Cellular Biology
advertisement
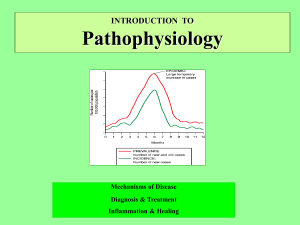
Innate Immunity: Inflammation Chapter 6 Immunity First line of defense Second line of defense Innate resistance – physical (skin/epithelial layer, GI & Resp Tract), , mechanical (Cough, sneeze, vomit, cilia action in trachea) & biochemical barriers (antimicrobial peptides, lung secretions, mucus, saliva, tears, earwax) Inflammation – vascular response – dilation, histamines increase vessel leakage, wbc action, cytokines, leucokines, fever. Usually redness and heat with swelling. Third line of defense Adaptive (acquired) immunity – antibody production First Line of Defense Physical and mechanical barriers Skin Linings of the gastrointestinal, genitourinary, and respiratory tracts Sloughing off of cells Coughing and sneezing Flushing Vomiting Mucus and cilia First Line of Defense Biochemical barriers Synthesized and secreted saliva, tears, earwax, sweat, and sebum Antimicrobial peptides Cathelicidins, defensins, and collectins Normal bacterial flora Second Line of Defense Inflammatory response Caused by a variety of materials Infection, mechanical damage, ischemia, nutrient deprivation, temperature extremes, radiation, etc. Local manifestations Vascular response Blood vessel dilation, increased vascular permeability and leakage, white blood cell adherence to the inner walls of the vessels and migration through the vessels Inflammation Goals Limit and control the inflammatory process Prevent and limit infection and further damage Interact with components of the adaptive immune system Prepare the area of injury for healing Plasma Protein Systems Protein systems Complement system Coagulation system Kinin system All contain inactive enzymes (proenzymes) Sequentially activated First proenzyme is converted to an active enzyme Substrate of the activated enzyme becomes the next component in the series Plasma Protein Systems Complement system Can destroy pathogens directly Activates or collaborates with every other component of the inflammatory response Pathways Classical Lectin Alternative Plasma Protein Systems Coagulation (clotting) system Forms a fibrinous meshwork at an injured or inflamed site Prevents the spread of infection Keeps microorganisms and foreign bodies at the site of greatest inflammatory cell activity Forms a clot that stops bleeding Provides a framework for repair and healing Main substance is an insoluble protein called fibrin Plasma Protein Systems Kinin system Functions to activate and assist inflammatory cells Primary kinin is bradykinin Causes dilation of blood vessels, pain, smooth muscle contraction, vascular permeability, and leukocyte chemotaxis Plasma Protein Systems Plasma Protein Systems Cellular Mediators of Inflammation Cellular components Granulocytes, platelets, monocytes, and lymphocytes Cell surface receptors Pattern recognition receptors (PRRs) Pathogen-associated molecular patterns (PAMPs) Toll-like receptors Complement receptors Scavenger receptors Mast Cells Cellular bags of granules located in the loose connective tissues close to blood vessels Skin, digestive lining, and respiratory tract Activation Physical injury, chemical agents, immunologic processes, and toll-like receptors Chemical release in two ways Degranulation and synthesis of lipid-derived chemical mediators Mast Cell Degranulation Histamine Vasoactive amine that causes temporary, rapid constriction of the large blood vessels and the dilation of the postcapillary venules Retraction of endothelial cells lining the capillaries Receptors H1 receptor (proinflammatory) H2 receptor (anti-inflammatory) Histamine Receptors H1 receptor Proinflammatory Present in smooth muscle cells of the bronchi H2 receptor Anti-inflammatory Present on parietal cells of the stomach mucosa Induces the secretion of gastric acid Mast Cell Degranulation Chemotactic factors Neutrophil chemotactic factor Attracts neutrophils Eosinophil chemotactic factor of anaphylaxis (ECF-A) Attracts eosinophils Mast Cell Synthesis of Mediators Leukotrienes Prostaglandins Product of arachidonic acid from mast cell membranes Similar effects to histamine in later stages Similar effects to leukotrienes; they also induce pain Platelet-activating factor Similar effect to leukotrienes and platelet activation Mast Cells Mast Cells Mast Cells Phagocytosis Process by which a cell ingests and disposes of foreign material Production of adhesion molecules Margination (pavementing) Adherence of leukocytes to endothelial cells Diapedesis Emigration of cells through the endothelial junctions Phagocytosis Phagocytosis Steps Opsonization, recognition, and adherence Engulfment Phagosome formation Fusion with lysosomal granules Destruction of the target Phagocytes Neutrophils Also referred to as polymorphonuclear neutrophils (PMNs) Predominate in early inflammatory responses Ingest bacteria, dead cells, and cellular debris Cells are short lived and become a component of the purulent exudate Phagocytes Monocytes and macrophages Monocytes are produced in the bone marrow, enter the circulation, and migrate to the inflammatory site, where they develop into macrophages Macrophages typically arrive at the inflammatory site 3 to 7 days after neutrophils Macrophage activation results in increased size, plasma membrane area, glucose metabolism, number of lysosomes, and secretory products Monocytes and Macrophages Phagocytes Eosinophils Mildly phagocytic Duties Defense against parasites and regulation of vascular mediators Phagocytes Natural killer (NK) cells Function is to recognize and eliminate cells infected with viruses and some function in eliminating cancer cells Platelets Activation results in degranulation and interaction with components of the coagulation system Cytokines Interleukins Produced primarily by macrophages and lymphocytes in response to a pathogen or stimulation by other products of inflammation Many types Examples IL-1 is a proinflammatory cytokine IL-10 is an anti-inflammatory cytokine Cytokines Interferon Protects against viral infections Produced and released by virally infected host cells in response to viral double-stranded RNA Types IFN-alpha and IFN-beta Induce production of antiviral proteins IFN-gamma Increases microbiocidal activity of macrophages Cytokines Cytokines Tumor necrosis factor–alpha Secreted by macrophages in response to PAMP and toll-like receptor recognition Induces fever by acting as an endogenous pyrogen Increases synthesis of inflammatory serum proteins Causes muscle wasting (cachexia) and intravascular thrombosis Cytokines Local Manifestations of Inflammation Results from vascular changes and corresponding leakage of circulating components into the tissue Heat Redness Swelling Pain Exudative Fluids Serous exudate Fibrinous exudate Thick, clotted exudate: indicates more advanced inflammation Purulent exudate Watery exudate: indicates early inflammation Pus: indicates a bacterial infection Hemorrhagic exudate Exudate contains blood: indicates bleeding Systemic Manifestations of Inflammation Fever Leukocytosis Caused by exogenous and endogenous pyrogens Act directly on the hypothalamus Increased numbers of circulating leukocytes Increased plasma protein synthesis Acute-phase reactants C-reactive protein, fibrinogen, haptoglobin, amyloid, ceruloplasmin, etc. Chronic Inflammation Inflammation lasting 2 weeks or longer Often related to an unsuccessful acute inflammatory response Other causes of chronic inflammation: High lipid and wax content of a microorganism Ability to survive inside the macrophage Toxins Chemicals, particulate matter, or physical irritants Chronic Inflammation Chronic Inflammation Characteristics Dense infiltration of lymphocytes and macrophages Granuloma formation Epithelioid cell formation Giant cell formation Resolution and Repair Regeneration Resolution Returning injured tissue to the original structure and function Repair Replacement of destroyed tissue with scar tissue Scar tissue Composed primarily of collagen to restore the tensile strength of the tissue Resolution and Repair Débridement Cleaning up the dissolved clots, microorganisms, erythrocytes, and dead tissue cells Healing Filling in the wound Sealing the wound (epithelialization) Shrinking the wound (contraction) Healing Primary intention Wounds that heal under conditions of minimal tissue loss Secondary intention Wounds that require a great deal more tissue replacement Open wound Healing Reconstructive phase Fibroblast proliferation Collagen synthesis Epithelialization Contraction Myofibroblasts Cellular differentiation Healing Maturation phase Continuation of cellular differentiation Scar tissue formation Scar remodeling Healing Dysfunctional Wound Healing Dysfunction during inflammatory response Hemorrhage Fibrous adhesion Infection Excess scar formation Wound sepsis Hypovolemia Hypoproteinemia Anti-inflammatory steroids Dysfunctional Wound Healing Dysfunctional during reconstructive phase Impaired collagen matrix assembly Impaired epithelialization Keloid scar Hypertrophic scar Anti-inflammatory steroids, hypoxemia, and nutritional deficiencies Impaired contraction Contracture Dysfunctional Wound Healing Dysfunctional Wound Healing Wound disruption Dehiscence Wound pulls apart at the suture line Excessive strain and obesity are causes Increases risk of wound sepsis Pediatrics Neonates have transiently depressed inflammatory and immune function Neutrophils are not capable of efficient chemotaxis Neonates express complement deficiency Deficient in collectins and collectin-like proteins Elderly Impaired inflammation is likely a result of chronic illness Diabetes, cardiovascular disease, etc. Chronic medication intake decreases the inflammatory response Healing response is diminished due to loss of the regenerative ability of the skin Infections are more common in the elderly