Chapter 4 ss Female Sexual A_and_P
advertisement

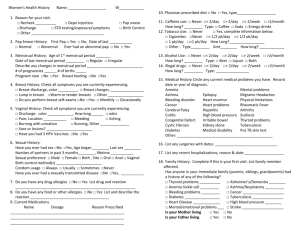
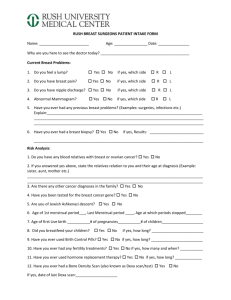
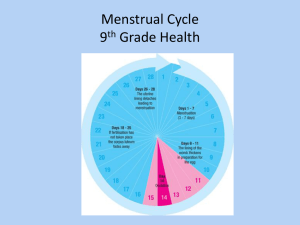
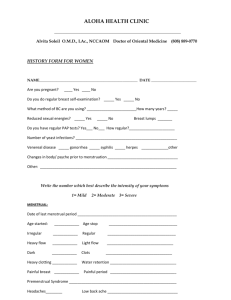
Chapter 4 Female Sexual Anatomy & Physiology Genital Self-Exam • Increases sexual comfort – Feeling familiar and comfortable with one’s anatomy can enhance sexual experiences • Monitor for changes related to health concerns – If you don’t know what “normal” looks like, you can’t know if something seems abnormal and requires medical attention. The Vulva • Vulva = all female external genital structures – Includes hair, folds of skin, and urinary and vaginal openings – Appearance varies from person to person The Vulva (cont.) Fig. 4.1 The structures and variations of the vulva: (a) external structures. Tour of the Vulva Mons veneris (from Latin “mound of Venus”): - Triangular mound over the pubic bone. - Consists of pads of fatty tissue btwn. pubic bone and skin. - Touch and pressure can be pleasurable due to numerous nerve endings. - At puberty, becomes covered with hair - Purpose of hair is to trap pheromones from vaginal secretions, adding to sensory erotic pleasure. Labia majora (outer lips): - Extend downward from mons veneris on each side of vulva. - Like mons veneris, touch and pressure can be pleasurable due to numerous nerve endings. Tour of the Vulva Labia minora (inner lips): - Located within outer lips and may protrude between them. - Hairless folds of skin that join at the prepuce (clitoral hood) and extend down past urinary and vaginal openings - Contain sweat glands, blood vessels, and nerve endings. - Vary considerably in size, shape, and color; become darker in color during pregnancy. Tour of the Vulva Clitoris: - Highly sensitive structure of the female external genitals. - Is the only organ in the human body whose only function is pleasure. - Consists of: - glans - shaft: has small spongy structures that engorge with blood during sexual arousal. - internal crura (roots) - Covered by clitoral hood - Stimulation of clitoris is the most common way that most women achieve orgasm. - External part of the clitoris has about the same # of nerve endings as the head of the penis. Tour of the Vulva Vestibule: - Area inside labia minora. - Urinary and vaginal openings are located within the vestibule. Perineum: - Area of skin between the vaginal opening and the anus - Urinary and vaginal openings are located within the vestibule. Female Genital Cutting • Circumcision: cutting off the clitoral hood. • Clitoridectomy: removal of the clitoris. • Genital infibulation: – Removal of the clitoris – Labia are cut off – Both sides of the vulva are stitched together • Procedures done w/o anesthetics, disinfectants, or sterile instruments • Cultural tradition in >40 countries in Africa, the Middle East, and Asia--clitoris is seen as male b/c it gets erect; ensures marriageability of girls • Serious gynecological and obstetric complications result from infibulation Underlying Structures of the Vulva (Fig 4.2) –Fill with blood during arousal, causing vulva to swell and vagina to increase in length. –Similar in structure and function to tissue in penis that engorges during arousal, causing erection. Secrete drop or two of fluid just before orgasm. Underlying Structures of the Vulva more on Kegel exercises in Chp. 5… Fig. 4.3 The underlying muscles of the vulva. These muscles can be strengthened using the Kegel exercises described in the text. Internal Structures (cont.) Fig. 4.4 Internal female sexual anatomy: front view of the internal organs. Parts of the ovaries, uterus, and vagina are shown cut away. Internal Structures (cont.) Fig. 4.4 Internal female sexual anatomy: (a) cross-sectional side view of female internal structures. • Vagina Internal Structures – Approx. 3-5 in. long--can elongate during arousal, stretch during childbirth, etc. – 3 layers: mucous, muscle, fibrous – Arousal and vaginal lubrication • Vaginal tissue blood vessels become engorged, causing clear fluid from the tissues to moisten the inside of the vaginal wall. • lubrication changes () vaginal pH and increases pleasure – Grafenberg (G) spot • Anterior (front) wall of vagina • Female equivalent of prostate gland – Secretions & chemical balance • Douching, feminine hygiene sprays, etc. are not only unnecessary, they cause numerous health problems. • Cervix Internal Structures – At the upper/back end of the vagina – Leads into uterus • Os: the small opening in the cervix that leads into uterus – Dilates to 10 cm opening during labor & birth Internal Structures • Uterus (or womb) – Hollow, thick, pear-shaped organ – 3 in. long, 2 in. wide in woman who has not had a child. – Walls consist of 3 layers • External: perimetrium • Middle: myometrium – (stretching, contraction) • Inner: endometrium – (nourishes zygote, sheds each month if no fertilization during menstruation) Internal Structures • Fallopian tubes – Extend from uterus to each ovary (each tube about 4 in.) – Lined with cilia to help move ovum along tube – Outside end of each tube is shaped like a funnel, with fringelike projections called fimbriae • When egg leaves ovary, it’s drawn into fallopian tube by the fimbriae. Fertilization – Ectopic pregnancy: when fertilized ovum implantsoccurs fairly outside of the uterus (usually in the fallopian tube). close to ovary • Can rupture the tube and cause uncontrolled bleeding Internal Structures • Ovaries – Endocrine glands that produce ova (eggs) and sex hormones. – 3 types of hormones produced: • Estrogens • Progesterones • Testosterone – Ovulation: the maturation and release of an egg from the ovary into the fallopian tube • Up to 472,000 ova at birth • Only about 400 will mature Group activity: female A & P flashcards One side: name of term Other side: definition, function, location TERMS: Vulva Mons veneris Labia majora Labia minora Clitoris Perineum Vagina Cervix Uterus Fallopian tubes Ovaries Discussion question: (4-A) • What are some slang terms for female genitalia and breasts? Keep track of how many terms your group knows. • Are these terms positive or negative? • Why do people tend to use “nicknames” for parts of the female sexual anatomy? • How might men and women become more comfortable using correct terms for female anatomy? Menstruation • Myths and negative attitudes – In the U.S., girls used to be taught that menstruation was dirty, something to be hidden. • Advertisements for “feminine hygiene products” often capitalized on these negative attitudes toward menstruation (see next slide) – Some cultural attitudes toward menstruation are positive • Association with transformation to adulthood, purification, spirituality, connectedness with natural cycles. – Today, even w/negative attitudes, most women associate regular menstruation with health. – Research has shown that women who have positive attitudes and comfort w/menstruation are more likely to be comfortable with their bodies and their sexuality. Menstruation (cont.) • Menarche (initial onset) – age 11-15 (avg: about 12.5 yr) – related to heredity, health, – Age has decreased over time: • Many reasons proposed, environmental pesticides, etc.), altitude including estrogens (in obesity, stress. • Menstrual physiology – – – – flow lasts from 2 to 6 days volume varies (6 to 8 ounces) duration varies (24 to 42 days) menstrual synchrony: simultaneous menstrual cycles that sometimes occur among women who live in close proximity. Menstruation (cont.) Fig. 4.7 Ovulation timing and cycle length. Regardless of the length of the cycle, ovulation occurs approximately 14 days before menstruation. Menstrual cycle: control by hormones • hypothalamus releases GnRH that stimulates pituitary • pituitary produces: – Follicle-stimulating hormone (FSH): • Estrogen production in ovaries • Ovum maturation in follicles inside ovaries – Luteinizing hormone (LH): • Stimulates release of mature ovum • Stimulates development of corpus luteum, the progesteronesecreting part of the follicle that remains after egg is released. • Negative feedback mechanism – Each hormone is secreted until the organ it acts upon is stimulated--then that organ secretes a hormone that reduces secretion of the first hormone. Menstrual cycle: 3 phases 1) Menstrual phase: menstruation - Menstrual flow=endometrial tissue, blood, and mucus - FSH: ovum (egg) matures inside follicle Egg produces estrogen: causes endometrium to thicken a little LH: causes ovulation (release of mature egg from follicle) 2) Proliferative phase: follicles mature, release ovum - 3) Secretory phase: corpus luteum develops - Corpus luteum develops from follicle & secretes progesterone progesterone: endometrium thickens & engorges w/blood & nutrients in preparation for implantation of a fertilized egg If there is no implantation, corpus luteum degenerates, and estrogen & progesterone levels fall --> triggers menstruation. Changes during menstrual cycle Gonadotropins (FSH, LH) Changes in the ovary Levels of estrogen & progesterone Changes in the endometrium Proliferative phase: Changes to ovaries and uterus • Follicle matures and releases ovum • Uterine lining begins to thicken Fig 4.6a Secretory phase: Changes to ovaries and uterus Uterine lining continues to thicken • Development of corpus luteum from follicle (corpus luteum degenerates if there’s no implantation of a fertilized egg in the uterus) • Uterine lining continues to thicken Fig 4.6b Menstrual phase: Changes to ovaries and uterus • Uterine endometrium is shed as menstrual flow Fig 4.6c Menstruation (cont.) • Sexual activity and the menstrual cycle • Menstrual cycle problems – premenstrual syndrome: • Premenstrual Dysphoric Disorder – dysmenorrhea = painful menses – amenorrhea = no menses – toxic shock syndrome – self-help for menstrual symptoms Sexual activity and the menstrual cycle • Libido is typically maximal around ovulation, as well as during menstruation • There are no medical reasons to avoid sex during menstruation • Orgasm during menstruation can be beneficial-relieves, backache, cramping, etc. Menstrual cycle problems • Premenstrual syndrome (PMS) - catchall term for a number of symptoms of physical discomfort and emotional irritability 2-12 days before menstruation – PMDD (Premenstrual dysphoric disorder): Premenstrual symptoms severe enough to significantly affect a woman’s functioning • Dysmenorrhea - pain or discomfort before or during menstruation - Can include cramping, backache, headache, nausea, fatigue • Amenorrhea - absence of menstruation – Can be caused by too little body fat (amenorrhea is common in training athletes, women with anorexia nervosa) Discussion question (4-B): PART 1: What types of sexual activity are acceptable during menstruation? PART 2: Where did you learn about female sexual anatomy and the menstrual cycle? Was the information that you received accurate and thorough? Menopause • Terms – Peri-menopause: time before menopause, when estrogen levels are decreasing – Menopause: permanent cessation of menstruation • Average age is 51 (range: 30s to 60s) Menopause (cont.) • Symptoms vary from mild to strong (due mostly to the decline in estrogen levels) – hot flashes or warm spells from rapid dilation of blood vessels (about 75% of women experience these) – night sweats, interrupted sleep – headaches, poor concentration – depression, anxiety – vaginal dryness, reduced libido Hormone Therapy during and after menopause • Hormone therapy: the use of supplemental hormones (estrogen, progesterone, testosterone) – Benefits: (mostly estrogen) can reduce hot flashes, night sweats, vaginal dryness, loss of bone density and (mostly testosterone) increase overall energy and sexual interest – Problems: Increased risk of endometrial, ovarian, and breast cancer; increased risk of blood clots, cardiovascular disease (prog. HT) Alternatives to Hormone Therapy • Lifestyle factors – Women who are sexually active have fewer changes in vaginal tissues and lubrication. – Exercise, avoiding caffeine, tobacco, alcohol, and spicy foods can reduce hot flashes. • Vitamins and herbs – Calcium supplements, vitamin D, and weightbearing exercise can prevent osteoporosis. – Vitamin E, herbs (e.g. dong quai or black cohosh) can relieve symptoms such as hot flashes. Gynecological Health Concerns • Urinary tract infections (UTIs) – Usually due to bacteria that enter urethral opening. – If infection spreads past bladder into kidneys, severe illness can result. – Treatable with antibiotics. * Prevention: Wiping from front to back (from vulva to anus) Avoiding introducing bacteria from the rectum from into the vagina during sexual activity Don’t wait to urinate--urinate as soon as you feel the urge to avoid stretching the bladder Use water-soluble lubricants during sexual activity (not petroleum jelly) Urinate after intercourse. Gynecological Health Concerns (cont). • Vaginal infections (aka vaginitis) – Include yeast infections, bacterial infections, etc. (more in Chp. 17) – Some factors that increase susceptibility to vaginitis: • • • • • • • • • Diabetes Antibiotic use Stress Diet high in simple carbohydrates Intercourse w/o adequate lubrication Hormonal changes due to pregnancy or birth control pills Wearing nylon underwear or panty hose (trap heat and moisture) Douching Unprotected sex (STDs can cause vaginitis) Gynecological Health Concerns (cont). • Cysts – Fluid-filled sac that sometimes grow on the ovary – Fairly common, usually resolve on their own and are unnoticeable – Need to be monitored if they become painful • Endometriosis – Condition in which uterine endometrial tissue grows on various parts of the pelvic cavity. – Cause pelvic pain, often quite severe – Can cause infertility • Self-exams & vaginal health care – The greater awareness a woman has about her body, the better able she will be to diagnose problems. The Pap Smear • To screen for cervical cancer. • Cells are taken from the cervix and examined under the microscope • Since widespread use of Pap smears began in 1950s, the death rate of cervical cancer has decreased dramatically b/c if cancer is found, it is usually at a very early stage. normal dysplasia cervical cancer Surgical removal of the uterus or ovaries • Hysterectomy: surgical removal of the uterus. • Oophorectomy: surgical removal of the ovaries • Can be necessary due to bleeding disorders, pelvic infections, fibroids, cancer. • Most frequently performed operation in U.S.--1/3 of women will have a hysterectomy by age 65. – more frequently performed on low income, less educated women • Can decrease sexual responsiveness due to hormonal changes, loss of nerves in the pelvis, loss of ability to have uterine contractions. • There are some alternatives to surgery--women should be fully informed about all options. The Breast • Mammary glands produce milk – fatty tissue determines size – There is little variation among women in amount of glandular tissue present • Therefore, amount of milk for breastfeeding doesn’t correlate with breast size. • Areola is darker area • Nipple is in center of areola – Has many nerve endings & has openings for milk. • Breasts are secondary sex characteristics – Physical characteristics other than genitals that indicate sexual maturity (such as body hair, breasts, and deepened voice). The Breast (cont.) Fig. 4.8 Cross-section front and side views of the female breast. Breasts come in lots of shapes and sizes • Media/porn, etc. has distorted our idea of what a “normal” breast looks like • Some normal breasts: (from http://www.007b.com/breast_gallery.php) Breast cancer screening • Breast exams: early detection is best b/c treatments work better on early stage cancers – self-exam following menstruation – routine healthcare provider exams Breast cancer screening, (cont.) • Mammography: X-ray of the breast – Can detect breast lump before it can be felt manually. – Recommended yearly for women over 50 – Sometimes recommended for women between 40-50, though mammograms are less effective in women under 50 b/c the breast tissue is more dense. – Can miss tumors-• better screening methods are needed. Breast health • Breast lumps: 3 types – cysts (fluid-filled sacs, benign) – fibroadenomas (solid, round, benign tumors) – malignant tumor (tumor made up of cancer cells) • Breast cancer – Incidence: 1 in 9 women in North America; 190,000 new diagnoses each year. – Kills 40,000 women in U.S. each year and 370,000 women worldwide each year. – In North America, one woman dies of breast cancer approximately every 12 minutes. Breast cancer • Early detection increases survival b/c cancer is usually found at an earlier stage. • The 5-year survival rate is lower for minority women than for white women, most likely due to differences in access to preventive health care. Stage of cancer Percentage of cancer diagnosed at this stage Survival Rate at 5 years (%) Local (confined to breast) 60 98 Regional (spread to lymph nodes) 31 76 Distant (spread to other organs) 6 16 Breast cancer: risk factors • Risk rises with age • Growing evidence indicates that synthetic chemicals found in plastics, pesticides, detergents, and cosmetics can increase the risk of breast cancer • Cosmetics and personal care products are not tested by the Food and Drug Administration (FDA) because they are not foods and are not drugs – Nonetheless, chemicals in these products can penetrate our skin and our bodies. • To check your personal care products and, if necessary, look for safer alternatives, go to: www.cosmeticsdatabase.com Breast cancer treatment • Surgery – Mastectomy: surgical removal of all or most of the breast – Lumpectomy: removal of part of the breast containing the tumor and some surrounding tissue. • Chemotherapy and/or radiation – Kills rapidly dividing cells (tumor cells generally divide more than normal cells) Breast cancer activism • 3 local groups committed to increasing awareness of breast cancer and advocating for breast cancer prevention. – Breast Cancer Fund (S.F.) – Breast Cancer Action (S.F.) – Women’s Cancer Resource Center (Berkeley) • Resource library, supportgroups Discussion question: (4-C) If you or your partner had a mastectomy (removal of a breast), how do you think this would affect your sexual feelings toward yourself/your partner? What would the effects be if you or your partner had a hysterectomy (removal of uterus)