ROM is to 4 SOI is to 4
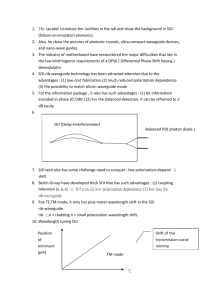
advertisement

3rd Annual Association of Clinical Documentation Improvement Specialists Conference The Power of Case Studies: Death Review and SOI/ROM Cheryl Ericson, MS, RN Manager of Clinical Documentation Integrity & Utilization Review Medical University of South Carolina (MUSC) Medical University of South Carolina • Academic medical center • Located in Charleston, SC • Licensed for 709 beds – Ashley River Tower – Main Hospital – Children’s Hospital • Approximately 40,000 discharges in 2009 Clinical documentation program • Initiated in 2005 – Three staff including the manager – Used consultants through 2007 • Current staffing – Eight FTE and one manager – Registered nurses without coding credentials – Split between two buildings • Ashley River Tower • Main Hospital Clinical documentation program • Primary duty is revenue capture • Only department that queries physicians – Coding does not query physicians • No additional duties related to quality measures, case management, etc. • Follow records to billing – Primarily conduct concurrent reviews – Discharge reviews – Few retro-reviews Reporting structure • CDI reports to the director of health information services (HIS) and patient access services (PAS) – HIS manager is over the coding department • One coding supervisor – CDI manager and HIS manager of equal status • Director of HIS/PAS reports to the chief financial officer (CFO) Challenge: Take CDI to the next level • New management, May 2008 – Tasked with taking CDI to the next level – CDI processes were unchanged since the department was established • MS-DRGs introduced October 2007 – Limited physician support and little physician education outreach – Focused on diagnosis clarification • Urosepsis, CHF, anemia, etc. Challenge: Physician engagement • Administrative physicians are interested in the financial impact of the CDI program; however, because hospital reimbursement doesn’t directly affect the medical staff, hospital revenue enhancement may not be enough incentive to elicit the cooperation of the medical staff in CDI activities. Physicians: What’s in it for me? • How did the medical staff view CDI at MUSC? – Many physicians viewed CDI activities/ documentation as a distraction from patient care – Many physicians thought CDI was a documentation “game” – Reimbursement was a dirty word Making the link • Historically, the CDI department at MUSC only focused on revenue enhancement – CC and MCC capture • Under new management, the focus of the CDI department was changed to a focus on improving the overall quality of the documentation regardless of the impact on CC/MCC capture – Introduced the significance of SOI/ROM Making the link • It was important to understand the link between CC and MCC capture rates and the expected mortality index – MS-DRG is a severity-adjusted DRG system, MS = Medicare Severity • MUSC uses the APR Grouper so the severity of illness (SOI) and risk of mortality (ROM) are calculated as part of the coding process APR grouper • Assigns a severity of illness (SOI) score on a scale of 1–4 • • • • 1 = minor 2 = moderate 3 = major 4 = extreme • • • • 1 = minor 2 = moderate 3 = major 4 = extreme • Assigns a risk of mortality (ROM) score on a scale of 1–4 Recognizing the importance of SOI/ROM • The mortality index is the ratio of actual deaths to expected deaths – CC/MCC capture impacts the expected mortality rate • The SOI/ROM scores are a key component in the algorithm used by the University Health Consortium (UHC) to calculate the expected mortality rate – MUSC uses UHC data for comparison with other academic medical centers How is the SOI/ROM determined? • Each diagnosis has its own intrinsic SOI/ROM value of 1–4 • A complex formula is used to calculate the SOI/ ROM of the DRG/case • Basically, in order for the DRG/case to be a 4/4, at least two diagnoses used to calculate the DRG must have a value of 4/4 – In other words, multiple major complicating conditions (MCC) are need to reach a 4/4 Making the link • The strategy for physician education was changed from CC/MCC capture and revenue enhancement to accurately representing their patient’s severity of illness and risk of mortality. • Basically, we challenged the assertion that MUSC physicians treat the “sickest of the sick” Making the link • CDI shifted focus from revenue to quality, with revenue enhancement as a byproduct – SOI/ROM scores were included on working DRG documentation – CDI staff began issuing “educational” queries • Queries that could result in an additional CC or MCC that may impact SOI/ROM but would not impact the current level of reimbursement Why focus on the mortality index • MUSC is a Studer® hospital • Studer® hospitals use five pillar goals to measure the success of the facility • The Quality Pillar at MUSC is measured by the mortality index – This pillar goal was unmet in 2008 and 2009 Mortality index prior to education Comparison data 4th Quarter 2008 MUSC data 4th Quarter 2008 • At the UHC median – middle of the pack in comparison to other academic medical centers • Significantly below the benchmark (0.83 for the year), which represents top quartile • Just barely below 1.0 for the mortality index – want to be as much below 1.0 as possible Implementing the strategy • The CDI staff at MUSC was successful at identifying diagnoses that required additional specificity to capture a CC or MCC (i.e., incomplete diagnoses such as CHF, anemia, urosepsis, etc.), but a successful CDI program also identifies missing diagnoses. The next step • Find a way to identify missing diagnoses • How do you know if/which records are potentially missing diagnoses? Assumption • Deaths should have a severity of illness (SOI) of extreme/4 and a risk of mortality (ROM) of extreme/4 • A focused review was conducted on deaths that occurred over the past year without a SOI/ROM 7 – Where the SOI/ROM was not 3/4 or 4/3 or 4/4 Outcome • Reviewing deaths that aren’t 4/4 revealed certain trends in physician documentation at MUSC – Identified many opportunities for CC/MCC capture – Identified types of patients that negatively impacted the mortality index • Hospice patients • Short-stay deaths • Nonviable neonates Outcome The CDI program was able to: • Generate a list of diagnoses that were supported by medical evidence but undocumented by the medical staff • “Translate” terms used by physicians into diagnoses that could be captured by coding Educational tools Initial phase • Educate the CDI and coding staff regarding the importance of reviewing all deaths without a SOI/ROM of 4/4 – We found that 3/4 and 4/3 were not strict enough criteria • Implemented a process where all deaths without a 4/4 are reviewed by CDI staff upon discharge – Non-DRG payers are referred to CDI by coding Education • Develop educational tools • Presentations are requested by the individual service lines or departments and are tailored to that particular service line to emphasize relevance to the medical staff – Neurosciences – Heart and vascular – Digestive disease center Sample of Physician Educations Short-stay death Diagnoses: Etiology of stated symptoms? Respiratory diagnoses? Encoder demonstration Added ABLA – no change Added hemorrhagic shock ROM is to 4 SOI is to 4 Added hemorrhagic shock & respiratory failure due to shock ROM is to 4 SOI is to 4 Added coma = Mental status? ROM is to 4 SOI is to 4 Key discussion points There are several diagnoses that were supported by medical evidence but not documented in the medical record that could have moved the SOI/ROM •Emphasize a body system review – Avoid focusing only on specialty area •Provide a rationale/diagnosis for all procedures Short-stay death SOI= 3 ROM = 2 Short-stay death – Suspected location of bleed? – Evidence of hypovolemic/hemorrhagic shock secondary to GI bleed? – Level of consciousness? – Respiratory status? Potential diagnoses? – Translate these findings into diagnoses • • • • • “Not having any spontaneous respirations” “Unresponsive” Hemoglobin 6.7, hematocrit 9/7 ABG results Totality of the symptoms Diagnoses? Encoder demonstration Revised w/ hemorrhagic shock ROM is to 3 Revised w/ acute respiratory failure ROM is to 4 SOI is to 4 Translation of ‘unresponsive’ Revised w/ coma ROM is to 4 SOI is to 4 The value of physician documentation • When presenting death cases, especially those with a long length of stay, ask how much documentation occurs on these patients (e.g., how many pages of progress notes). Physicians are often surprised to learn that pages and pages of documentation may result in only a few diagnoses that can be coded. Service Line Education Mortality index • The goal is for the expected mortality rate (yellow line) to ALWAYS be higher than the observed mortality rate with increasing separation • The observed mortality rate should be on a steadily rising incline as physician documentation improves Potential problem DRG Base MS-DRG 84 Major cardiovascular procedures – adults MS-DRG 238 (w/o MCC) It is important to note the cases we will be discussing occurred in a MS-DRG associated with “healthy” patients – those without a major complication and comorbidity (MCC) rather than in the MS-DRG assigned to the “sickest of the sick” (i.e., those with an MCC). Therefore, deaths are not expected to occur within this MS-DRG. Distribution by procedure Problematic procedures One death occurred in seven cases = 14% One death occurred in 11 cases = 9% Non-deaths need to be maximized to offset the deaths, but it is always problematic when deaths occur in “healthy” tiers (i.e., w/o MCC) Actual case from UHC Encoder results APR-DRG grouper • The SOI of major/3 is captured because two diagnoses have a value of SOI = 3 • Because there is only one diagnosis with an ROM value of 3, the ROM of major/3 cannot be captured for the diagnosis Discharge summary Evidence of additional diagnoses: Cardiogenic shock The 4/4 of cardiogenic shock is not sufficient to move it to 4/4 Review of systems • No documentation regarding respiratory function • No documentation regarding level of consciousness/neurological status Maximized SOI/ROM The Impact of Physician Cooperation Change in mortality ranking • In 4th Quarter 2008, MUSC was at the median compared to other academic medical centers in the University Health Consortium (UHC) database • MUSC uses pillar goals to monitor our success, and the mortality index was an unmet pillar goal in 2009 – The goal was a ratio of 0.80; our value was 0.98 for the year Current mortality index Current medical mortality index Current surgical mortality index Comparison data 3rd Quarter 2009 Change in mortality ranking • In less than a year, MUSC has improved its annual comparison ranking from 57th to 35th – It will take up to four quarters for the impact of process changes to be realized – The current quarterly ranking for MUSC is 22nd, so the annual ranking is expected to continue to rise Change in mortality ranking • In less than a year, MUSC has dramatically reduced its annual mortality rate from 0.98 to 0.83 – It will take up to four quarters for the impact of process changes to be realized – The current quarterly rate for MUSC is 0.74, so the annual value is expected to continue to decrease Risk of mortality distribution Percentage ROM Distribution 100% 95% 90% 85% 80% 75% 70% 65% 60% 55% 50% 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% 1st 08 2nd 08 3rd 08 4th 08 1st 09 2nd 09 3rd 09 4th 09 Quarter ROM Minor = 1 ROM Moderate = 2 ROM Major = 3 ROM Extreme =4 A closer look Percentage ROM Distribution 100% 98% 96% 94% 92% 90% 88% 86% 84% 82% 80% 78% 76% 74% 72% 70% 68% 66% 64% 62% 60% 58% 56% 54% 52% 50% 1st 08 2nd 08 3rd 08 4th 08 1st 09 2nd 09 3rd 09 4th 09 Quarter ROM Minor = 1 ROM Moderate = 2 ROM Major = 3 ROM Extreme =4 MUSC ROM = Extreme Risk of Mortality = Extreme Percent 7.00 6.50 6.00 5.50 5.00 4.50 4.00 1st 2008 2nd 2008 3rd 2008 4th 2008 1st 2009 2nd 2009 Quarter ROM=4 Benchmark 3rd 2009 Severity of illness distribution SOI Distribution 100% 90% 80% Percentage 70% 60% 50% 40% 30% 20% 10% 0% 1st 08 2nd 08 3rd 08 4th 08 1st 09 2nd 09 3rd 09 4th 09 Quarter SOI Minor =1 SOI Moderate = 2 SOI Major = 3 SOI Extreme = 4 A closer look SOI Distribution 100% 95% 90% 85% 80% Percentage 75% 70% 65% 60% 55% 50% 45% 40% 35% 30% 25% 20% 1st 08 2nd 08 3rd 08 4th 08 1st 09 2nd 09 3rd 09 4th 09 Quarter SOI Minor =1 SOI Moderate = 2 SOI Major = 3 SOI Extreme = 4 Revenue capture CMI Value Case Mix Index by Quarter 2.15 2.10 2.05 2.00 1.95 1.90 1.85 1.80 1.75 1.70 1.65 1.60 1.55 1.50 1.45 1.40 1.35 2008-1 2008-2 2008-3 2008-4 2009-1 2009-2 2009-3 Quarter Total CMI Medicare CMI Non-Medicare CMI 2009-4 CMI comparison with UHC data CMI Case Mix Index by Quarter 2 1.95 1.9 1.85 1.8 1.75 1.7 1.65 1.6 1.55 1.5 1st 2008 2nd 2008 3rd 2008 4th 2008 1st 2009 MUSC CMI 2nd 2009 UHC Benchmark CMI 3rd 2009 Second phase initiated 1/10 • Ensuring all deaths are 4/4 is only part of the equation; the extremely ill patients who survive have the greatest impact on the expected mortality index • When more patients with 4/4 survive it raises the expected mortality rate and lowers the mortality index Second phase initiated 1/10 • The “sickest of the sick” patients are usually in the ICU – CDI staff perform concurrent review on ICU patients with DRG payers until the SOI/ROM is maximized or transfer out of the ICU – CDI staff round with ICU medical teams • CDI staff also follow hospice patients of DRG payers for SOI/ROM regardless of their location in the hospital The future We anxiously await each quarter of data as it is released by UHC to track our progress and hope we can continue to sustain this growth in CC/MCC capture and decreasing mortality index The goal of the CDI department is to reach the top 10 among academic medical centers Questions? • Questions?