CAROTID ARTERY DISEASE
advertisement

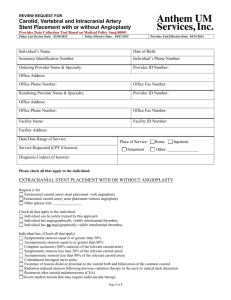
Carotid Artery Disease Lenore C. Ocava, MD Vascular Neurology AECOM/Jacobi Medical Center Anatomy: Transverse Aortic Arch Brachiocephalic trunk or Innominate Artery (1) R common carotid artery R subclavian artery Vertebral artery Left common carotid Artery (2) Left subclavian artery(3) L vertebral artery 1 2 3 True in about 70% Common variant: L CCA originating from innominate artery Anatomy: Common Carotid Artery Located anterolaterally in the neck and medial to the jugular vein The carotid artery, jugular vein, and vagus nerve are enclosed in connective tissue - carotid sheath Terminates as the carotid bifurcation Internal carotid artery (ICA) and External carotid artery (ECA) At the vicinity of the superior border of the thyroid cartilage or approximately at the level of C4 Bifurcation has been described to be as low as T2 and as high as C1. External Carotid Artery smaller of the two terminal branches of the CCA Has 8 branches : the superior thyroid, ascending pharyngeal, lingual, facial, occipital, posterior auricular, and the terminal branches, the superficial temporal, and the internal maxillary artery. The abundant number of anatomoses between the branches of the ECA and the intracranial circulation provides important collateral pathway for cerebral perfusion when significant disease is present in the ICA Internal Carotid Artery The larger of the CCA terminal branches Divided into 4 main segments: Cervical begins at the CCA bifurcation and extends to the base of the skull normally has a slight dilation, termed the carotid bulb and/or the carotid sinus usually does not have branches Petrous - inside the petrous part of the temporal bone Internal Carotid Artery Cavernous invested within the cavernous sinus situated between the layers of the dura mater of the cavernous sinus, but covered by the lining membrane of the sinus Cerebral – begins after the artery perforates the dura matter, passes between the optic and oculomotor nerves, then proceeds to the terminal bifurcation into The Circle of Willis Formed by branches from paired carotid (anterior circulation) and vertebral (posterior circulation) arteries the posterior cerebral, posterior communicating, internal carotid, anterior cerebral, and anterior communicating arteries on each side Allows for “collateral flow” in the setting of atherostenosis or occlusive disease Carotid Artery Disease Vascular layers: adventitia, intima, media Carotid disease is mostly due to atherosclerosis buildup of cholesterol and fibrotic tissue in the arterial wall results from both genetic and environmental influences Caucasians – cervical carotid disease Ethnic minorities – intracranial atherostenosis Other uncommon causes: dissection, vasculitis, fibromuscular dysplasia Evaluation of Patients with Carotid Disease - History Useful information: vascular risk factors focal neurologic deficits transient monocular blindness Likely unrelated events Syncope headache or pain* *except in dissection Evaluation of Patients with Carotid Disease – Carotid Artery Bruit Classic recommendation: assess for the presence of a bruit (CAB – carotid artery bruit) Questions: Does a detectable CAB indicate the presence of a significant lesion? Does the absence of a CAB preclude the presence of a significant lesion? Will the presence of a CAB change further investigation and disposition? Evaluation of Patients with Carotid Disease – Carotid Artery Bruit Hemodynamically significant stenotic lesions may exist in the absence of an audible bruit. The absence of CAB may also signify complete occlusion of the carotid artery. CAB assessment has a sensitivity of 63%-76% and specificity of 61%-76% for clinically significant stenosis* Irrespective of the detection of a CAB in patients with possible vascular events, most authorities would still recommend imaging studies. * Using 70%-99% stenosis on a carotid angiogram as a gold standard threshold Evaluation of Patients with Carotid Disease – Imaging Studies Available Options Carotid duplex US Non invasive, virtually without complications Readily available and quick to do Sensitivity ~70% when compared with angiography CT angiogram – CT with IV contrast, very thin sections Good resolution but requires expertise for interpretation Readily available and quick to do Complications associated with IV dye MR angiogram Good resolution but requires expertise for interpretation Readily available (except in Jacobi) and relatively quick to do Claustrophobia-inducing machine patient required to lie still for about 20-30 minutes Digital subtraction angiography gold standard Invasive Complications related to IV dye 1% stroke risk associated with the procedure Carotid Duplex Ultrasound The degree of stenosis is determined by the velocity of blood flow through the artery the higher the velocity, the greater the degree of stenosis Carotid Duplex Ultrasound Color doppler can demonstrate the area of stenosis with increased flow ( blue/ yellow flow pattern in this image) B-mode can demonstrate the walls of the vessel and the area of stenosis Carotid Duplex Ultrasound Can identify other pathology. Carotid artery dissection - the "false“ channel (yelloworange) is show, distinct from the normal lumen (red). Carotid Duplex Ultrasound: Interpretation Carotid Duplex Ultrasound: Interpretation >70% stenosis with contralateral PSV < 125 cm/sec ICA occlusion: ICA flow velocity may be PSV>125 cm/sec falsely elevated EDV>140 cm/sec Other important information: ICA/CCA (PSV) >4 Occlusion Absence of flow <50% stenosis 50-79% stenosis 80-99% stenosis extent of the plaque plaque characteristics patency of the distal ICA CT Angioram Using a 70% cutoff value for stenosis, CTA compared to DSA agreement in 96% of cases sensitivity 100% specificity 63% negative predictive value was 100% Interobserver agreement was higher for CTAmeasured stenosis than for DSA-measured stenosis Neurology. 2004;63:412-413, 457-460 CT Angioram MR Angiogram 70% to 99% ICA stenoses Time-of-flight MRA Sensitivity 91.2% Specificity 88.3% Contrast-enhanced MRA Sensitivity 94.6% Specificity 91.9% ICA occlusion Time-of-flight MRA Sensitivity 94.5% Specificity 99.3% Contrast-enhanced MRA Sensitivity 99.4% Specificity 99.6% Moderate (50 to 69%) stenoses Time-of-flight MRA Sensitivity 37.9% Specificity 92.1% Contrast-enhanced MRA Sensitivity 65.9% Stroke. 2008;39:2237-2248 Specificity 93.5% MR Angiogram R L Digital Subtraction Angiogram Treatment Strategy #1 stabilize or halt the progression of the carotid plaque Risk Factor Target Comment Hypertension SBP <140 and DBP <90. For patients with diabetes, SBP<130 and DBP <85 Use of ACEIs should be encouraged Diabetes FBS < 126 mg/dL Diet and oral hypoglycemic agents or insulin as needed Elevated lipid levels LDL <100 mg/dL AHA step II diet (<30% fat, <7% saturated fat, < 200mg chol/d) Statin therapy if lipid levels remain elevated Cigarette smoking Stop smoking Counseling, specific therapies Alcohol use Eliminate excessive use Mild to moderate use (1-2 drinks per day) Physical activity 30-60 minutes of exercise at least 3x per week Treatment Strategy #2 eliminate or reduce carotid stenosis Treatment Strategy #2 eliminate or reduce carotid stenosis Carotid endarterectomy (CEA) – treatment of choice Other procedures EC-IC bypass: not beneficial (1980’s) Currently being revisited - Carotid Occlusion Surgery Study (COSS) • aims to identify a subgroup of patients with carotid occlusion that may benefit from EC-IC bypass • ipsilateral increased oxygen extraction fraction (OEF) measured by positron emission tomography (PET) Carotid angioplasty and stenting trials and case series have shown that the outcomes of stenting are worse than or no different from those of carotid endarterectomy Current use limited to patients with high surgical risk preventing the performance of CEA Symptomatic Carotid Stenosis >70% stenosis 2 rate of ipsilateral stroke: 26% in the medical group and 9%in the surgical group* Relative risk reduction 65%* Absolute risk reduction 17%* NNT 7-8 (# patients who would need to undergo endarterectomy to prevent one stroke in a 5-year period)** *,**North American Symptomatic Carotid Endarterectomy Trial (NASCET), the **European Carotid Surgery Trial (ECST), and the trial by the Veterans Affairs Cooperative Studies Program Symptomatic Carotid Stenosis <50% stenosis trials showed that there was no significant benefit of surgery. in NASCET, there was no significant difference in the risk of ipsilateral stroke between those who were treated with endarterectomy and those who were treated medically North American Symptomatic Carotid Endarterectomy Trial (NASCET), the European Carotid Surgery Trial (ECST), and the trial by the Veterans Affairs Cooperative Studies Program Symptomatic Carotid Stenosis Moderate stenosis, 50 to 69% In ECST, there was no significant benefit of surgery for those with moderate stenosis. In NASCET, the 5-year risk of fatal or nonfatal ipsilateral stroke among patients was 22.2% in the medical group and 15.7% in the surgical group Absolute risk reduction 6.5% NNT 15 North American Symptomatic Carotid Endarterectomy Trial (NASCET), and the European Carotid Surgery Trial (ECST) Patients with symptomatic moderate grade stenosis with greatest benefit from CEA more severe stenosis 75 years of age and older men patients with a recent (within 3 months) history of stroke (rather than transient ischemic attacks) as the qualifying event patients with hemispheric TIAs rather than transient monocular blindness radiographic factors: the presence of intracranial stenosis, the absence of microvascular ischemia, and the presence of collateral vessels operative risk experience of the surgeon Asymptomatic Carotid Stenosis the risk of stroke is lower than that associated with symptomatic disease In observational studies, the rate of ipsilateral stroke was 1 to 3% per year among patients with asymptomatic stenosis of greater than 50% the risk in NASCET was 3.2% per year for asymptomatic stenosis of 60 to 99% Asymptomatic Carotid Atherosclerosis Study (ACAS) - >60% stenosis The risk of ipsilateral stroke or any perioperative stroke or death was 5% during 5 years of follow-up in surgically treated patients and 11% in medically treated patients. Absolute risk reduction (ARR) 6% NNT 17 Because of the lower ARR, a rate of perioperative complications (stroke or death) of more than 3% would eliminate the potential benefit of the operation The benefit of surgery was greater for men than women (reduction in risk, 66% vs. 17%) The rate of perioperative complications was higher among women than men (3.6% vs. 1.7%). Risk and Benefit of CE in Women With Symptomatic Carotid Artery Disease With 70% stenosis, the 5-year absolute risk reduction (ARR) in stroke from CE was similar between women (15.1%) and men (17.3%). 30-day perioperative risk of death was higher in women than in men (2.3% versus 0.8%) Higher perioperative risk of stroke and death was also observed in women (7.6% versus 5.9%) but not statistically significant. With 50% to 69% stenosis CE was not beneficial in women (ARR=3.0%), contrary to men (ARR=10.0%). Medically treated women had low risk for stroke Data from NASCET and ACAS Stroke. 2005;36:27 Challenging the Results From ACAS and NASCET Observational study Results (Southern Illinois University School of Medicine ) Surgical death rates were nearly identical for 21-year period asymptomatic and 1,204 CEAs performed symptomatic patients. 464 (39%) in Perioperative stroke rates women were similar for 739 (61%) in men asymptomatic and symptomatic patients. Complete follow-up was available in 70% of Life-table stroke-free rates patients. at 1, 5, and 8 years were similar for asymptomatic women and men and stroke-free survival rates at these follow-up symptomatic women and intervals were greater for asymptomatic men. women compared with men, and for symptomatic women compared to men Ann Surg. 2001 October; 234(4): 438–446 Case #1 L L IM 2008 IM 2010 Case#1 L JR Case #2 L JR DA Case #3 L DA