of treatment guidelines
◦ Decreased use of blood cx
◦ Decreased advanced imaging
◦ Decreased consultations
◦ Shorter durations of therapy
◦ Decreased use of anti-pseudomonal
◦ Decreased use of broader spectrum abx
◦ Decreased costs
◦ No change in adverse outcomes
Systemic illness
◦ HR >100 and
◦ Temp >38 o C or <36 o C and
◦ Systolic bp <90 or decrease of 20 mmHg < baseline
◦ CRP>13
◦ Marked left shift
◦ Elevated creatinine
◦ Low serum bicarbonate
◦ CPK 2 x the upper limit of normal
Abnormally rapid progression of cellulitis
Worsening infection despite appropriate antibiotics
Tissue necrosis
Severe pain
Altered mental status
Respiratory, renal or hepatic failure
Co-morbidities: immune compromise, neutropenia, asplenia, preexisting edema, cirrhosis, cardiac failure, renal insufficiency
Indicators of more severe disease:
◦ Low sodium
◦ Low bicarb
◦ High creatinine
◦ New anemia
◦ Low or high wbc
◦ High CRP (associated with longer hospitalization)
Blood cultures positive <5%
Needle aspiration 5-40%
Punch biopsy 20-30%
HR >100 , Temp >38 o C and <36 o C, Sys <90mmHg
Lymphedema
Immune compromise/neutropenia/malignancy
Pain out of proportion to exam
Infected mouth or eyes
Unresponsive to initial antibiotics
Water-associated cellulitis
Diabetes
Recurrent or persistent cellulitis
Concern for a cluster or outbreak
HR >100 , Temp >38 o C and <36 o C,
Sys<90mmHg
◦ CRP>13
◦ Elevated creatinine
Marked left shift
Low serum bicarb
◦ CPK 2 x upper limit of normal
Immune compromise/neutropenia/malignancy
Diabetes
Animal or human bite wounds
Immune status
Geographic locale
Travel history
Recent trauma or surgery
Previous antimicrobial therapy
Lifestyle - occupation
Hobbies
Animal exposure
Bite exposure
If no improvement in systemic signs in 48 hours
If no improvement in skin in 72 hours
As antibiotics kill organisms, released toxins may cause a worsening of skin findings in first 48 hours
Acute skin findings resolving
Afebrile
No signs of systemic illness
Should see systemic signs improvement by
48 hours
Should see skin improvement 3-5 days by at the latest
65% relative increase since 1999
600,000 admissions annually
Obesity
Edema
◦ Venous insufficiency
◦ Lymphatic obstruction
Fissured toe webs
◦ Maceration
◦ Fungal infection
Inflammatory dermatoses – eczema
Repeated cellulitis
Subcutaneous injection or illegal drugs
Previous cutaneous damage
All lead to breaches in the skin for organism invasion
Saphenous venectomy
Axillary node dissection for breast cancer
Gyn malignancy surgery with lymph node dissection *** in conjuction with XRT
Liposuction
CBC with diff
BMP
Blood cultures
Culture aspiration of leading edge of cellulitis
INTACT SKIN
No purulent drainage, no exudate, no associated abscess
Beta hemolytic streptococci
Antibiotic:
◦ Cefazolin
◦ Documented anaphylactic cephalosporin allergy -
Vancomycin
Deescalation:
◦ Cephalexin
◦ Beta-lactam anaphylaxis - clindamycin
5 days of treatment
BROKEN SKIN
Purulent drainage
Exudate
Absence of a drainable abscess
MRSA coverage
Antibiotics:
◦ Vancomycin
Deescalation:
◦ Trimethoprim/sulfamethoxazole + cephalexin
◦ Beta lactam anaphylaxis – clindamycin
◦ Sulfa allergy – tetracycline or doxycycline
◦ If sulfa and beta lactam allergies - linezolid
5 days of treatment
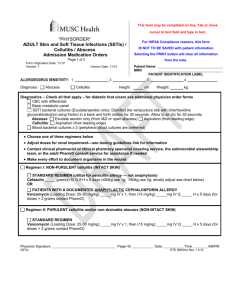
Empiric SSTI algorithm
*This algorithm does NOT include: surgical site infections, diabetic foot ulcers, decubitus ulcers, insect, animal or human bites, or gangrene
**Please see order form for guidance (including renal dosing adjustments)
Yes < 3 cm
I&D; No Cx;
No antibiotics
Nonnecrotizing
SSTI
Empiric
Adult SSTI
Necrotizing
Fasciitis
Abscess 1
Drainable?
Yes >3 cm; I&D and culture
(exudate aerobic only)
Vancomycin
(25-30 mg/kg; doses
> 2 grams contact
PharmD on call) IV x
1, then (15 mg/kg) IV
Purulent
Cellulitis
(Complicated)
Intact Skin
Cellulitis
(Uncomplicated)
Cefazolin
1
- 2 gram IV Q8H x 5 days
Immediate ID and surgical consult for
STAT debridement
Vancomycin
(25-30 mg/kg; doses
> 2 grams contact
PharmD on call) IV x
1, then (15 mg/kg) IV
No – Treat if
I&D is NOT possible
Vancomycin
(25-30 mg/kg; doses
> 2 grams contact
PharmD on call) IV x
1, then (15 mg/kg) IV
(
If cephalosporin allergic:
Vancomycin can be substituted for cefazolin
1 The preferred method of treatment is
I&D
Clinical Pearl: Treatment should continue for 48 hours prior to determination of clinical failure; SSTIs often appear worse during initial treatment period
Antibiotic De-escalation Criteria
1. Culture susceptibilities
2. Clinical response
1. Clinically stable
2. Decreased erythema
3. Decreased edema
4. Decreased warmth
5. Resolving leukocytosis
6. Afebrile
Empiric Adult SSTI –
Antibiotic
De-escalation
Non-purulent Cellulitis
INTACT SKIN
(Uncomplicated)
Purulent Cellulitis
NON-INTACT SKIN
(Complicated)
Completely Drained
Abscess
Non-drainable Abscess
Cephalexin 500 mg PO
Q 6 H (to complete
5 day total course)
TMP/SMX 160/800 mg
PO Q 12 H plus
Cephalexin 500 mg PO
Q 6 H (to complete
5 day total course)
TMP/SMX 160/800 mg
PO Q 12 H plus
Cephalexin 500 mg PO
Q 6 H (to complete
5 day total course)
TMP/SMX 160/800 mg
PO Q 12 H plus
Cephalexin 500 mg PO
Q 6 H (to complete
5 day total course)
Total course of antibiotics is 5 days (i.e. 2 days of IV cefazolin + 3 days of PO cephalexin)
Note: Renal dose adjustments are required for patients with CrCL less than 30 mL/min
If sulfa allergic: Either tetracycline or doxycycline can be substituted to replace TMP/SMX
If beta-lactam anaphylaxis: Clindamycin (non-severe infection) can be substituted to replace cephalexin, or linezolid can be substituted to replace both TMP/SMX and cephalexin
Elevation of affected leg
Compression stockings
Treat underlying tinea pedis, eczema, trauma
Keep skin well hydrated
Acute dermatitis
Lipodermatosclerosis
Deep vein thrombosis
Contact dermatitis
Drug reaction
Foreign body reaction
Gout
Herpes zoster
ALWAYS, ALWAYS
◦
Incision and drainage
Incision and drainage
No blood cultures
No aspirate culture
NO ANTIBIOTICS
CBC with diff
BMP
Blood cultures
Culture exudate
Drainable abscess >3cm
Undrainable
Multiple sites of infection
Rapid progression in presence of cellulitis
Systemic illness (fever, hypotension, tachycardia)
Immune compromise
Elderly
Difficult to drain area (hand, face, genitalia)
Lack of response to incision and drainage
Septic phlebitis - multiple lesions
Gangrene
MRSA coverage
Antibiotic:
◦ Vancomycin
Deescalation:
◦ Trimethoprim/sulfamethoxazole + cephalexin
◦ Beta lactam anaphylaxis – clindamycin
◦ Sulfa allergy – tetracycline or doxycycline
◦ If sulfa and beta lactam allergies - linezolid
Treatment duration:
◦ Usually 5 days of treatment – 10 maximum
Pasteurella – mc organism
Antibiotics:
◦ Ampicillin/sulbactam
◦ Piperacillin/tazobactan
◦ Cefoxitin
◦ Meropenem
◦ Ertapenem (restricted to ID and Surgery)
Tetanus toxoid (if not up to date)
Deescalation
◦ Amoxicillin/clavulanate
◦ Doxycycline
Treatment duration:
◦ Discontinue abx 3 days after acute inflammation disappears
◦ Usually 5-10 days of treatment
Antibiotics:
◦ Ampicillin/sulbactam
◦ Meropenem
◦ Ertapenem (restricted to ID and Surgery)
Tetanus toxoid (if not up to date)
Closed fist***
Antibiotics:
◦ Cefoxitin
◦ Ampicillin/sulbactam
◦ Ertapenem(restricted to ID and Surgery)
Tetanus toxoid (if not up to date)
Hand surgery consult***
Deescalation:
◦ Amoxicillin/clavulanate
◦ Moxifloxacin + clindamycin
◦ Trimethoprim/sulfamethoxazole + metronidazole
Treatment duration:
◦ Discontinue abx 3 days after acute inflammation disappears
◦ Usually 5-10 days of treatment if no joint or tendon involvement
Pain, swelling, erythema, purulent drainage
Usually have no clinical manifestations for at least 5 days after operation
Most resolve without antibiotics
Open all incisions that appear infected >48 hours after surgery
No antibiotics if temperature <38.5
o
C and
HR <100 bpm
If temperature >38.5
o C or HR >100 bpm:
Trunk, head, neck, extremity
◦ Cefazolin
◦ Clindamycin
◦ Vancomycin if MRSA is suspected
Perineum, gi tract, female gu tract
◦ Cefotetan
◦ Ampicillin/sulbactam
◦ Ceftriaxone + metronidazole or clindamycin
◦ Fluoroquinolone + clindamycin
Treatment duration:
◦ Usually 24-48 hours or for 3 days after acute inflammation resolves
ALWAYS blood CULTURES
Initial infection - <7 days neutropenia
Antibiotics
◦ Carbapenems
◦ Cefepime
◦ Ceftazidine
◦ Piperacillin/tazobactam
PLUS
◦ Vancomycin
◦ Linezolid (restricted to ID)
◦ Daptomycin (restricted to ID)
◦ (discontinue if culture negative after 72-96 hours)
Subsequent infection- >7days neutropenia (fungi, viruses, atypical bacteria)
Treatment:
◦ Amphotericin B
◦ Micafungin (may require higher dose and ID consult)
◦ Voriconazole (restricted to ID, Heme/Onc, Critical Care,
Pulmonary, and Transplant)
PLUS
◦ Carbapenems
◦ Cefepime
◦ Ceftazidine
◦ Piperacillin/tazobactam
PLUS
◦ Vancomycin
◦ Linezolid (restricted to ID)
◦ Daptomycin (restricted to ID)
◦ (discontinue if culture negative after 72-96 hours)
Deescalation:
◦ Ciprofloxacin and amoxicillin/clavulanate
Treatment duration:
◦ At least 7 days
Device predisposes to SSTI
66% Gram positive
Entry site infection
◦ Antibiotics
Tunnel infection and vascular port-pocket infection
◦ Device removal and antibiotics
Not all diabetic foot ulcers are infected.
Infection if at least 2 present:
Purulent secretions
Redness
Warmth
Swelling/induration
Pain/tenderness
Common, complex, costly
Largest number of diabetes-related hospital bed days
Most common proximate, non-traumatic cause of amputations
Recent hospitalization last 90 days
Residence in long term care facility
Antibiotics last 90 days
Injection drug use
Hemo- or peritoneal dialysis
Incarceration last 90 days
Home infusion therapy
History of MRSA colonization
Immunosupressive state/medications
Wound care in past 30 days
ICU stay in last 90 days
Immunosuppressive state/medications
Immunosuppressive states includes:
◦ HIV, solid organ transplants, BMT
Immunosuppressive medications includes:
◦ Rejection medications, >20mg/d prednisone x2w
Cellulitis or erythema extends <2cm around ulcer, infection limited to skin – no systemic indications
Obtain foot xray – screen for osteomyelitis
Antibiotics:
◦ No MRSA risk:
Cephalexin
Amoxicillin/clavulanate
◦ MRSA risk:
Trimethoprim/sulfamethoxazole
Doxycycline
Treatment duration
◦ Usually 1-2 weeks treatment (can be as long as 4 weeks)
Erythema extends >2cm around ulcer or signs of abscess, osteomyelitis, septic arthritis, fasciitis – no systemic signs
Foot x-ray
Culture wound
Wound care
Assess need for debridement general surgery
CRP
ESR
Bone biopsy for culture
MRI if ESR and CRP elevated
ID consult if osteomyelitis present
Erythema extends >2cm around ulcer and signs of systemic infection(hypotension, hyperthermia, tachycardia)
Foot xray
Culture wound
Blood cultures
Wound care
Assess need for debridement general surgery
CRP
ESR
Consider MRI if suspect abscess or uncertain if osteomyelitis or if the ESR and CRP
Bone biopsy
ID consult if osteomyelitis
Wound care
Debridement
Glycemic control
Evaluate vascular status
Cards
Not on cpoe or clinician order forms
Quality
Starts now – review at end of June 2013
Algorithm – antibiotics
Questions for Dr. Gomez or Dr. Hurst?
Gunderson CG. Cellulitis: Definition, etiology, and clinical features. Am J Med
2011;124:1113-1122.
Jenkins TC, et al. Decreased antibiotic utilization after implementation of a guideline for inpatient cellulitis and cutaneous abscess. Arch Intern Med.
2011;171(12):1072-1079.
Rajan S. Skin and soft-tissue infections: Classifying and treating a spectrum.
Cleveland Clinic Journal of Medicine. 2012;79(1):57-66.
Swartz MN. Cellulitis. N Engl J Med 2004;350:904-912.
IDSA GUIDELINES:
Lipsky BA, et al. Diagnosis and treatment of foot infections. Clin Infect
Dis 2004;39:885-910.
Liu C, et al. Clinical practice guidelines by the Infectious Diseases Society of
America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis 2001;52(3):e18-e55.
Stevens DL, et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis 2005;41:1373-1406.
MUSC Antibiotic Stewardship – Drs. Juan Manual Gomez, Sean Boger, John Hurst.