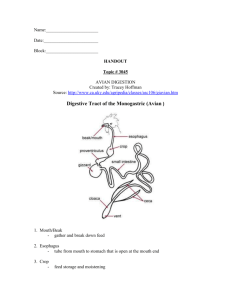
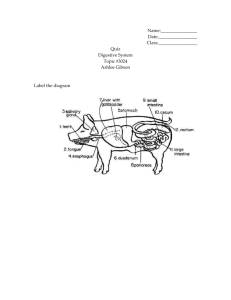
The Digestive System
advertisement

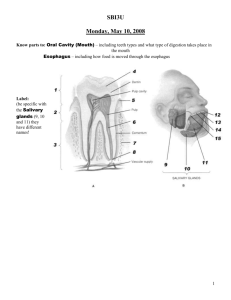
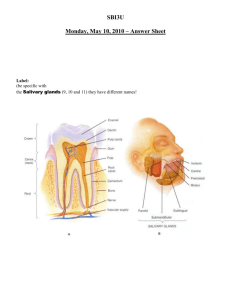
The Digestive System Breakdown • Process and general anatomy • The alimentary canal: From mouth to anus • Physiology of digestion and absorption Digestion • What is digestion and why is it necessary? • How is digestion accomplish? Stages of Digestion • Ingestion • Digestion – Mechanical and chemical • Absorption • Compaction • Defecation http://www.ootonline.com/OOTnews/?p=1507 Digestive System General Anatomy • Structure: common layers through out the system • Mucosa • Submucosa • Muscularis externa • Serosa Variations in Layers of GI Tract • Mucosa (mucous membrane) – lines the lumen and consists of: – inner epithelium • simple columnar in most of digestive tract • stratified squamous from mouth through esophagus, and in lower anal canal – lamina propria – loose connective tissue layer – muscularis mucosa – thin layer of smooth muscle • tenses mucosa creating grooves and ridges that enhance surface area and contact with food • improves efficiency of digestion and nutrient absorption – mucosa-associated lymphatic tissue (MALT) – abundance of lymphocytes and lymphatic nodules • Submucosa – thicker layer of loose connective tissue – contains blood vessels, lymphatic vessels, a nerve plexus, local mucus secreting glands that dump lubricating mucus into the lumen Variations in Layers of GI Tract • Muscularis externa – Two layers of muscle near outer surface – inner circular layer • in some places, thickens to form valves (sphincters) – outer longitudinal layer • responsible for the motility that propels food • Serosa – composed of a thin layer of areolar tissue topped by simple squamous mesothelium – begins in the lower 3 to 4 cm of the esophagus, ends just before rectum – adventitia – a fibrous connective tissue layer that binds and blends the pharynx, most of the esophagus, and the rectum into the adjacent connective tissue of other organs Tissue Layers of GI Tract Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Diaphragm Esophageal hiatus Enteric nervous system: Mucosa: Stratified squamous epithelium Lamina propria Muscularis mucosae Myenteric plexus Submucosal plexus Parasympathetic ganglion of myenteric plexus Submucosa: Esophageal gland Lumen Muscularis externa: Inner circular layer Outer longitudinal layer Blood vessels Serosa Figure 25.2 Enteric Nervous System • Regulates motility, secretion, blood flow • Independent of CNS – CNS greatly influences • Two networks – Submucosal plexus – Myentric plexus Regulation of Digestive Tract • Motility and secretion of the digestive tract are controlled by neural, hormonal, and paracrine mechanisms • Neural control – short (myenteric) reflexes – stretch or chemical stimulation acts through myenteric plexus • stimulates parastaltic contractions of swallowing – long (vagovagal) reflexes - parasympathetic stimulation of digestive motility and secretion • Hormones – chemical messengers secreted into bloodstream – gastrin and secretin • Paracrine secretions – chemical messengers that stimulate nearby target cells Lesser and Greater Omentum Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Liver Gallbladder Stomach Lesser omentum Greater omentum Ascending colon Small intestine Figure 25.3a (a) • lesser omentum- attaches stomach to liver • greater omentum- covers small intestines like an apron Mesentery and Mesocolon Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Greater omentum (retracted) Transverse colon Mesocolon Descending colon Mesentery Jejunum Sigmoid colon Figure 25.3b (b) • mesentery of small intestines holds many blood vessels • mesocolon anchors colon to posterior body wall Mouth Copyright © The McGraw-Hill Companies, Inc. • Oral or buccal cavity • Site of ingestion • Teeth, tongue, saliva Figure 25.4 • Mechanical and chemical digestion The Teeth • Dentition – the teeth • Masticate food into smaller pieces – makes food easier to swallow – exposes more surface area • 32 adult teeth – 20 deciduous (baby) teeth – from midline to the rear of each jaw • • • • 2 incisors – chisel-like cutting teeth used to bite off a piece of food 1 canine – pointed and act to puncture and shred food 2 premolars – broad surface for crushing and grinding 3 molars – even broader surface for crushing and grinding The Teeth • Alveolus – tooth socket in bone – gomphosis joint formed between tooth and bone Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Names of teeth Age at eruption (months) 6–9 Central incisor Lateral incisor 7– 11 16–20 Canine • Periodontal ligament – modified periosteum anchors tooth firmly in alveolus – allows slight movement under pressure of chewing 12–16 1st molar 20–26 2nd molar (a) Deciduous (baby) teeth • Gingiva (gum) – covers the alveolar bone Names of teeth Central incisor Lateral incisor • Regions of a tooth – crown – portion above the gum – root – the portion below the gum, embedded in alveolar bone – neck – the point where crown, root, and gum meet – gingival sulcus – space between the tooth and the gum • hygiene in the sulcus in important to dental health Age at eruption (years) 6–8 7–9 Canine 9–12 1st premolar 10–12 2nd premolar 1st molar 2nd molar 3rd molar (wisdom tooth) (b) Permanent teeth 10–12 6–7 1 –13 17–25 Figure 25.6 Tooth Structure • Dentin – hard yellowish tissue • Enamel – covers crown and neck Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Enamel Crown Dentine • Cementum – covers root Pulp in pulp cavity Gingival sulcus Neck Gingiva Alveolar bone • Root canal in the roots leading to pulp cavity in the crown Periodontal ligament – nerves and blood vessels – apical foramen – pore at the basal end of each root canal Cementum • Occlusion – meeting of the teeth with the mouth closed Root canal Root Apical foramen Artery , nerve, vein Figure 25.7 Saliva • Saliva – – – – – – moisten mouth begin starch and fat digestion cleanse teeth inhibit bacterial growth dissolves molecules so they can stimulate the taste buds moistens food and bind it together into bolus to aid in swallowing • Hypotonic solution of 97.0% to 99.5% water and the following solutes: – – – – – – salivary amylase – begins starch digestion in the mouth lingual lipase – activated by stomach acid and digests fats mucus – binds and lubricates the mass of food and aids in swallowing lysozyme – enzyme that kills bacteria immunoglobulin A (IgA) – an antibody that inhibits bacterial growth electrolytes - Na+, K+, Cl-, phosphate and bicarbonate • pH of 6.8 to 7.0 Salivary Glands • Intrinsic salivary glands – small glands dispersed amid other oral tissues – – – – lingual glands – in the tongue – produce lingual lipase labial glands – inside of the lips buccal glands – inside of the cheek all secrete saliva at a fairly constant rate • Extrinsic salivary glands – three pair connected to oral cavity by ducts – parotid – located beneath the skin anterior to the earlobe – submandibular gland – located halfway along the body of the mandible • its duct empties at the side of the lingual frenulum, near the lower central incisors – sublingual glands – located in the floor of the mouth • has multiple ducts that empty posterior to the papilla of the submandibular duct Pharynx • Pharynx – muscular funnel that connects oral cavity to esophagus – digestive and respiratory tracts intersect • Pharyngeal constrictors (superior, middle, and inferior) circular muscles that force food downward during swallowing – when not swallowing, the inferior constrictor remains contracted to exclude air from the esophagus • Considered upper esophageal sphincter Esophagus • Esophagus – a straight muscular tube 25-30 cm long – begins at level between C6 and the cricoid cartilage – extends from pharynx to cardiac orifice of stomach (T7) – lower esophageal sphincter • prevents stomach contents regurgitation • heartburn – burning sensation produced by acid reflux into the esophagus – nonkeratinized stratified squamous epithelium – esophageal glands in submucosa secrete mucus – skeletal muscle in upper one-third, mixture in middle one-third, and only smooth muscle in the bottom one-third – covered with adventitia sciencequiz.net cytochemistry.net Stomach • Stomach – muscular sac in upper left abdominal cavity immediately inferior to the diaphragm – primarily functions as a food storage organ • internal volume of about 50 mL when empty • 1.0 – 1.5 L after a typical meal • up to 4 L when extremely full and extend nearly as far as the pelvis • Mechanically breaks up food particles, liquefies the food, and begins chemical digestion of protein and fat – chyme – soupy or pasty mixture of semi-digested food in the stomach Gross Anatomy of Stomach Copyright © The McGraw-Hill Companies, Inc. © The McGraw-Hill Companies, Inc./Rebecca Gray, photographer/Don Kincaid, dissections Microscopic Anatomy Copyright © The McGraw-Hill Companies, Inc. • Mucosa – simple columnar epithelium • Gastric pits – depressions in mucosa – Cardiac, pyloric and gastric glands – Produce gastric juice Figure 25.13 b-c Cells of Gastric Glands • Mucous cells – secrete mucus – predominate in cardiac and pyloric glands • Regenerative (stem) cells – found in the base of the pit and in the neck of the gland – divide rapidly and produce a continual supply of new cells Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Mucous neck cell Parietal cell • Parietal cells – found mostly in the upper half of the gland – secrete hydrochloric acid (HCl), intrinsic factor, hunger hormone ghrelin Chief cell • Chief cells – most numerous – secrete gastric lipase and pepsinogen – absent in pyloric and cardiac glands G cell • Enteroendocrine cells – concentrated in lower end of gland – secrete hormones and paracrine messengers that regulate digestion (c) Gastric gland Figure 25.13c Hydrochloric Acid Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Blood Parietal cell Lumen of gastric gland Alkaline tide Cl– Cl– Stomach acid HCO3 – K+ HCO3 – H+ Figure 25.14 H+–K+ ATPase CO2 CO2 + H2O H2CO3 • gastric juice has a high concentration of hydrochloric acid – pH as low as 0.8 • parietal cells produce HCl and contain carbonic anhydrase (CAH) CAH – CO2 + H2O H2CO3 HCO3- + H+ – H+ is pumped into gastric gland lumen by H+- K+ ATPase pump • antiporter uses ATP to pump H+ out and K+ in – HCO3- exchanged for Cl- (chloride shift) from blood plasma • Cl- (chloride ion) pumped into the lumen of gastric gland to join H+ forming HCl • elevated HCO3- (bicarbonate ion) in blood causes alkaline tide increasing blood pH Functions of Hydrochloric Acid • activates pepsin and lingual lipase • breaks up connective tissues and plant cell walls – helps liquefy food to form chyme • converts ingested ferric ions (Fe3+) to ferrous ions (Fe2+) – Fe2+ absorbed and used for hemoglobin synthesis • contributes to nonspecific disease resistance by destroying most ingested pathogens Production and Action of Pepsin Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Parietal cell Removed peptide Dietary proteins HCl Pepsin (active enzyme) Chief cell Pepsinogen (zymogen) Partially digested protein Gastric gland Figure 25.15 Gastric Secretions • Gastric lipase – Combines with lingual lipase – Begin to digest small amount of fats • Intrinsic factor – Secreted by the parietal cells – Required for vitamin B12 absorption – Only essential function of stomach Stomach Rumbles • Digestion and Absorption – Partial digestion of proteins and lipids – Absorption of aspirin and lipid-soluble drugs • Protection – Mucus – Tight junctions – Cell replacement Regulation of Gastric Function • Cephalic phase – Stomach responds to sensory and mental info • Gastric phase – Occurs after ingestion and deglutition – Stimulate gastric activity (secretion) • Ach, Histamine, Gastrin – Act on parietal, chief, enteroendocrine cells – Positive and negative feedback loops • Intestinal phase – Initially stimulates gastric secrestions – Enterogastric reflex- inhibitory signals – Secretion of secretin and cholecystokinin • Suppress gastric secretion and motility Accessory Organs • Liver – Produces and secretes bile • Gall bladder – Stores and concentrates bile – Bile • Contains cholesterol • Bile acids and lecithin help digest fat • 80% of bile acids reabsorbed in ilieum • Pancreas – – – – – Exocrine tissue secretes pancreatic juice Mixture of zymogens, enzymes, NaCO3, and water Zymogens include: trypsinogen, chymotrypsinogen, procarboxypeptidase Enzyms include: lipase, amylase, ribonuclease, deoxyribonuclease Regulation • Ach, CCK, Secretin Small Intestine • Digestion and absorption completed • Duodenum – Pancreatic enzyme digestion • Jejunum – Highly vascularized – Absorption • Ileum – Less vascularized – Absorption – Ileocecal valve Copyright © The McGraw-Hill Companies, Inc. Copyright © The McGraw-Hill Companies, Inc. Intestinal Motility • Segmentation • Peristalsis – Migrating motor complex Copyright © The McGraw-Hill Companies, Inc. Large Intestine • Begins with cecum, 1.5m long • Ascending, transverse, descending, sigmoid • Rectum Copyright © The McGraw-Hill Companies, Inc. • Anus Copyright © The McGraw-Hill Companies, Inc. Carbohydrate Digestion and Absorption • Digestible dietary form is starch • Primary enzyme – amylase – Digests starch into oligosaccharides • Secondary enzymes – dextrinase, glucoamylase, maltase, sucrase, lactase Protein Digestion and Absorption • Three sources – Dietary – Digested enzymes – Sloughed epithelial cells • Digested by proteases – Pepsin (cleaves between tyrosine and phenylalanine) • Stomach – Trypsin, chymotrypsin, carboxypeptidase • Pancreatic secretions – aminopeptidase, dipeptidase • Brush border enzymes • Absorbed like carbohydrates Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Protein Digestion and Absorption Mouth No chemical digestion occurs. Protein N H O C H HO Polypeptides Stomach N H C C H HO O OH N C H O H O N OH H N H H O C Protein Pepsin ( ) hydrolyzes certain peptide bonds, breaking protein down into smaller polypeptides. H HO N H O H C HO Small intestine Actions of pancreatic enzymes O C H N O OH O OH C OH C H H N N H O C C O H N H O C H N C HO N C H OH OH O Trypsin ( ) and chymotrypsin ( ) hydrolyze other peptide bonds, breaking polypeptides down into smaller oligopeptides. OH O OH Oligopeptides H O C H C N C H O H H N N O H H HO Polypeptides OH C H H H C N O N H OH H H N H N N H H OH HO H O C H O H OH H N C O H OH H N O C OH Carboxypeptidase ( ) removes one amino acid at a time from the carboxyl (–COOH) end of an oligopeptide. Small intestine Actions of brush border enzymes (contact digestion) Carboxypeptidase H N H C O OH Aminopeptidase H N H C Dipeptidase O H OH H N O C OH Carboxypeptidase ( ) of the brush border continues to remove amino acids from the carboxyl (–C OOH) end. Aminopeptidase ( ) of the brush border removes one amino acid at a time from the amino (–N H ) end. Blood capillary of intestinal villus Dipeptidase ( ) splits dipeptides into separate amino acids ( ). ( ) Figure 25.29 Lipid Digestion and Absorption • Digested by lipases • Emulsification • Micelles – Transport to brush border • FFAs, monoglycerides, fat-soluable vitamins, cholesterol • Resynthesized – Chylomicrons and exocytosis • Enter lacteals Emulsification Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Emulsification Hydrophilic region Hydrophobic region Lecithin Bile acid Fat globule is broken up and coated by lecithin and bile acids. Fat globule Emulsification droplets Figure 25.30 Fat Hydrolysis and Micelles Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Fat hydrolysis Pancreatic lipase Pancreatic lipase Free fatty acid Lecithin Monoglyceride Bile acid Dietary lipid Triglyceride Emulsification droplets are acted upon by pancreatic lipase, which hydrolyzes the first and third fatty acids from triglycerides, usually leaving the middle fatty acid. Free fatty acid Lipid uptake by micelles Bile acid Monoglycerides Cholesterol Fatty acids Fat-soluble vitamins Figure 25.30 Micelles in the bile pass to the small intestine and pick up several types of dietary and semidigested lipids. Lipid core Micelles Nucleic Acids and Vitamins • Nucleic acid – nucleases (deoxyribonuclease and ribonuclease) hydrolyze DNA and RNA to nucleotides – nucleosidases and phosphatases of brush border split them into phosphate ions, ribose or deoxyribose sugar, and nitrogenous bases • Vitamins – are absorbed unchanged – fat-soluble vitamins - A, D, E and K absorbed with other lipids • if they are ingested without fat-containing food, they are not absorbed at all, but are passed in the feces and wasted – water-soluble vitamins, B complex and C, absorbed by simple diffusion and B12 if bound to intrinsic factor from the stomach Minerals • minerals (electrolytes) – are absorbed all along small intestine – Na+ cotransported with sugars and amino acids – Cl- exchanged for bicarbonate reversing chloride-bicarbonate exchange that occurs in the stomach – iron and calcium absorbed as needed • iron absorption is stimulated by liver hormone hepcidin • absorptive cells bind ferrous ions (Fe2+) and internalize by active transport • unable to absorb ferric ions (Fe3+) but stomach acid reduces ferric ions to absorbable ferrous ions • transferrin (extracellular protein) transports iron in blood to bone marrow, muscle, and liver Water Balance • Digestive system is one of several systems involved in water balance • Digestive tract receives about 9 L of water/day – 0.7 L in food, 1.6 L in drink, 6.7 L in gastrointestinal secretions – 8 L is absorbed by small intestine and 0.8 L by large intestine – 0.2 L voided in daily fecal output • Water is absorbed by osmosis following the absorption of salts and organic nutrients • Diarrhea - occurs when large intestine absorbs too little water – feces pass through too quickly if intestine is irritated – feces contains high concentrations of a solute (lactose) • Constipation – occurs when fecal movement is slow, too much water gets reabsorbed, and feces becomes hardened