Kribriformní adenokarcinom jazyka
advertisement

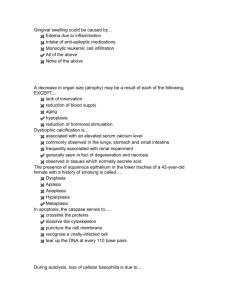
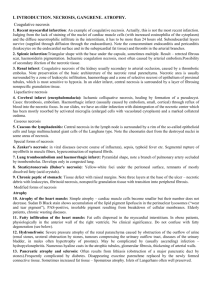
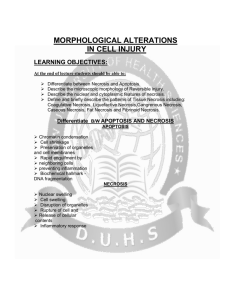
Cell injury:necrosis, apoptosis. Adaptations:atrophy, hypertrophy,hyperplasia. Metaplasia. 2011 DEFINITIONS OF BASIC ASPECTS OF DISEASE PROCESS epidemiology (occurrence and incidence of d.) etiology (causes of disease) pathogenesis (mechanisms of disease) morphology of the tissue changes clinical significance and consequences classification of diseases congenital- present at birth, even though they are sometimes recognized later acquired- occur only later after births (infectious, nutritional, chemical, physical, radiation injury etc.) CELL INJURY Causes of cell injury heterogeneous, range from gross mechanical external causes to mild endogenous causes as genetic lack of enzymes etc. Normal cell is confined to relatively narrow range of functions and structure by its genetic program to handle normal physiologic demands homeostastatic „steady„ state Cells react to adverse influence by adapting sustaining reversible injury suffering irreversible cellular injury- cell death cellular adaptation More excessive stimuli (either physiologic or pathologic) Cellular adaptation altered steady state excessive work stress causes the increase in muscle mass that reflects the increase in size of the individual muscle fiber - higher level of metabolic activity -new equilibrium adaptive response, in which there is a decrease in the size and function of the cells hypertrophy vascular atrophy- results from slow long-lasting decrease of blood supply If the limits of adaptive mechanisms are exceeded or when no adaptive response is possible- cell injury Cell injury Reversible cell injury denotes pathologic changes that can be reversed when the stimulus is removed and the cellular injury has been mild. Cell injury is reversible- up to certain point. Irreversible cell injury denotes pathologic changes that are permanent and cause cell death, cannot be reversed to normal state Cell death Cell death Cell death Necrosis defined as the morphologic changes that following the cell death in a living tissue or organ resulting from the progressive degradative activity of catalytic enzymes on lethally injured cells These enzymes are derived either from dying cells themselves-autolysis or from lysosomal enzymes of leukocytes heterolysis COAGULATIVE NECROSIS most common pattern hypoxic death- results from sudden severe ischemia Coagulative necrosis implies preservation of the basic outline of coagulated cells for several days nucleus usually disappears, but the shape of cell is preserved best example of coagulative necrosismyocardial infarction Coagulative necrosis Myocardial infarct Histological hallmarks of myocardial infarction: Thin, wavy and hypereosinophilic cardiomyocytes lacking nuclei and inflammatory infiltration of the interstitium Coagulative necrosis Kidney infarct Necrotic tissue Viable tissue necrosis Demarcation line Coagulative necrosis Infarct of the spleen LIQUEFACTIVE NECROSIS results from rapid action of hydrolytic enzymes characteristic of ischemic necrosis of brain, pancreas also common in bacterial lesions autolysis and heterolysis prevail over denaturation of proteins -due to activity of enzymes of bacterial and leukocytic origin good example of liquefactive necrosis is brain infarction gross morphology very soft and fluidly, tissue liquefaction results in subsequent pseudocystic degeneration no fibrous scar is formed, necrotic area changes into postmalatic pseudocyst (postnecrotic) Liquefactive necrosis Encephalomalacia (liquefactive necrosis of the brain) and the resulting postmalatic pseudocyst FAT NECROSIS due to action of activated lipases acute pancreatic necrosis, in which active pancreatic enzymes cause focal necrosis of the pancreas and the adipose tissue throughout the abdomen lipases are activated and released and destroy not only pancreatic tissue itself but also fat cells in the pancreas and also fat cells throughout the peritoneal cavity Balser necrosis sharply circumscribed foci of enzymatic necroses of fat tissue with shadowy outlines surrounded by a zone of inflammation Liquefactive necrosis So-called Balser´s necrosis of pancreatic and peripancreatic fat Shadows of dead fat cell that have undergone enzymatic necrosis Viable pancreatic glandular tissue CASEOUS NECROSIS in tuberculosis Gross morphology it appears grossly as soft, friable, whitish-gray debris resembling cheesy material -caseous necrosis Histologically, caseous necrosis appears as amorphous eosinophilic material with cell debris specific granulomatous inflammatory reaction Composed of epithelioid histiocytes giant cells of Langhans type lymphocytes Caseous necrosis Yellow „cheesy“ areas of caseous necrosis in TBC lymphadenitis GANGRENOUS NECROSIS dry gangrene- black and dry and is sharply demarcated from viable tissue in extremities as a result of ischemic coagulative necrosis doe to arterial obstruction wet gangrene- results from severe bacterial infection extremities due to arterial obstruction, in acute suppurative appendicitis tissue is swollen, reddish-black with extensive liquefaction wet gangrene is severe complication associated with high mortality rate gas gangrene- is a wound infection caused by Clostridium perfringens extensive necrosis, tissue destruction, and production of gas by fermentative action of bacteria presence of gas in tissues -crepitus associated with a high mortality rate Healing of necrosis regeneration necrosis scar postnecrotic pseudocyst Cellular adaptation and repair Atrophy Reduction in size of a previously normal organ As opposed to: Hypoplasia: insufficient growth of the organ during its development Aplasia: inborn lack of the organ Agenesis: inborn lack of the primordium of the organ Atrophy under pathologic conditions-pathologic adaptation There are four main adaptive states: atrophy- shrinkage of the organ as a result of decreased cell size or/and the cell number hypertrophy - enlargement of the organ as a result of increased cell size hyperplasia - enlargement of the organ as a result of increased cell number metaplasia -the replacement of one cell type by another cell type in a tissue or organ Vascular atrophy of the kidney is caused by a long standing gradual incomplete narrowing of the renal artery Brown atrophy of the liver is an example of senile atrophy Aging Diminution of cells Accumulation of lipofuscin in cells due to its poor solubility during their aging Brown atrophy Hydronephrosis is an example of mechanical atrophy due to compression of the renal parenchyma by dilated pelvis (e. g. in the setting of urolithiasis) Normal kidney Dilated calyces in moderate hydronephrosis Severe hydronephrosis Renal parenchyma Flattened papilla Dilated calyx Histological hallmark of hydronephrosis is flattening of the renal papilla. On higher power you can see glomerular and tubular atrophy Hypertrophy and hyperplasia Hypertrophy: enlargement of an organ due to enlargement of its cells Hyperplasia: enlargement of an organ due to increase in number of cells Normal Hypertrophy Myocardial hypertrophy is characterized by increased thickness of cardiac walls and increased weight of the heart Myocardial hypertrophy Normal myocardium Enlargement of prostate may be due to: Hyperplasia Adenocarcinoma Hyperplasia Adenocarcinoma Hyperplasia Adenocarcinoma Imunohistochemical staining for HMW cytokeratin 34βE12 Hyperplasia Adenocarcinoma + orchiectomy? TURP Metaplasia Reversible change in which one adult cell type is replaced by another adult Other possible but cell type usually not used differentiation lines Injury Normal line of differentiation Stem cell New line of differentiation Stem cell Metaplasia is an abnormality of cell differentiation in which one type of mature cell is replaced by a different type of adult cell squamous metaplasia n glandular metaplasia nonsquamous columnar or pseudostratified epithelium is replaced by stratified squamous epithelium in uterine cervix, in bronchial mucosa, in nasal cavity and paranasal sinuses occurs in the oesophagus, where the normal epithelium is replaced by glandular mucus secreting epithelium Barret oesophagus Clinical significance: risk of development of peptic ulcer in metaplastic gastric mucosa intestinal metaplasia - occurs often in chronic gastritis Metaplasia only rarely occurs in mesenchymal tissue: osseous metaplasia - in scars