2. Who is served by the WIC program?
advertisement

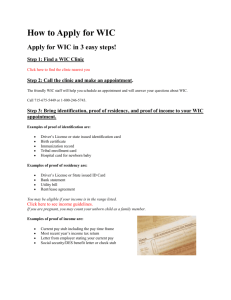
WIC Pre-Rotation Worksheet 1. What does WIC stand for? Women, Infants, and Children 2. Who is served by the WIC program? Federal grants are given to States with the purpose of providing food, nutritional counseling, and health care referrals to low-income pregnant, breastfeeding and non-breastfeeding postpartum women, and infants and children up to age five who are found to be at nutritional risk. These grants fall under the Special Supplemental Nutrition Program for Women, Infants, and Children and is popularly known as WIC. 3. How can a person become a WIC certified? To be eligible for the WIC Program, applicants must meet all of the following eligibility requirements: • Categorical: Women Pregnant (during pregnancy and up to 6 weeks after the birth of the infant or end of the pregnancy) Postpartum (up to 6 months after the birth of the infant or the end of the pregnancy) Breastfeeding (up to the infant’s first birthday) Infants Up to the infant’s first birthday Children Up to the child’s 5th birthday • Residential- must live in the state which you apply • Income- at or below an income level or standard set by the State agency or be determined automatically income-eligible based on participation in certain programs. Income standard: between 100-185% of the Federal Poverty guidelines Automatic Income Eligibility: eligible for SNAP, Medicaid, or TNAF • Nutrition Risk- Health professional determines nutritional risk, usually done in WIC clinic to prevent additional costs to Applicant. Nutritional risk implies the individual has medical-based or dietary-based conditions. Examples of medicalbased conditions include anemia (low blood levels), underweight, or history of poor pregnancy outcome. A dietary-based condition includes, for example, poor diet. 4. Which foods are included as WIC foods in the voucher program? The WIC food packages provide supplemental foods designed to meet the special nutritional needs of low-income pregnant, breastfeeding, non-breastfeeding postpartum women, infants and children up to five years of age who are at nutritional risk. On March 4, 2014, a final rule revising food packages was published. The following table is the maximum monthly allowances (MMA) of supplemental foods for children and women with qualifying conditions in food package III: Foods Juice, Single Strength WIC Formula Milk Breakfast Cereal Cheese Eggs Fruits and Vegetables Whole Wheat or Whole Grain Bread Fish (canned) Legumes, dry and/or peanut butter Children 1-4 Years Old 128 fl oz…………………….. 455 fl oz liquid concentrate 16 qt 36 oz N/A 1 dozen $8.00 in cash-value vouchers 2 lbs N/A 1 lb or 18 oz Women Postpartum (up to 6 months postpartum) Fully breastfeeding, (up to 1 year post-partum) 96 fl oz………………………… 455 fl oz liq concentrate 16 qt 36 oz N/A 1 dozen $10.00 in cash vouchers 144 fl oz…………………… 455 fl oz liq concentrate 24 qt 36 oz 1 lb 2 dozen $10.00 in cash vouchers 1 lb N/A 1 lb N/A 1 lb and 18 oz N/A 1 lb or 18 oz 30 oz 1 lb or 18 oz Pregnant and partially breastfeeding (up to 1 year postpartum) 144 fl oz……………………… 455 fl oz liq concentrate 22 qt 36 oz N/A 1 dozen $10.00 in cash vouchers 5. How is the WIC program funded? Is funding adequate? WIC is not an entitlement program as Congress does not set aside funds to allow every eligible individual to participate in the program. The program receives a finite grant amount each year designated by congress, thus continued support for the program is critical. The WIC program is primarily funded through two separate federal grants: the food grant, and the nutrition services and administration (NSA) grant. • administered at the Federal level by the Food and Nutrition Service (FNS) of the United States Department of Agriculture (USDA) • administered by 90 WIC state agencies, through approximately 47,000 authorized retailers. • WIC operates through 1,900 local agencies in 10,000 clinic sites, in 50 State health departments, 34 Indian Tribal Organizations, the District of Columbia, and five territories (Northern Mariana, American Samoa, Guam, Puerto Rico, and the Virgin Islands). With bipartisan support since 1989, WIC has been funded to meet caseload needs. In order to protect funding, WIC must continue to be efficient, and effective, providing a solid return on investment, and contributing to long-term deficit reduction. The National WIC Association recommends urging Congress to provide a balanced approach that includes mindful, strategic cuts and adequate revenue to resolve the nation’s deficit challenges without harming the range of human needs programs, including WIC. http://www.paramountcommunication.com/nwica/wicfundinghistory.pdf 6. Are states required to partially fund the WIC program? Does North Carolina? Yes. Yes. http://www.urban.org/UploadedPDF/412549-WIC-Participants-and-Their-Growing-Need-for-Coverage.pdf 7. What are the funds used for? To pay for WIC foods, nutrition education, breastfeeding promotion and support, and administration costs. http://www.fns.usda.gov/sites/default/files/WIC-Fact-Sheet.pdf 8. What are the national trends regarding birth outcome according to the National Commission to Prevent Infant Mortality? Infant mortality, deaths to infants during the first year of life (measured as the rate of infant deaths per 1000 live births), has long been understood to be a reflection of how well a society takes care of its most vulnerable members. Infant mortality rates reflect a society’s commitment to the provision of: high quality health care, adequate and nutritionally dense food, safe housing, a healthy psychosocial and physical environment, and sufficient income to prevent impoverishment. Our society’s willingness to commit to the health and welfare of all women, infants and children is paramount to our ability to prevent infant deaths and to address longstanding disparities in infant mortality rates between social classes and ethnic groups. Risk factors for infant mortality include those related to women’s health prior to and during pregnancy, those related to pregnancy, those associated with the birthing process and the environment the newborn enters into, and continue into the first year of life. The ability to reduce infant mortality is dependent on expanding access to: primary care or family planning prior to pregnancy, highquality prenatal care, specialty treatments for preterm or sick infants, breastfeeding support and immunizations, and safe housing and healthy neighborhoods. From 1960 to 1988, the infant mortality rate for the United States decreased by 60% from 26 to 10 infant deaths per 1,000 live births. The causes of death contributing the most were pneumonia and influenza, causes related to hypoxia and asphyxia and causes related to prematurity and low birth weight. The U.S. infant mortality rate has been slowly declining over the past several decades. In 2010, the reported rate was 6.15 deaths per 1,000 live births, and the provisional rate for 2011 was 6.05 per 1,000. The decline is a significant achievement and a result of increasing the availability of life saving neonatal care, increases in access to primary care, and better nutrition. At the same time, racial-ethnic disparities in infant mortality remain, and preventable infant deaths continue to occur. The fact that other industrialized nations average a lower infant mortality rate shows that more can be done. http://www.cdc.gov/nchs/data/series/sr_20/sr20_020acc.pdf http://www.hrsa.gov/advisorycommittees/mchbadvisory/InfantMortality/Correspondence/recommendationsjan2013.pdf 9. What is the infant mortality rate for North Carolina? How does North Carolina compare to other states in the US? 118,983 babies were born alive in 2013. North Carolina's infant mortality rate was tied for the lowest in the state's history. 7.0 babies died in 2013 for every 1,000 born alive. This is down 5.4% from 2012, and a dramatic 44% reduction since 1988 when North Carolina had the highest infant mortality rate in the nation. However, North Carolina continues to exceed the national average. http://nchealthystart.org/infant_mortality/index.htm 10. Which children are most likely to not receive the health care they need according to the National Commission on children? Uninsured children. Those with the lowest incomes face the greatest risk of being uninsured. Being uninsured affects people’s access to needed medical care and their financial security. The access barriers facing uninsured people mean they are less likely to receive preventive care, are more likely to be hospitalized for conditions that could have been prevented, and are more likely to die in the hospital than those with insurance. http://kff.org/uninsured/report/the-uninsured-a-primer/ 11. What was reported by the Committee for Economic Development in “The Unfinished Agenda: A New Vision for Child Development and Education” (1991) for children to reach their learning potential? Abstract from “The Unfinished Agenda: A New Vision for Child Development and Education” “Schools and business must unite to make all the changes needed to ensure the success of all children. Social change, particularly the increase in single-parent families, has resulted in more children being born at risk of school failure. Most early childhood education reform initiatives have been piecemeal and have lacked a true understanding of at-risk children's complex needs. The following imperatives for educational improvement are discussed: (1) the nation needs a comprehensive, coordinated human investment strategy for child development and education; (2) programs should strengthen the entire family; (3) teen parents who have not finished high school should have access to a specialized school that meets their needs; (4) early childhood education should be available to all children; (5) programs must be flexible in design, administration, and funding; (6) successful programs must be broadly replicated; (7) the mission of the public schools must be redefined to account for social changes, including development of clearer goals and more effective methods of measurement to permit accountability; (8) students must take greater responsibility for their own success; (9) business should encourage volunteerism; and (10) business should play a leadership role in identifying strategies and determining what resources are needed. Twenty-four successful programs are highlighted. Statistical data are presented in two tables and one graph. A list of 35 references, 8 dissenting comments, and a list of the objectives of the Committee for Economic Development are appended.” http://www.centerforcsri.org/research/improvement.cgi?st=s&sr=SR000161 12. Why will the government actively save money by having pregnant women participate in the WIC program? Describe quantitative effects. The Institute of Medicine (IOM) estimated that in 2005the average direct cost of medical care for a preterm infant in the United States was more than $30,000, with the majority (85%) of this cost being incurred during the first year of life. The average cost per infant increased to $51,600 when the costs of maternal medical care, early intervention and special education services, and lost household productivity were considered. The annual societal economic burden associated with preterm birth in the United States was in excess of $26 billion in 2005. These costs grow each year with medical care inflation. Moreover, these estimates do not take into account the emotional toll on families who lose a baby or whose infant has adverse consequences. Research has shown that the WIC Program has been playing an important role in improving birth outcomes and containing health care costs. A series of reports published by USDA based on linked 1988 WIC and Medicaid data on over 100,000 births found that every dollar spent on prenatal WIC participation for low-income Medicaid women in 5 States resulted in: longer pregnancies; fewer premature births; lower incidence of moderately low and very low birth weight infants; fewer infant deaths; a greater likelihood of receiving prenatal care; and savings in health care costs from $1.77 to $3.13 within the first 60 days after birth. A summary of sources suggests that: WIC reduces fetal deaths and infant mortality. WIC reduces low birth weight rates and increases the duration of pregnancy. WIC improves the growth of nutritionally at-risk infants and children. WIC decreases the incidence of iron deficiency anemia in children. WIC improves the dietary intake of pregnant and postpartum women and improves weight gain in pregnant women. Pregnant women participating in WIC receive prenatal care earlier. Children enrolled in WIC are more likely to have a regular source of medical care and have more up to date immunizations. WIC helps get children ready to start school: children who receive WIC benefits demonstrate improved intellectual development. WIC significantly improves children’s diets http://www.fns.usda.gov/wic/about-wic-how-wic-helps#Improved Birth Outcomes and Savings in Health Care Costs 13. What where the overall effects of the WIC program according to the extensive multi-year medical evaluation supported by USDA in 1986. A series of medical evaluations have found striking results that WIC improves the health of participating women, infants and children. Most significant is an extensive, multi-year medical evaluation supported by the U.S. Department of Agriculture and issued in 1986. Directed by Dr. David Rush, one of the nation's leading researchers in the field, the evaluation found that: 1. WIC contributed to a reduction of 20 to 33.33 percent in the late fetal death rate. 2. WIC significantly increased the head size of infants whose mothers received WIC foods during pregnancy. Head size normally reflects brain growth. 3. Women who participated in WIC had longer pregnancies leading to fewer premature births. There was a 23 percent decrease in prematurity among white women with less than a high school education and a 15 percent decrease among black women with less than a high school education. Premature births are one of the leading causes of deaths among infants. 4. WIC participation resulted in a significant increase in the number of women seeking prenatal care early in pregnancy and a significant drop in the proportion of women with too few prenatal visits to a health facility. Early and adequate prenatal care is one of the major factors affecting the health of newborn infants. 5. WIC participation also appears to lead to better cognitive performance. Four and five year olds whose mothers participated in WIC during pregnancy had better vocabulary test scores. Children who participated in WIC after their first birthdays had better digit memory test scores. 6. Women enrolled in WIC consumed more of such key nutrients as iron, protein, calcium, and vitamin C. 7. WIC also improved the diets of infants by increasing the average intake of iron and vitamin C and significantly diminishing the frequency of low consumption of iron and vitamins A and C. WIC improved the diets of older preschool children by increasing average consumption of iron, vitamin C, thiamine, and niacin and by significantly decreasing the frequency of low intake of vitamins A and B and riboflavin. 8. The greatest dietary benefits were among those people at highest risk: minority women, women with less education and children who are very poor, short, black, or in female-headed families. 9. Children participating in WIC were better immunized and more likely to have a regular source of medical care. Other studies have also demonstrated that WIC makes a significant contribution to the health of pregnant women and young children. 10. The General Accounting Office (GAO) reviewed all medical research on WIC published and found that the incidence of low birth weight infants born to low income women who have been participating in WIC appears to be reduced by 16 to 20 percent. 11. WIC has a major impact on reducing anemia among children. "The Journal of the American Medical Association" (September 25, 1987) reported findings from the Center for Disease Control's Pediatric Nutrition Surveillance data that showed a two-thirds reduction in childhood anemia over a ten-year period. The study indicated that WIC contributed markedly to the decline. The study found that low income children not enrolled in WIC have a significantly higher prevalence of anemia than those who are enrolled. 12. According to a University of California School of Public Health study, women who participated in WIC for an extended time during the postpartum period had higher mean hemoglobin levels and a lower risk of maternal obesity at the onset of the next pregnancy. Their infants had higher mean birth weights and were at a lower risk of having a low birth weight than were the infants of women who did not participate in the WIC program for an extended time during the postpartum period. 13. A Harvard School of Public Health study found that WIC reduced the incidence of low birth weight and that each $1 spent on the prenatal component of WIC averted $3 in hospitalization costs in the geographical areas under study. 14. A Missouri Department of Health study found that WIC participation was associated with reductions in low birth weight rates and that for every $1 spent on the prenatal component of WIC, about 49 cents in medical costs were saved during the first 45 days after birth. 15. A Mathematical Policy Research study found that for every $1 spent prenatally in WIC, from $1.77 to $3.13 in Medicaid costs were saved during the first 60 days after birth. http://www.houstontx.gov/health/WIC/research.html 14. State the purpose of WIC: To safeguard the health of low-income women, infants, and children up to age 5 who are at nutrition risk by providing nutritious foods to supplement diets, information on healthy eating, and referrals to health care http://www.fns.usda.gov/wic/about-wic-wics-mission 15. List the criteria to participate in WIC. To be eligible for the WIC Program, applicants must meet all of the following eligibility requirements: • Categorical: Women Pregnant (during pregnancy and up to 6 weeks after the birth of the infant or end of the pregnancy) Postpartum (up to 6 months after the birth of the infant or the end of the pregnancy) Breastfeeding (up to the infant’s first birthday) Infants Up to the infant’s first birthday Children Up to the child’s 5th birthday • Residential- must live in the state which you apply • Income- at or below an income level or standard set by the State agency or be determined automatically income-eligible based on participation in certain programs. Income standard: between 100-185% of the Federal Poverty guidelines Automatic Income Eligibility: eligible for SNAP, Medicaid, or TNAF • Nutrition Risk- Health professional determines nutritional risk, usually done in WIC clinic to prevent additional costs to Applicant. Nutritional risk implies the individual has medical-based or dietary-based conditions. Examples of medicalbased conditions include anemia (low blood levels), underweight, or history of poor pregnancy outcome. A dietary-based condition includes, for example, poor diet. 16. What foods does WIC provide for infants (birth – 12 months)? What brands of infant formula are available at your WIC office? How and in what circumstances can infants receive non-contract brands of formula? Food packages include: The food package for fully breastfeeding women provides greater amounts of foods, including a higher dollar value for fruits and vegetables. Fully breastfeeding infants receive baby food meats in addition to greater amounts of baby food fruits and vegetables. Less infant formula is provided to partially breastfeeding infants so that they may receive the benefits of breast milk. A minimal amount of infant formula is provided to partially breastfeeding infants in the first month after birth in order to help mothers build and maintain their milk production. WIC State agencies are responsible for identifying the types and brands of infant formulas that are authorized for use in their WIC Programs. The Federal regulations that govern the WIC Program outline the minimum requirements for WIC-eligible infant formula. WIC State agencies are required to have a competitively bid, sole-source rebate contract with a manufacturer of infant formulas. Under such an agreement, most healthy WIC infants may be provided either a milk-based or soy-based iron-fortified infant formula produced by the manufacturer awarded the contract. In turn, WIC State agencies receive a rebate per can of infant formula issued to a WIC infant. Infants who have special dietary needs are provided an appropriate alternative formula, in accordance with State WIC policies and Federal regulations. WIC rebate contracts and policies vary by State, therefore the types and brands of infant formula will vary by State. Medical documentation is required for the issuance of exempt infant formulas and medical foods. Medical documentation forms for alternate formula or food needs: 17. What foods does WIC provide for women and children? What foods are also available for women who exclusively breastfeed? Pregnant and postpartum women and children (under 5 years of age) participating in WIC receive food benefits for milk, cheese, eggs, cereals, peanut butter, dry beans/peas or canned beans/peas, and fruit or vegetable juices, fresh fruits and vegetables and whole grain choices to include breads, tortillas, brown rice and oatmeal. Women who exclusively breastfeed their babies may also receive extra food, including canned tuna fish. (http://www.michigan.gov/mdch/0,4612,7-132-2942_4910_6329-12667--,00.html) 18. Has WIC been successful? Give specific examples? WIC saves lives and improves the health of nutritionally at-risk women, infants and children. It is one of the most successful Federally-funded nutrition programs in the United States. The findings of studies, reviews and reports concerning WICs efficacy have been shown in questions 12 and 13. The following are more examples of how WIC has benefited its target population: Improved Diet and Diet-Related Outcomes Higher mean intakes of iron, vitamin C, thiamin, niacin and vitamin B6, without an increase in food energy intake, indicating an increase in the nutrient density of the diet Positive effects on the intakes of ten nutrients without an adverse effect on fat or cholesterol More effective than other cash income or SNAP benefits at improving preschoolers' intake of key nutrients Decline in the rate of iron deficiency anemia from 7.8 percent in 1975 to 2.9 percent in 1985 which the Centers for Disease Control and Prevention attributed to both a general improvement in iron nutrition and participation in WIC and other public nutrition programs. Improved Infant Feeding Practices WIC participants who reported having received advice to breastfeed their babies from the WIC clinic were more likely to breastfeed than other WIC participants or eligible nonparticipants; WIC breastfeeding policy and program activities were strengthened in the early 1990's; Between 1996 and 2001, the percentage of WIC mothers breastfeeding in the hospital increased by almost 25 percent, from 46.6 to 58.2 percent The percentage of WIC infants breastfeeding at six months of age increased by 61.2 percent, from 12.9 to 20.8 percent; and, For those infants who are fed infant formula, 90 percent received iron-fortified formula, which is recommended for nearly all nonbreastfed infants for the first year of life. Improved Cognitive Development Improve vocabulary scores for children of mothers who participated in WIC prenatally Significantly improve memory for numbers for children enrolled in WIC after the first year of life. Improved Pre-conception Nutritional Status The women who received postpartum benefits had higher hemoglobin levels and lower risk of maternal obesity at the onset of the subsequent pregnancy. Other Improved Outcomes Increase the likelihood of children having a regular provider of medical care Improve growth rates. http://www.fns.usda.gov/wic/about-wic-how-wic-helps 19. What anthropometric and biochemical data are obtained from WIC participants? How often? For applicants who are being certified, re-certified, or during a current certification period, the following Anthropometric and/or hematological data collected within the WIC agency or contracted agency or provided by referral must be obtained. Anthropometric data includes height/length, weight and head circumference (for infants up to one year of age). The data must have been collected within 60 days prior to the date of certification or recertification and must reflect current health and categorical status. Such data may not be appropriate for pregnant women, or infants and children during critical periods of growth. For women, the data must have been collected while she was in the same status as when being certified or recertified for the WIC Program, regardless of the date the data was obtained. Hematological data includes hemoglobin or hematocrit. The data must have been collected within 90 days prior to the date of certification or recertification or may be deferred for up to 90 days after the date of certification or recertification if the participant has another qualifying risk factor. For all categories, the data must have been collected while in the same status as when being certified or recertified for the WIC Program, exceptions noted. All infants shall have hematological data collected between 9 and 12 months of age. The data must not have been obtained prior to the infant's 6-month birthday. All children must have hematological data collected according to the following guidelines. For children 12-23 months of age, blood work must be taken at least once – recommended at 15-18 months of age, ideally 6 months after the infant blood work. For children 24-60 months of age, blood work must be taken at least once every 12 months if blood test results were within the normal range at last certification. For children 2-5 years of age, blood work must be rechecked at the next recertification visit if blood test results were abnormal. For all postpartum women, the blood work should be taken between 4 and 6 weeks postpartum, as long as another risk factor exists at certification. If no other risk factor exists, a blood test shall be performed. For breastfeeding women being recertified at 6-12 months postpartum, no additional blood test is necessary, as long as she was on the program as an N or B during first six months. However, if the woman had a positive low hemoglobin/low hematocrit screen result when tested after delivery, the CPA should ensure and document that appropriate treatment and follow-up occurred. If no other risk factor exists, including Risk Factor 501(formerly E1), a follow-up blood test is an allowable WIC cost to determine if the low hemoglobin/low hematocrit risk factor still applies. For infants who were certified younger than 6 months of age, one or more infant follow-up visits (quality checks) must be performed during the first year to assure that the quality and accessibility of health care services are not diminished. A record will not be entered into the system. The follow-up visit (quality checks) will include: Anthropometric and/or hematological data collected within the WIC agency or contracted agency or provided by referral. Anthropometric data includes length, weight, and head circumference. http://www.google.com/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&ved=0CCMQFjAA&url=http%3A%2F%2Fhealth.mo. gov%2Fliving%2Ffamilies%2Fwic%2Fwicupdates%2Fdoc%2FER2.02800CertRecertandInfantFollow-upComponents-rev2-2808.doc&ei=7U29VPnYLsHuggShoIOIAQ&usg=AFQjCNEwf3BXeoDnMKRTSrVIZRWeo5NJ8w 20. In order for a food to be WIC approved, it must be a good source of one or more of these nutrients: Foods selected are low in sugar and salt and are good sources of vitamins A, C, and D, iron, protein, and calcium. (http://health.mo.gov/living/families/wic/faqs.php#8) 21. List several high risk indicators for each of the following categories: prenatal women, postpartum women, infants/children. Prenatal: Economic deprivation, smoker, use of drugs, pre-partum weight of less than 85% or more than 120% of desirable BMI for height and age, weight loss during pregnancy or gain of less than 2 pounds per month in the last 2 trimesters, dehydration, hyperemesis Postpartum: Low income, homeless, food insecurity, substance abuse, lack of food and nutrition knowledge Infants/Children: Failure to thrive, protein malnutrition, underweight, inappropriate diet 22. In which class is the WIC participant at the highest risk? Class I or Class VI? Priority levels? Pregnant women, breastfeeding women, and infants determined to be at nutritional risk because of serious medical problems. Infants up to 6 months of age whose mothers participated in WIC or could have participated and had serious medical problems. Children (up to age 5) at nutritional risk because of serious medical problems. Pregnant or breastfeeding women and infants at nutritional risk because of dietary problems (like poor diet). Children (up to age 5) at nutritional risk because of dietary problems. Non-breastfeeding, postpartum women with any nutritional risk. Individuals at nutritional risk only because they are homeless or migrants, and current participants who without WIC foods could continue to have medical and/or dietary problems. http://www.fns.usda.gov/wic/frequently-asked-questions-about-wic#2 23. If a person applying for WIC is already receiving Medicaid or Food Stamps, they are automatically income-qualified for WIC. True or False. True 24. List several ways a WIC participant can become ineligible. If you/child are no longer at risk, if income doesn’t meet guidelines, if you are not postpartum/pregnant/have an infant-child younger than 5. 25. Define LBW. A baby born at how many weeks gestation is considered premature? LBW (low birth weight) is a live infant born weighing less than 5 lbs, 8 ounces, regardless of gestational age. Infants born before 37 weeks are considered premature. Nutritional Formulas Worksheet 1. Give some examples of diseases that alter the metabolism of infants and may require special formulas. Phenylketonuria (PKU): Infants diagnosed with PKU are treated with a special low-phenylalanine formula. Tyrosine is given at approximately 25 mg per kg of weight per day; amino acids are given at about 3 g per kg per day in infancy and 2 g per kg per day in childhood. Infants and children must be monitored regularly during the developmental period, and it is recommended that strict dietary therapy be continued for life. Medium-chain acyl-CoA dehydrogenase (MCAD) deficiency: Babies with MCAD deficiency can’t convert fat into energy. Avoid fasting, supplemental carnitine. Treatment of MCAD deficiency also may include frequent cornstarch feeds. Galactosemia: Restrict Galactose, and lactose. Lactose-free infant formula Ornithine transcarbamylase deficiency- is the most common urea cycle disorder. Acute treatment options include sodium benzoate, sodium phenylacetate, and arginine. Certain persons may benefit from liver transplantation. http://www.aafp.org/afp/2006/0601/p1981.html 2. What does the nutrition plan for an infant’s diet include? Birth to 4 months 4-6 months Suggest starting solids closer to 6 months of age Breast Milk or Infant Formula Cereal, Bread, and Starches Fruits and Vegetables 8-12 feedings 2-6 oz or more per feeding (18-32 oz per day) 4-6 feedings 4-6 oz or more per feeding (27-45oz per day) None None None 2-3 servings of iron fortified baby cereal mixed with breast milk or formula (do not put in bottle or mix with juice) None None Begin to offer plain cooked, mashed or strained baby food vegetables and fruits. Avoid combination meat and vegetable dinners. (2-3TBS) (Stage I & II) 2-4 oz of fruit juice may also be offered at this time in a cup only 2-3 servings daily of soft, cut up, and mashed vegetables and fruits. 3-4 oz of fruit juice in a cup only. (Stage III) None 6-8 months 3-5 feedings 6-8 oz per feeding (24-32 oz per day) 2-3 servings of baby cereal and other soft, cooked breads, cereals and starches (teething biscuits, zweiback toast) 8-10 months 3-4 feedings 7-8 oz per feeding (24-32 oz per day) 2-3 servings daily of baby cereal and other soft, starches 10-12 months 24-32 oz of breast milk or formula per day 4 servings daily of baby cereal, breads, and other starches 4 servings daily of fruits and vegetables(2-3 Tbsp) 3-4 oz of fruit juice in a cup only Meats and Other Protein Foods Begin offer soft, well cooked, finely cut/ pureed meats, cheese and casseroles 1-2 oz daily of soft, finely cut or chopped meat or other protein foods Cow's milk is not recommended by the American Academy of Pediatrics for children under 1 year old. The baby will begin drinking less formula or breast milk once solid foods become a source of nutrition. After a baby has tried a variety of different baby cereals, try strained fruits and vegetables. • For strained fruits and vegetables, introduce one at a time, waiting 2 - 3 days in between to check for any allergic reaction. • Start with plain vegetables such as green peas, potatoes, carrots, sweet potatoes, squash, beans, beets; and plain fruits such as bananas, applesauce, apricots, pears, peaches, and melon. • Some dietitians recommend introducing a few vegetables before fruits, as the fruit's sweetness may make a less-sweet food such as vegetables less appealing. -At 8-12 months of age, Breast milk or formula should be offered three to four times per day.. A baby will be ready to try strained or finely chopped meats. For breastfed infants, start meats at 8 months of age (breast milk is not a rich source of iron, but infants have adequate iron stores to last until 8 months of age when iron-rich foods such as meats can be given). As with other foods, offer only 1 new meat per week in 3 - 4 tablespoon servings -- use strained and finely ground meats, or meat sticks. Serving sizes for fruits and vegetables increases to 3 - 4 tablespoons, four times per day. Eggs may be given 3 - 4 times per week, but only the yolk until the baby is 1 year old, as some babies are sensitive to egg whites. 3. List the steps of making in infant formula (concentrated, powdered and ready to feed)? 1. Check the expiration date and condition of the container 2. Wash your hands. 3. Prepare your bottle Sterilize bottles, nipples, caps and rings before using them for the first time: -Boil the bottle and accessories in water for five minutes. Use a pot that's large enough to hold all of the pieces and cover them completely with water. -Remove the pieces from the water using a clean set of tongs. -Allow the pieces to air-dry. After the first use, there's no need to sterilize your bottle and accessories. Simply wash these items with soap and water and allow them to air-dry. Bottle and nipple brushes can help you clean nooks and crannies. You can also use the dishwasher. If you do so, consider getting a dishwasher-safe basket to hold your utensils. Also, during the cleaning process, make sure the nipples are open. Hold each nipple upside down and fill it with clean water, then look for the water to drip slowly out of the nipple. Remember to clean formula containers, too. Before opening a new container, wash the top with soap and water, then rinse well. If you plan to prepare formula in the bottle, confirm the measuring marks on each bottle. Simply use a liquid measuring cup and water to make sure the measurements on the bottle are accurate. 4. Add water to liquid-concentrate or powdered formula If you're using liquid-concentrate or powdered formula, you'll need to add water to the bottle. Check to see if the manufacturer's instructions specify whether to add water or formula to the bottle first. Typically, you'll add water to the clean bottle first to ensure you're using the proper amount. Follow the manufacturer's instructions for how much water to use. Adding too little water can put a burden on your baby's digestive system, and adding too much water might overly dilute the formula and deprive your baby of calories and nutrients. You can use any type of clean water — tap or bottled — to prepare liquid-concentrate or powdered formula. If you'd like to use tap water but you're concerned about the safety of your water supply or you use private well water, consider sterilizing the water before adding it to the bottle: -Use cold tap water. -Let the cold water run for as long as it takes to get as cold as it gets — up to two minutes. This helps reduce the amount of lead and other contaminants in the water. -Pour the cold water into a clean pan and boil it for one to two minutes. -Let the water cool. -Carefully pour the amount needed. -You might also have well water checked for lead, nitrates and bacteria. It's also important to consider the amount of fluoride in the water you use to prepare your baby's liquid-concentrate or powdered formula. Exposure to fluoride during infancy helps prevent tooth decay during infancy. However, regularly mixing a baby's formula with fluoridated water might increase your child's risk of developing faint white markings or streaks on the teeth — a sign of mild enamel fluorosis. If you're concerned about fluorosis, consider ways to minimize your baby's exposure to fluoride. For example, you might use readyto-feed formula or alternate between tap water and low-fluoride bottled water — such as purified, demineralized, deionized or distilled bottled water — for formula preparation. However, if you feed your baby only ready-to-feed formula or concentrated formula mixed with low-fluoride water, your baby's doctor might recommend fluoride supplements beginning at 6 months. 5. Measure the formula For ready-to-use formula: Shake the container of formula well before opening it. Pour enough formula for one feeding into a clean bottle. Use only formula — don't add water or any other liquid. Attach the nipple and cap and shake well. For liquid-concentrate formula: Shake the container of formula well before opening it. Pour the amount of formula for one serving into the bottle, which already contains the appropriate amount of water. Attach the nipple and cap and shake well. For powdered formula: Use the scoop that came with the formula container. Make sure the scoop is dry. Determine the amount of formula you want to prepare, following instructions on the package. Note the number of scoops you'll need. Fill the scoop with powdered formula, shaving off any excess formula from the top of the scoop with the flat side of a knife not a spoon or other curved surface. Pour the scoop or scoops into the bottle, which already contains the appropriate amount of water. Attach the nipple and cap and shake well. 6. Warm the formula, if needed It's fine to give your baby room temperature or even cold formula. If your baby prefers warm formula: Place a filled bottle in a bowl or pan of hot, but not boiling, water and let it stand for a few minutes — or warm the bottle under running water. Shake the bottle after warming it. Turn the bottle upside down and allow a drop or two of formula to fall on your wrist or the back of your hand. The formula should feel lukewarm — not hot. Don't warm bottles in the microwave. The formula might heat unevenly, creating hot spots that could burn your baby's mouth. Shake the bottle well and feed the formula to your baby immediately. Discard any formula that remains in the bottle after a feeding. 7. Store formula safely Store unopened formula containers in a cool, dry place. Don't store formula containers outdoors or in a car or garage, where temperature extremes can affect the quality of the formula. If you're using ready-to-use formula, cover and refrigerate any leftover formula from a freshly opened container. Discard any leftover formula that's been in the refrigerator more than 48 hours. If you prepare and fill several bottles of liquid-concentrate or powdered formula at once: Label each bottle with the date that the formula was prepared. Refrigerate the extra bottles until you need them — don't freeze them. Put the bottles toward the back of the refrigerator, where it's coldest. Discard any prepared formula that's been in the refrigerator more than 24 to 48 hours. If you're unsure whether a particular container or bottle of formula is safe, throw it out. 4. How much time does it take to prepare a specialized infant formula approximately? Enough time to follow all directions above. Initially more time should be budgeted for preparation until they become more comfortable with the process. 5. Which are the 4 categories of infant formula? Milk-based: This is the most common formula. It has protein and lactose from cow's milk. Hydrolyzed: “Predigested” proteins are easier to digest. Soy: These formulas are sometimes recommended for babies with sensitive stomachs who are unable to digest lactose, the main carbohydrate in milk-based formulas. Soy formulas contain no animal products. Specialized: These formulas are manufactured for infants with specific disorders or diseases, and for babies born preterm. http://similac.com/feeding-nutrition/formula-feeding/best-baby-formula 6. What is the amount of iron in fortified standard formulas? The American Academy of Pediatrics (AAP) recommends that iron-fortified cow’s milk-based infant formula is the most appropriate milk feeding from birth to 12 months for infants who are not breastfed or who are partially breastfed. Use of an iron-fortified infant formula ensures that formula-fed infants receive an adequate amount of iron, an important nutrient during the first year. Standard iron-fortified infant formulas are fortified with approximately 10 to 12 milligrams of iron, in the form of ferrous sulfate, per quart. http://www.nal.usda.gov/wicworks/Topics/FG/Chapter4_InfantFormulaFeeding.pdf 7. Which manufacturers combine demineralized whey with nonfat milk to produce a whey/casein ratio similar to that in human milk? Is there any advantage to this practice? In the belief that altering this ratio may improve digestibility, the standard formulas Enfamil and Similac (Mead Johnson and Abbott) have been adjusted to have casein:whey ratio near 40:60. This excludes the protein in Similac Sensitive, which is all casein. However, some babies (and preemies) may do better with a different product. (http://ons.wvdhhr.org/Portals/20/PDFs/Aunt%20C%20Choosing%20Infant%20Milks%20andFormulas%20Part2%20commercial%20f ormulas%204-12%20THIS.pdf) 8. Which manufacturers produce a modified casein-predominant formula? Similac and Gerber 9. How are soymilk based formulas produced? Soy formula is an infant food made using soy protein and other components. It has no animal ingredients. It is used as a supplement or replacement for human milk or cow milk formulas in infants with allergies or due to other diet restrictions. 10. Under what circumstances should an infant be placed on a soymilk based formula? Pediatricians usually recommend soy formula for those babies who need it, including infants with: • galactosemia • primary lactase deficiency - a rare condition in which is born without the enzyme to digest the sugar lactose • diarrhea and a temporary lactase deficiency (Note: Switching babies to soy formula when they have diarrhea is controversial and usually not recommended) • Vegan parents (although completely vegan formulas do not exist) (http://pediatrics.about.com/od/infantformula/a/0508_soy_milk.htm) 11. Should an infant with a diagnosed milk allergy be placed on a soymilk based formula? Why/why not? Not usually recommended for a cow milk protein allergy, since many of these infants can also be allergic to soy proteins and should drink an extensively hyrdrolyzed protein formula instead, such as Nutramigen or Alimentum http://pediatrics.about.com/od/infantformula/a/0508_soy_milk.htm 12. Define galactosemia. People with galactosemia are unable to fully metabolize the simple sugar galactose. 13. Which nutrients are lacking on goat milk? Goat’s milk is deficient in vitamin D, vitamin B12, iron and especially folate. Goat's milk offers 1/5th the amount of Vitamin B12 and 1/10th the folic acid of cow's milk. Infants younger than six months of age need 65 μg/day of folate (the recommended daily allowance increases with age). Goat’s milk contains 6 μg/L of folate (breast milk and cow’s milk contain approx. 45 μg/L-50 μg/L). http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2528716/ 14. When do you use protein hydrolysate? It has special application in sports medicine because its consumption allows amino acids to be absorbed by the body more rapidly than intact proteins, thus maximizing nutrient delivery to muscle tissues. It is also used in the biotechnology industry as a supplement to cell cultures (infant formula). These types of formulas contain protein that's been broken down (hydrolyzed) — partially or extensively — into smaller sizes than are those in cow's milk and soy-based formulas. Protein hydrolysate formulas are meant for babies who don't tolerate cow's milk or soy-based formulas. Extensively hydrolyzed formulas are an option for babies who have a protein allergy. (http://www.mayoclinic.org/healthy-living/infant-and-toddler-health/in-depth/infant-formula/art-20045782) 15. Discuss the two follow-up formulas and their usefulness. Infants up to 12 months are not physiologically able to digest cows’ milk and thus, follow-up formula is specially designed to help older infants (over 6 months of age) meet their nutritional requirements as they increase their dietary diversity. Follow-up formula is a liquid food prepared from cows’ milk, or the milk of other animals and/or constituents of animal and/or plant origin. It contains a unique blend of iron, vitamins and minerals, making it a better choice than cows’ milk for infants older than 6 months. Follow-up formula is complementary to breast-feeding or to a breast-milk substitute when either becomes insufficient to satisfy the nutritional requirements of the infant. (http://www.ifm.net/infant-young-child-nutrition/infant-and-young-child-nutrition-options/follow-upformula/) 16. When would evaporated milk formula be used? If necessary (in emergency situations due to low cost), you can make your own formula temporarily from evaporated milk. Evaporated milk formulas have some of the same risks as whole cow's milk, namely, iron deficiency anemia and allergies. http://www.childrenshealthnetwork.org/CRS/CRS/pa_formula_hhg.htm 17. How do you make evaporated milk formula? Mix 13 ounces of evaporated milk with 19 ounces of boiled water and 2 tablespoons of corn syrup. Caution: Avoid honey until 1 year old. Place this mixture in sterilized bottles and keep the bottles refrigerated until use (up to 48 hours). http://www.childrenshealthnetwork.org/CRS/CRS/pa_formula_hhg.htm 18. Which are the disadvantages of using evaporated milk formula? Poorly digested fat, low concentration of iron and vitamin C, excessive amounts of sodium, protein, and phosphorus. Vitamin A and D supplements are needed unless the evaporated milk is fortified. This product also contains high amounts of corn syrup/sugar due to the removal of 60% of the water. (Handbook of Pediatric Nutrition) 19. Which nutrient supplements are needed by an infant on a diet exclusively consisting of a formula? Commercial infant formulas with iron are manufactured to contain all the nutrients your baby needs. Infants, whether breastfed or formula-fed do not need fluoride supplements during the first 6 months. From 6 months to 3 years, babies require fluoride supplements only if the water supply is deficient in fluoride like those who get their water from a well or other unfluorinated source. (http://kidshealth.org/parent/growth/feeding/formulafeed_concerns.html?tracking=P_RelatedArticle#) 20. Which is the maximum amount of formula to be used in a 24 hours unless otherwise indicated? After the first few days, formula-fed newborns will take from 2 to 3 ounces (60–90 ml) of formula per feeding and on average will eat every three to four hours during the first few weeks. At 6 months babies will consume 6 to 8 ounces (180–240 ml) at each of four or five feedings in twenty-four hours. On average, babies should take in about 2 1⁄2 ounces (75 ml) of formula a day for every pound (453 grams) of body weight. Most babies are satisfied with 3 to 4 ounces (90–120 ml) per feeding during the first month. An increase of 1 ounce (30 ml) per month until a maximum of about 7 to 8 ounces (210–240 ml) is reached. Babies should drink no more than 32 ounces (960 ml) of formula in 24 hours. (http://www.healthychildren.org/English/ages-stages/baby/feeding-nutrition/Pages/Amount-and-Schedule-of-FormulaFeedings.aspx) 21. When should extra water in addition to formula be provided in a 3 months old infant? Formula-fed babies may occasionally need extra water, like during hot weather, if they are constipated, or if they are ill or feverish. You should only give small amounts of water at a time. You don’t want water to replace a feed by making the baby feel satiated. For babies younger than six months, boil water first and allow it to cool. Tap water is fine to use. Ensure the formula preparation methods are correct and the bottles do not have too much powder, which can lead to constipation. It’s best not to give babies bottled mineral water, unless you are in a country with poor water sanitation, or you have no alternative. Bottled waters can contain high levels of minerals, such as sodium and sulphates. Babies only need a tiny amount of salt until they are a year old. http://www.babycentre.co.uk/x562087/does-my-formula-fed-baby-need-extra-water#ixzz3Ca6R27HU 22. At what temperature should formula be fed? Some babies may actually prefer cold or room-temperature bottles to warm, especially if that is how they were served from the beginning. If warm bottles are served, remember that the microwave can create dangerous "hot spots" in bottles, so they should not be used. Instead, you can: • Run the bottle under very warm or hot water for a few minutes. • Put bottles in a pan of hot water. Remove the pan from the heat source before placing the bottle in it. • Use bottle warmers that either sit on your countertop at home or plug into car's lighter. Whichever way bottles are heated, be sure to shake vigorously. Test the temperature of the formula by squirting a drop or two on the inside or your wrist before feeding baby. It should be lukewarm (barely warm) not hot. (http://kidshealth.org/parent/pregnancy_newborn/formulafeed/formulafeed_storing.html#) 23. If an infant frequently vomits after eating, how should the infant be handled during and after the feeding? • Burp the infant when they come off each breast, or after every 1 to 2 ounces during bottle feeds. Giving smaller, more frequent feeds may be better than feeds with larger volume. • Keep the babies head upright. Holding the baby is best, since the position of the baby in an infant seat may actually make spitting up more common. • Don't jiggle, bounce, or actively play with babies right after feedings. • Keep your baby's head above his or her feet while feeding (in other words, don't hold your baby in a dipped-down position when feeding). • Raise the head of the crib or bassinet. Roll up a few small hand towels or receiving blankets (or you can buy special "blocks") to place under (not on top of) the mattress. Don't use a pillow under the baby’s head. Make sure the mattress doesn’t fold in the middle, and that the incline is gentle enough so the baby doesn’t slide down. (http://kidshealth.org/parent/pregnancy_newborn/breastfeed/breastfeed_concerns.html) 24. Why should cow’s milk not be taken if an infant is constipated? In cow's milk, approximately 82% of milk protein is casein and the remaining 18% is serum, or whey protein. Some infant formula is more constipating than others. Casein dominant formula, lactose-free formula, AR (anti regurgitation) and thickened formulas can be more constipating for some babies. Variations can also occur between different brands of the same type of formula. Switching formula (or switching to cow's milk) can lead to changes in stool consistency, resulting in either constipation or loose runny stools. Most often this change is only temporary, until your baby's little tummy gets used to the new formula. (We recommend you rule out other reasons for constipation before switching formula.) (http://www.babycareadvice.com/babycare/general_help/article.php?id=48#279) 25. Which measures should be taken if an infant is constipated? Natural remedies: water, sugar, fruit juice, fiber in fruits and vegetables (if eating complementary foods), probiotics Medications: laxatives Other causes that can be corrected: not enough liquid added to powdered formula, need for a different type of formula, medications such as antibiotics, low fiber in mother/baby’s diet (http://www.babycareadvice.com/babycare/general_help/article.php?id=48#279) 26. What is the treatment for acute diarrhea? In 2003, the CDC put forth recommendations for the management of acute pediatric diarrhea. The report included information on the assessment of dehydration and what steps should be taken to adequately treat it. Treatment of dehydration due to diarrhea includes the following: Minimal or no dehydration Rehydration therapy - Not applicable Replacement of losses Less than 10 kg body weight - 60-120 mL oral rehydration solution for each diarrhea stool or vomiting episode More than 10 kg body weight - 120-140 mL oral rehydration solution for each diarrhea stool or vomiting episode Mild-to-moderate dehydration Rehydration therapy - Oral rehydration solution (50-100 mL/kg over 3-4 h) Replacement of losses Severe dehydration Rehydration therapy - Intravenous lactated Ringer solution or normal saline (20 mL/ Replacement of losses Less than 10 kg body weight - 60-120 mL oral rehydration solution for each diarrhea stool or vomiting episode More than 10 kg body weight - 120-140 mL oral rehydration solution for each diarrhea stool or vomiting episode until perfusion and mental status improve, followed by 100 mL/kg oral rehydration solution over 4 hours or 5% dextrose (half normal saline) intravenously at twice maintenance fluid rates Less than 10 kg body weight - 60-120 mL oral rehydration solution for each diarrhea stool or vomiting episode More than 10 kg body weight - 120-140 mL oral rehydration solution for each diarrhea stool or vomiting episode If unable to drink, administer through nasogastric tube or intravenously administer 5% dextrose (one fourth normal saline) with 20 mEq/L potassium chloride (http://emedicine.medscape.com/article/928598-treatment) 27. What is the treatment for gastroesophageal reflux? Most cases of infant reflux clear up on their own, helped by simple changes in feeding techniques: • Smaller, more frequent feedings • Interrupting feedings to burp the baby • Holding baby upright during and after feedings To test to see if the reflux is caused by an allergy to a protein in cow's milk, your baby's doctor may suggest that you eliminate dairy products or beef from your diet if you're breast-feeding. If you feed your baby formula, sometimes switching types can help. • Medication. Acid-blocking medications are not recommended in cases of uncomplicated infant reflux. A short-term trial of an H-2 blocker such as ranitidine, or perhaps a proton pump inhibitor such as omeprazole (Prilosec) or lansoprazole (Prevacid), may be worth trying for babies who have poor weight gain, refuse to feed, have evidence of esophagitis or who have chronic asthma and reflux. It's important to note that otherwise healthy children taking these medications may face an increased risk of certain intestinal and respiratory infections. In addition, prolonged use of proton pump inhibitors has been linked to problems in iron and calcium absorption in infants. • Surgery. In rare instances, the muscle that relaxes to let food into the stomach (the lower esophageal sphincter) needs to be surgically tightened to prevent acid from flowing back into the esophagus. This fundoplication procedure is usually reserved for the few babies who have reflux severe enough to interfere with breathing or prevent growth. (http://www.mayoclinic.org/diseases-conditions/infant-acid-reflux/basics/treatment/con-20026253)