ACLS/BLS Exam Questions: 2010 Guidelines
advertisement

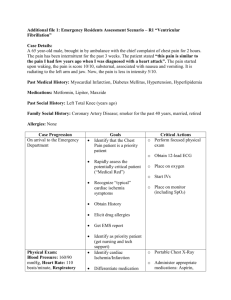
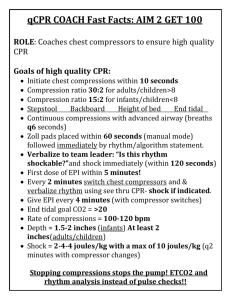
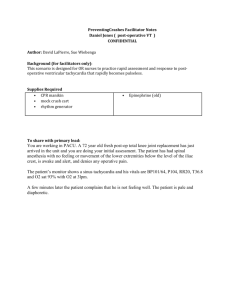
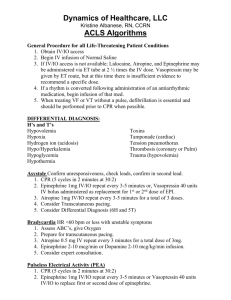
ACLS 2010 qustions BLS - שאלות 1. The 2010 guidelines added a 5th link in the AHA ECC Adult Chain of Survival. This addition was: – a. rapid defibrillation – b. integrated post-cardiac arrest care – c. effective advanced life support – d. early CPR with emphasis on chest compressions 2. (True or False) Chest compressions should be stopped while the defibrillator is charging. – True – False • 3. The BLS Survey focuses on: – early CPR and early defibrillation – early use of advanced airways and drugs – rapid access to emergency services – proper rhythm interpretation 4. Success of any resuscitation attempt is built on: – A. high quality CPR – B. defibrillation when required by the patients ECG rhythm – C. neither A or B – D. both A and B 5. The most important algorithm to know for adult resuscitation is: – A. Bradycardia – B. PEA – C. Tachycardia – D. Cardiac Arrest 6. The systematic approach with a person in cardiac arrest should include the BLS survey and the ACLS survey? – True – False 7. While conducting the BLS Survey, you should do all of the following except: – A. check patient responsiveness – B. active emergency response system – C. open the airway – D. get an AED 8. According to new 2010 Guidelines for CPR, which of the following is in the correct order for the patient with sudden cardiac arrest? – A. open airway, provide ventilations, give 30 chest compressions, attach AED as soon as possible – B. give 30 compressions, open airway, provide ventilation, attach AED as soon as possible – C. open airway, check breathing, check pulse , attach AED as soon as possible – D. none of the above 9. After providing a shock with an AED you should: – A. Start CPR, beginning with chest compressions – B. check a pulse – C. give a rescue breath – D. let the AED reanalyze the rhythm 10. During CPR with no advanced airway in place the compression-to-ventilation ratio is: – A. 5:1 – B. 30:2 – C. 10:1 – D. 20:2 11. During CPR after an advanced airway is in place, which of the following is true: – A. The breaths should be synchronized with the chest compressions. – B. The goal is 20 or greater breaths per minute – C. Chest compressions should be stopped while giving breaths. – D. One breath every 6 to 8 seconds should be given 12. The most important intervention with witnessed sudden cardiac arrest is: – A. early defibrillation – B. effective chest compressions – C. early activation of EMS – D. rapid use of resuscitation drugs 13. Typically, suctioning attempts in ACLS situations should be: – A. ten seconds or less – B. 20 seconds or less – C. 5 seconds or less – D. no more than 30 seconds • 3. When performing BLS/ACLS you should avoid all of the following except: – prolonged rhythm analysis – frequent pulse checks – taking too long to give rescue breaths to the patient – keeping the patients airway open • 4. When checking for a carotid pulse during CPR you should take no longer than ______seconds before restarting CPR – Fifteen – Ten – Five – twenty • 5. Interruptions in chest compressions should be limited to no longer than _____seconds. – Twelve – Five – Ten – Fifteen • 10. Which of the following is true about chest compressions: – push hard and fast – ensure full chest recoil – minimize interruptions in chest compression – all of the above • 3. Which of the following is performed before and/or during the BLS Survey: – a. make sure the scene is safe – b. activate EMS and get an AED if available – c. tap the victim's shoulder and say "Are you alright?“ – d. all of the above • 5. Which of the following is the correct sequence of steps for BLS according to the 2010 Guidelines? – a. chest compressions, airway, breathing, early defibrillation, if necessary – b. airway, breathing, circulation, definitive care – c. circulation, airway, breathing, differential diagnosis – d. access care early, begin CPR, check pulse, early defibrillation, if necessary • 8. Five cycles of CPR should take about __________minutes. –2 –3 –1 –4 2010 Guidlines 3. Which is now recommended for confirming placement of the endotracheal tube after intubation? – a. exhaled carbon dioxide detector – b. oxygen saturation monitor – c. esophageal detector device – d. continuous waveform capnography • 9. During CPR with an advanced airway in place the compression rate is: – ≥ 80/min – ≥ 60/min – ≥ 100/min – ≤90/min • 1. Examples of advanced airway adjuncts include all the following except: – a. oropharyngeal airway – b. laryngeal tube – c. laryngeal mask airway – d. combitube – e. endotracheal tube • 2. Which is not true about the oropharyngeal airway(OPA): – a. The OPA keeps the airway open during bagmask ventilation. – b. The OPA can stimulate coughing and gagging. – c. The OPA can prevent the patient from biting on an ET tube. – d. The OPA should only be used on a conscious patient • 7. During the ACLS Survey when assessing (B)breathing, which of the following is correct about supplementary oxygen delivery? – a. Administer 100% oxygen for cardiac arrest patients – b. Other than cardiac arrest, administer oxygen to maintain O2 saturation value o≥ 94% by pulse oximetry – c. both a and b are correct – d. neither a and b are correct • 8. During the (C) circulation portion of the ACLS survey, the following actions are carried out: – a. look, listen, and feel – b. Obtain IV access, Attach ECG leads, monitor rhythm, given medications to manage rhythm, give IV/IO fluids if needed – c. Obtain IV access, give supplemental oxygen, secure the advanced airway, give IV/IO fluids if needed – d. Check a pulse, monitor heart rhythm, begin CPR if indicated • 10. In the Final Portion of the ACLS survey, the D stands for: – a. defibrillation – b. definitive care – c. differential diagonosis – d. discuss options • 11. Which of the following best describes how to select the proper size of an (OPA) oropharyngeal airway? – a. one size fits all – b. the OPA should be the length of the patients middle finger – c. the OPA should be the length from the corner of the mouth to the angle of the mandible. – d. the OPA should be the length from the patients nose to the ear lobe Bradycardia • 1. What is the drug of first choice for symptomatic bradycardia? – a. atropine – b. lidocaine – c. epinephrine – . vasopressin • 2. Which ECG rhythm is commonly associated with bradycardia? – a. PEA – b. Mobitz II – c. ventricular fibrillation – d. sinus rhythm • 3. What is generally considered the most important and clinically significant degree of block? – a. type I (Mobitz I) – b. type II (Mobitz II) – c. third-degree AV block – d. first-degree AV block • 4. Which drugs are involved in the Bradycardia Algorithm? – a. atropine, epinephrine, dopamine – b. atropine, norepinephrine, dopamine – c. atropine, lidocaine, adenosine – d. atropine, epinephrine, lidocaine • 5. Bradyarrhythmia is defined as: – a. any rhythm disorder with a heart rate less than 40 beats per minute – b. any rhythm disorder with a heart rate less than 60 beats per minute – c. any symptomatic rhythm disorder with a heart rate less than 50 beats per minute – d. any rhythm disorder with a heart rate less than 50 beats per minute • 6. Symptomatic bradycardia exists when_________. – a. the heart rate is slow – b. the patient has symptoms – c. the symptoms are due to a slow heart rate – d. all of the above are needed for symptomatic bradycardia to exist. • 7. Symptoms of bradycardia can include chest discomfort or pain, shortness of breath, decreased level of consciousness, weakness, fatigue, lightheadedness, dizziness, and presyncope or syncope. – True – False • 8. Signs of symptomatic bradycardia include hypotension, orthostatic hypotension, diaphoresis, pulmonary congestion, frequent PVC's or VT. – True – False • . The primary decision point in the bradycardia algorithm is the determination of: – a. heart rate – b. adequate perfusion – c. blood pressure – d. rhythm • 10. After it is determined that the patient does not have adequate perfusion your first step is to: – a. prepare for transcutaneous pacing – b. observe and monitor the paitent – c. give atropine while awaiting transcutaneous pacer – d. use defibrillator set at 200 J Ventricular Fibrillation/Pulseless Ventricular Tachycardia • 1. The primary ACLS treatment for VF and Pulseless VT is: – Lidocaine – high-energy unsynchronized shocks – synchronized shocks – epinephrine • 2. Drugs used in the VF/Pulseless VT Algorithm include: – epinephrine, vasopressin, amiodarone, lidocaine, and magnesium sulfate – epinephrine, vasopressin, atropine, and magnesium sulfate – epinephrine, vasopressin, adenosine, betablockers, magnesium sulfate – epinephrine, vasopressin, amiodarone, lidocaine, and atropine • 5. (True or False) According to the 2010-2011 Guidelines, chest compressions may be continued while the defibrillator is charging. – True – False • 6. For VF/pulseless VT how many shocks should initially be given? – 1 shock – 3 stacked shocks – none, shocks are not indicated – it depends whether the rhythm is VF or VT • 8. After the first shock in the Pulseless VF/VT you should: – give 1 mg epinephrine IV/IO – immediately resume CPR – check for a pulse – check for a rhythm • 10. If you do not know the effective biphasic dose range for the defibrillator that you are using, you should deliver a first shock and all subsequent shocks for VF / pulseless VT at _________. – 120 – 200 – the lowest energy does that is available – the maximal energy dose that is available • 1. If VF is initially terminated by a shock but recurs later in the resuscitation attempt you should: – shock at the previously successful energy level – increase energy level 20J for subsequent shocks – increase energy level to maximum dose that defibrillator can deliver – use medications to reverse VF • 2. Select the sequence that is in the correct order? – give 3 stacked shocks, 5 cycles CPR, check rhythm, give 1 shock, 5 cycles CPR, after 2nd shock give 1mg epinephrine IV push – give 1 shock, 3 cycles CPR, check rhythm, give 1 shock, 3 cycles CPR, after 2nd shock give 1mg epinephrine IV push – give 1 shock, 5 cycles CPR, check rhythm, give 1 shock, 5 cycles CPR, check rhythm after 2nd shock give 1mg epinephrine IV push – give 1 shock, check rhythm, 5 cycles CPR, give 1 shock, check rhythm, 5 cycles CPR, after 2nd shock give 1mg epinephrine IV push • 3. You have given a patient the 1st shock and CPR for 5 cycles, your next step is to __________. – check breathing – give the patient epinephrine 1 mg IV – check rhythm – give a second shock • 4. You have given a patient the 1st shock, CPR for 5 cycles, and now they have an organized rhythm. Your next step is to ___________. – place the patient in rescue position – start the patient on an antiarrhythmic drug – search for possible causes of the VF/VT – palpate for a pulse • 5. The drug ___________ can be used as a substitute for epinephrine for the first or second dose during resuscitation. – Vasopressin – Adenosine – Atropine – Lidocaine • 6. If during VF/VT after a shock, the rhythm check reveals a __________ rhythm and _______, you then should proceed with the asystole/PEA pathway of the ACLS Pulseless Arrest. – ventricular, no pulse – slow, weak pulse – shockable, strong pulse – nonshockable, no pulse • 9. You have shocked the patient, given 5 cycles of CPR and have done a rhythm check. Now, the patient remains in VT with no pulse. What should you do next: – give the patient a second shock – give the patient 1 mg epinephrine – continue CPR for 5 cycles – consider giving antiarrhythmics • 1. The initial energy dose used during defibrillation is dependent upon ____________. – whether the patient has an internal pacemaker – whether the arrest was witness or unwitnessed – whether the defibrillator is monophasic or biphasic – none of the above • 2. Prior to defibrillation which of the following should be done? – ensure all team members are clear – charge the defibrillator – minimize time delay between chest compressions and shock delivery – all of the above • 3. Epinephrine hydrochloride is used during resuscitation primarily for its alpha-adrenergic effects. Alpha-adrenergic effects include: – increase in coronary blood flow resulting from vasoconstriction – increased cerebral blood flow resulting from vasodilation – increased oxygenation resulting from bronchoconstriction – increased renal blood flow resulting from vasoconstruction • 4. (True or False) Overall vasopressin effects have not been shown to differ from epinephrine with regard to ROSC (return of spontaneous circulation), 24 hour survival, or survival to hospital discharge. – True – False • 5. When treating pulseless VF/VT remember to __________. – ensure full chest recoil – push hard and fast (100/min) – search for treatable contributing factors (H and T's) – all of the above • 6. The H's of treatable contributing factors are: – hypovolemia, hypoxia, hydrogen ion, hypo/hyperkalemia, hypothermia – hypovolemia, hydrogen ion, hypo-/hyperkalemia, hyperglycemia, hypothermia – hypovolemia, hypoxia, hydrogen ion, hypo/hypercalcemia, hypoglycemia, hypothermia – hemophilia, hypoxia, hydrogen ion, hypo/hyperkalemia, hypoglycemia • 7. After the third shock in the pulseless VF/VT algorithm with no change in rhythm/pulse, you should __________. – get a different defibrillator – check for a pulse – consider giving antiarrhythmic drugs – consider giving a beta-blocker • 8. Four important aspects to the Pulseless VF/VT algorithm are: – early defibrillation, effective CPR(hard and fast), secure the airway, establish IV/IO access – stacked shocks with defibrillation, minimize delay in CPR, establish IV/IO access, avoid hyperventilation – use only biphasic defibrillator, avoid hyperventilation, establish IV/IO access, CPR immediately after shock – early defibrillation, atropine after first shock, consider antiarrhythmic use, establish IV/IO access • 9. For the pulseless VF/VT algorithm, the proper first dose of IV Amiodarone is ________. – 150 mg – 300 mg – 200 mg – 100 mg • 10. A second dose of ________IV Amiodarone can be given. – 150 mg – 300 mg – 200 mg – 100 mg Tachycardia • 1. A tachyarrhythmia is defined as "any rhythm other than sinus tachycardia with a rate greater than ______.“ – 60 – 100 – 80 – 150 • 2. (True or False) • Unstable tachycardia exists when the heart rate is too fast for the patient’s clinical condition and the excessive heart rate causes symptoms. – True – False • 3. Symptoms that may be due to tachycardia include all the following except: – shortness of air – facial droop – altered mental status – chest pain • 4. Serious signs or symptoms of tachycardia can include which of the following: – Hypotension – poor peripheral perfusion – acutely altered mental status – acute heart failure – all of the above • 5. Heart rates from _____to_____ (per minute) usually are the result of an underlying process (fever, anemia, blood loss, etc.) and are generally sinus tachycardia. – 90-150 – 100-130 – 150-200 – none of the above • 7. The decision point for performing immediate synchronized cardioversion is: – The patient is unstable and no other reversible causes are identified – The patient's heart rate is greater than 150 – Advised by expert consultation – Adenosine does not convert the patient's rhythm • 8. Tachyarrhythmias respond to cardioversion. Sinus tachycardia will not respond to cardioversion. What will often occur if a shock is delivered with sinus tachycardia? – heart rate decreases – Asystole – heart rate increases – ventricular fibrillation • 9. Which of the following would be considered a tachyarrhythmia if the ventricular rate is greater than 100 ? – atrial flutter – atrial fibrillation – supraventricular tachycardia – all of the above • 10. (True or False) When performing synchronized electrical cardioversion on a patient, the shock will occur at the exact time that you press the "deliver shock button.“ – True – False • 1. Which of the following is not an appropriate initial intervention when addressing tachycardia with a pulse? – give oxygen (if hypoxemic) – monitor ECG, blood pressure, and oximetry – identify and treat reversible causes – attempt vagal maneuvers • 2. True or False Tachycardia rates less than 150 per minute usually do not cause serious signs or symptoms. – True – False • 3. Which of the following are key questions that should be addressed during the assessment and management of a patient with tachycardia? – Are symptoms present or absent? – Is the patient stable? – Is the QRS narrow or wide? – Is the rhythm regular or irregular? – All of the above • 4. True or False With tachycardia, if a patient is seriously ill or has significant underlying heart disease or other conditions, symptoms may be present at a lower heart rate? – True – False • 5. If a tachyarrhythmia is causing a patient to become unstable what is the most important intervention? – Cardioversion – IV fluids – expert consultation – antiarrhythmic medications • 6. True or False Unstable Monomorphic VT and Polymorphic VT (with a pulse) are treated with the same interventions? – True – False • 7. Which is the correct treatment for unstable polymorphic VT? – treat as VF with high-energy unsynchronized shocks – treat with 3 stacked shocks – treat with medications only – treat with synchronized cardioversion and an initial shock of 100 J • 8. Which is the correct treatment of unstable monomorphic VT with a pulse ? – treat as VF with high-energy unsynchronized shocks – treat with 3 stacked shocks – treat with medications only – treat with synchronized cardioversion and an initial shock of 100 J • 9. If there is any doubt about whether an unstable patient has monomorphic or polymorphic VT what should you do? – treat with high-energy unsynchronized shocks – treat with 3 stacked shocks – treat with medications only – treat with synchronized cardioversion and an initial shock of 100 J • 10. If the patient is unstable with a narrowcomplex SVT what IV medication can be given as you prepare for immediate synchronized cardioversion? (not shown in unstable pathway but can be given) – amiodarone 150 mg IV – adenosine 6 mg rapid IV push – atropine 1 mg IV – epinephrine 1 mg IV • 1. Which is the correct definition of unsynchronized shock ? – The electrical shock is delivered as soon as the operator pushes the SHOCK button to discharge the machine. The shock can fall randomly anywhere within the cardiac cycle. – The electrical shock is delivered with a peak of the R wave in the QRS Complex thus avoiding the delivery of a shock during cardiac repolarization (twave) • 2. (True or False) Synchronized cardioversion uses a higher energy level than used with unsynchronized cardioversion (defibrillation). – True – False • 3. Low-energy shocks are always delivered synchronized due to the fact that low energy shocks have the potential to produce which rhythm if delivered unsynchronized? – VT – Asystole – VF – atrial flutter • 4. Which of the following cases is unsynchronized shock NOT advised? – for the patient who is pulseless – for a patient who is unstable with polymorphic VT – for a patient who has unstable tachycardia with a pulse – for the patient who is unstable and you are unsure what type of VT exists • 5. According to the new 2010 ACLS Guidelines, how many doses of adenosine rapid IV push can be give with the tachycardia algorithm? –2 –3 –4 –5 • 6. (True or False) Two interventions that can be performed for a regular narrow-complex tachyarrhythmias are vagal maneuvers and adenosine administration? – True – False • 7. Adenosine can be given 2 times to attempt conversion of tachyarrhythmia. What is the recommended dosing schedule? – 12 mg, if no conversion 6 mg – 12 mg, if no conversion 12 mg – 6 mg, if no conversion 12 mg – 6 mg, if no conversion 6 mg • 8. (True or False) Cardioversion is contraindicated for SINUS tachycardia because the increased heart rate is being caused by an external influence such as fever, blood loss, or exercise. – True – False • 9. (True or False) With sinus tachycardia the goal is to identify and treat the underlying systemic causes. – True – False • Adenosine can now be considered for the diagnosis and treatment of stable undifferentiated wide-complex tachycardia when the rhythm is regular and the QRS waveform is monomorphic. – True – False Acute Coronary Syndrome (ACS) • 1. Immediate assessments and actions for a patient presenting with symptoms suggestive of ACS include: – a. oxygen – b. aspirin – c. nitroglycerin – d. morphine – e. 12-lead ECG – f. all of the above • 3. What is the primary focus of treatment of a patient with ACS? – a. Early reperfusion of the STEMI patient – b. Early hospital arrival – c. Early use of medications to prevent plaque formation – d. Assessing family history of coronary artery disease • 4. Which rhythms is most commonly caused by acute myocardial ischemia and is the leading cause of sudden cardiac death? – a. VT – b. Bradycardia – c. SVT – d. VF • 5. Reperfusion therapy may involve which of the following: – a. PCI (percutaneous coronary intervention) – b. fibrinolytic therapy – c. heparin – d. both a and b – e. all of the above • 6. Which of the following drugs are used in the initial treatment of ACS (acute coronary syndrome)? – a. aspirin, morphine, nitroglycerine – b. heparin, metoprolol, aspirin – c. aspirin, fibrinolytics, ACE inhibitors – d. simvastatin, labetalol, oxygen • 8. What is the most common symptom of myocardial ischemia and infarction? – a. discomfort in the retrosternal chest – b. radiating left arm pain – c. jaw pain – d. discomfort in the upper back between the shoulder blades • 9. Other life-threatening conditions that may cause acute chest discomfort are: – a. aortic dissection, acute PE – b. acute pericardial effusion with tamponade – c. tension pneumothroax – d. all of the above • 2. What rhythm is most likely to develop in the first 4 hours after onset of acute coronary syndrome? – a. VT – b. VF – c. atrial flutter – d. PEA • 3. Nitroglycerine should be administered if the patient's systolic blood pressure remains >(greater than) ________ and the heart rate is 50-100/min. – a. 100 – b. 80 – c. 90 – d. 120 • 4. Which pain medication is indicated in STEMI when chest discomfort is unresponsive to nitrates? – a. Motrin – b. morphine – c. dilaudid – d. hydrocodone • 5. (True or False) For the patient with acute coronary syndrome, use of Non-steroidal antiinflammatory drugs (NSAIDs) is contraindicated (excpet for aspirin) and should be discontinued. – True – False • 7. One of the goals of reperfusion therapy is to perform PCI (percutaneous coronary intervention) within ________ minutes of arrival in the ED. – a. 30 minutes – b. 60 minutes – c. 90 minutes – d. 120 minutes • 8. What is the major contraindication to aspirin administration? – a. true aspirin allergy – b. recent GI bleed – c. hypotension – d. fever >100 F (37.7 C) – e. all of the above – f. both a and b • What is the recommended dosage of oral aspirin to be given within the ACS protocol? – 300 mg – 160-325 mg – 80-120 mg – 120-200 mg • 1. Which item(s) below can be used to identify a STEMI? – a. retrosternal chest pain – b. 12-lead EKG – c. troponin – d. all of the above • 2. One goal of reperfusion therapy is to give fibrinolytics within _______minutes of arrival. – a. 60 – b. 20 – c. 30 – d. 90 • 3. (True or False) Morphine is recommended for patients suspected of having ischemic chest discomfort that does not respond to nitrates. – True – False • 4. (True or False) Consultation with a cardiologist should take place before treatment of STEMI. – True – False • 5. Patients with suspected ACS should have oxygen administered if the patient is ___________. – a. dyspenic – b. hypoxemic – c. oxyhemaglobin saturation is < 94% – d. any of the above • 6. The 4 agents that are routinely recommended for consideration in patients with ischemic-type chest discomfort are: – a. aspirin, nitroglycerin, morphine, and oxygen if hypoxemic (o2<94%) – b. motrin, morphine, nitroglycerine, and oxygen if hypoxemic (o2<94%) – c. aspirin, nitroglycerin, dilaudid, and metoprolol – d. epinephrine, dopamine, morphine, and oxygen if hypoxemic (o2<94%) • 7. What is the major contraindication to the administration of nitroglycerine and morphine? – a. recent bleeding – b. changes in level of consciousness – c. chest pain – d. hypotension • 8. For cases in which fibrinolytics are contraindicated, what intervention should be performed? – a. heparin therapy – b. PCI (percutaneous coronary intervention) – c. bypass surgery – d. observation • 9. (True or False) routine use of IV nitroglycerine is not indicated for STEMI and has not been shown to significantly reduce mortality in STEMI. – True – False • Which is a contraindication for the use of nitroglycerin in the ACS protocol? – a. right ventricular infarction – b. hypotension – c. recent phosphodiesterase inhibitor use – d. all of the above PEA / Asystole • The H’s include: – Hypovolemia, Hypoxia, Hydrogen ion (acidosis), Hyper/hypokalemia, Hypoglycemia, Hypothermia. • The T’s include: – Toxins, Tamponade(cardiac),Tension pneumothorax, Thrombosis (coronary and pulmonary), andTrauma. • 1. Some clues for PEA caused by acidosis (hydrogen ion) would be all of the below except: – recent trauma – history of diabetes – renal failure – smaller-amplitude QRS complexes • 2. Recommended treatment to reverse PEA caused by acidosis is: – a. adequate ventilation – b. sodium bicarbonate – c. normal saline bolus – d. both a and b • 3. PEA caused by HYPERkalemia may present with which of the following rhythm changes? – narrow QRS complex, smaller P-waves, and Twaves taller and peaked – wide QRS complex, taller P-waves, and T-waves taller and peaked – wide QRS complex, smaller P-waves, and T-waves taller and peaked – narrow QRS complex, smaller P-waves, and Twaves smaller and rounded Hyperkalemia ecg • • 4. Patients that you might more commonly see with PEA caused by HYPERkalemia are all the followingexcept which one? – renal failure – Diabetes – Elderly – dialysis recipient • 5. Reversing HYPERkalemia is done using which of the following medications? – sodium bicarbonate – glucose and insulin – Albuterol – any of the above • 6. PEA caused by HYPOkalemia may present with which if the following symptoms? – flattened T-waves, prominent U waves, wide QRS, prolonged QT – peaked T-waves, prominent U waves, narrow QRS, prolonged QT – flattened T-waves, prominent U waves, narrow QRS, shortened QT – peaked T-waves, non-visible U waves, wide QRS, prolonged QT • 7. Patients that you might more commonly see with PEA caused by HYPOkalemia are: – diabetic patients – patients using diuretics – patients with chest pain – all of the above • 8. Life threatening hypokalemia is uncommon but can occur in the setting of gastrointestinal and renal losses and is associated with hypomagnesemia. Treatment with magnesium may help during cardiac arrest. – True – False • 9. The “T” that represents drug overdose and chemical exposure among frequent causes of PEA stands for: – Thrombosis – tension pneumothroax – Tamponade – toxins • 10. A clue that PEA could be caused by drug overdose “Toxins” is: – narrow QRS complex – prolonged QT interval – Tachycardia – tracheal deviation