The Digestive System
advertisement

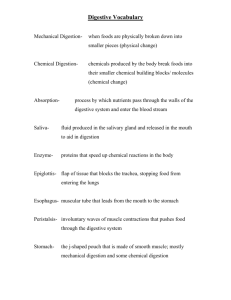
Chapter 24 THE DIGESTIVE SYSTEM I. INTRODUCTION A. Food contains substances and energy the body needs to construct all cell components. The food must be broken down through digestion to molecular size before it can be absorbed by the digestive system and used by the cells. B. The organs that collectively perform these functions compose the digestive system. C. The medical professions that study the structures, functions, and disorders of the digestive tract are gastroenterology for the upper end of the system and proctology for the lower end. II. OVERVIEW OF THE DIGESTIVE SYSTEM A. Organization 1. The two major sections of the digestive system perform the processes required to prepare food for use in the body. 2. The gastrointestinal tract is the tube open at both ends for the transit of food during processing. The functional segments of the GI tract include the mouth, esophagus, stomach, small intestine, and large intestine. 3. The accessory structures that contribute to the food processing include the teeth, tongue, salivary glands, liver, gallbladder, and pancreas. B. Digestion includes six basic processes. 1. Ingestion is taking food into the mouth (eating). 2. Secretion is the release, by cells within the walls of the GI tract and accessory organs, of water, acid, buffers, and enzymes into the lumen of the tract. 3. Mixing and propulsion result from the alternating contraction and relaxation of the smooth muscles within the walls of the GI tract. 1 Digestive System Regulation • Nervous regulation – Involves enteric nervous system • Types of neurons: sensory, motor, interneurons – Coordinates peristalsis and regulates local reflexes • Chemical regulation – Production of hormones • Gastrin, secretin – Production of paracrine chemicals • Histamine • Help local reflexes in ENS control digestive environments as pH levels 4. Digestion a. Mechanical digestion consists of movements of the GI tract that aid chemical digestion. b. Chemical digestion is a series of catabolic (hydrolysis) reactions that break down large carbohydrate, lipid, and protein food molecules into smaller molecules that are usable by body cells. 5. Absorption is the passage of end products of digestion from the GI tract into blood or lymph for distribution to cells. 6. Defecation is emptying of the rectum, eliminating indigestible substances from the GI tract. 2 III. LAYERS OF THE GI TRACT A. The basic arrangement of layers in the gastrointestinal tract from the inside outward includes the mucosa, submucosa, muscularis, and serosa (visceral peritoneum). B. The mucosa consists of an epithelium, lamina propria, and muscularis mucosa. 1. The epithelium consists of a protective layer of non-keratinized stratified cells, simple cells for secretion and absorption, and mucus secreting cells, as well as some enteroendocrine cells that put out hormones that help regulate the digestive process. 2. The lamina propria consists of three components, including loose connective tissue that adheres the epithelium to the lower layers, the system of blood and lymph vessels through which absorbed food is transported, and nerves and sensors. a. The lymph system is part of the mucosa-associated lymph tissues (MALT) that monitor and produce an immune response to pathogens passing with food through the GI tract. b. It is estimated that there are as many immune cells associated with the GI tract as in all the rest of the body. 3. The muscularis mucosa causes local folding of the mucosal layer to increase surface are for digestion and absorption. C. The submucosa consists of aerolar connective tissue. It is highly vascular, contains a part of the submucosal plexus (plexus of Meissner), and contains glands and lymphatic tissue. 1. The submucosal plexus is a part of the autonomic nervous system. 2. It regulates movements of the mucosa, vasoconstriction of blood vessels, and innervates secretory cells of mucosal glands. 3 D. Muscularis 1. The muscularis of the mouth, pharynx, and superior part of the esophagus contains skeletal muscle that produces voluntary swallowing. Skeletal muscle also forms the external anal sphincter. 2. Through the rest of the tract, the muscularis consists of smooth muscle in an inner sheet of circular fibers and an outer sheet of longitudinal fibers. 3. The muscularis also contains the major nerve supply to the GI tract - the myenteric plexus (plexus of Auerbach), which consists of fibers from both divisions of the ANS. This plexus mostly controls GI tract motility. E. The serosa is the superficial layer of those portions of the GI tract that are suspended in the abdominoplevic cavity. 1. The esophagus is covered by an adventitia. 2. Inferior to the diaphragm, the serosa is also called the visceral peritoneum. IV. PERITONEUM A. The peritoneum is the largest serous membrane of the body. 1. The parietal peritoneum lines the wall of the abdominal cavity. 2. The visceral peritoneum covers some of the organs and constitutes their serosa. 3. The potential space between the parietal and visceral portions of the peritoneum is called the peritoneal cavity and contains serous fluid. 4. Some organs, such as the kidneys and pancreas, lie on the posterior abdominal wall behind the peritoneum and are called retroperitoneal. 5. The peritoneum contains large folds that weave between the viscera, functioning to support organs and to contain blood vessels, lymphatic vessels, and nerves of the abdominal organs. 6. Extensions of the peritoneum include the mesentery, meoscolon, falciform ligament, lesser omentum, and greater omentum. 4 B. Peritonitis is an acute inflammation of the peritoneum. V. MOUTH A. Introduction 1. The mouth (oral or buccal cavity) is formed by the cheeks, hard and soft palate, lips, and tongue. 2. The vestibule of the oral cavity is bounded externally by the cheeks and lips and internally by the gums and teeth. 3. The oral cavity proper is a space that extends from the gums and teeth to the fauces, the opening between the oral cavity and the pharynx or throat. B. Salivary Glands 1. The major portion of saliva is secreted by the salivary glands, which lie outside the mouth and pour their contents into ducts that empty into the oral cavity; the remainder of saliva comes from buccal glands in the mucous membrane that lines the mouth. 2. There are three pairs of salivary glands: parotid, submandibular (submaxillary), and sublingual glands. 3. Saliva lubricates and dissolves food and starts the chemical digestion of carbohydrates. It also functions to keep the mucous membranes of the mouth and throat moist. 4. Chemically, saliva is 99.5% water and 0.5% solutes such as salts, dissolved gases, various organic substances, and enzymes. 5. Salivation is entirely under nervous control. 6. Mumps is an inflammation and enlargement of the parotid salivary glands caused by infection with the mumps virus (myxovirus). Symptoms include fever, malaise, pain, and swelling of one or both glands. If mumps is contracted by a male past puberty, it is possible to experience inflammation of the testes and, occasionally, sterility. 5 Saliva and the Salivary Glands • Saliva • Saliva moistens the mouth, digests a small amount of starch and fat, cleanses the teeth, inhibits bacterial growth, dissolves molecules so they can stimulate taste buds, and moistens food and binds particles together to aid in swallowing. It is secreted by the salivary glands. • Saliva is a hypotonic solution composed of 97% to 99.5% water and the following solutes: salivary amylase, lingual lipase, mucus, lysozyme, immunoglobulin A, and electrolytes. • Saliva has a pH of 6.8 to 7.0. Salivation • The extrinsic salivary glands secrete 1.0 to 1.5 L of saliva per day. • Food stimulates tactile, pressure, and taste receptors, which transmit signals to the salivatory nuclei in the medulla oblongata and pons. These nuclei also receive input from higher brain centers so even the odor, sight, or thought of food stimulates salivation. • The salivatory nuclei send autonomic signals: Sympathetic stimulation reduces saliva output, and parasympathetic stimulation causes the production of thinner saliva with more salivary amylase. • Salivary amylase begins to digest starch as the food is chewed, while the mucus of saliva binds food particles into a soft, slippery, easily swallowed mass called a bolus. C. Teeth 1. The teeth project into the mouth and are adapted for mechanical digestion. 2. A typical tooth consists of three principal portions: crown, root, and neck. 3. Teeth are composed primarily of dentin, a calcified connective tissue that gives the tooth its basic shape and rigidity; the dentin of the crown is covered by enamel, the hardest substance in the body, which protects the tooth from the wear of chewing. 6 a. The dentin of the root is covered by cementum, another bone-like substance, which attaches the root to the periodontal ligament (the fibrous connective tissue lining of the tooth sockets in the mandible and maxillae). b. The dentin encloses the pulp cavity in the crown and the root canals in the root. c. The branch of dentistry that is concerned with the prevention, diagnosis, and treatment of diseases that affect the pulp, root, periodontal ligament, and alveolar bone is known as endodontics. Orthodontics is a dental branch concerned with the prevention and correction of abnormally aligned teeth. Periodontics is a dental branch concerned with the treatment of abnormal conditions of tissues immediately around the teeth. 4. There are two dentitions, or sets of teeth, in an individual’s lifetime: deciduous (primary), milk teeth, or baby teeth; and permanent (secondary) teeth. 5. There are four different types of teeth based on shape: incisors (used to cut food), cuspids or canines (used to tear or shred food), premolars or bicuspids (absent in the deciduous dentition and used for crushing and grinding food), and molars (also used for crushing and grinding food). E. Mechanical and Chemical Digestion in the Mouth 1. Through mastication (chewing), food is mixed with saliva and shaped into a bolus that is easily swallowed. 2. The enzyme salivary amylase converts polysaccharides (starches) to disaccharides (maltose). This is the only chemical digestion that occurs in the mouth. VI. PHARYNX A. The pharynx is a funnel-shaped tube that extends from the internal nares to the esophagus posteriorly and the larynx anteriorly. 1. It is composed of skeletal muscle and lined by mucous membrane. 7 2. The nasopharynx functions in respiration only, whereas the oropharynx and laryngopharynx have digestive as well as respiratory functions. B. Deglutition, or swallowing, moves a bolus from the mouth to the stomach. It is facilitated by saliva and mucus and involves the mouth, pharynx, and esophagus. 1. Deglutition consists of a voluntary state, pharyngeal stage (involuntary), and esophageal stage (involuntary). 2. Receptors in the oropharynx stimulate the deglutition center in the medulla and the lower pons of the brain stem. VII. ESOPHAGUS A. The esophagus is a collapsible, muscular tube that lies behind the trachea and connects the pharynx to the stomach. B. The wall of the esophagus contains mucosa, submucosa, and muscularis layers. The outer layer is called the adventitia rather than the serosa due to structural differences. C. Physiology of the Esophagus 1. The esophagus contains an upper and a lower esophageal sphincter. 2. During the esophageal stage of swallowing progressive contractions of the muscularis push the bolus onward. There propulsive contractions are termed peristalsis. D. Gastroesophageal reflux disease occurs when the lower esophageal sphincter fails to close adequately after food has entered the stomach, resulting in stomach contents refluxing into the inferior portion of the esophagus. HCl from the stomach contents irritates the esophageal wall resulting in heartburn. VIII. STOMACH A. Introduction 1. The stomach is a J-shaped enlargement of the GI tract that begins at the bottom of the esophagus and ends at the pyloric sphincter. 8 2. It serves as a mixing and holding area for food, begins the digestion of proteins, and continues the digestion of triglycerides, converting a bolus to a liquid called chyme. It can also absorb some substances. B. Anatomy of the Stomach 1. The gross anatomical subdivisions of the stomach include the cardia, fundus, body, and pyloris. 2. When the stomach is empty, the mucosa lies in folds called rugae. 3. Pylorospasm and pyloric stenosis are two abnormalities of the pyloric sphincter that can occur in newborns. Both functionally block or partially block the exit of food from the stomach into the duodenum and must be treated with drugs or surgery. C. Histology of the Stomach 1. The surface of the mucosa is a layer of simple columnar epithelial cells called mucous surface cells. a. Epithelial cells extend down into the lamina propria forming gastric pits and gastric glands. b. The gastric glands consist of three types of exocrine glands: mucous neck cells (secrete mucus), chief or zymogenic cells (secrete pepsinogen and gastric lipase), and parietal or oxyntic cells (secrete HCl). c. Gastric glands also contain enteroendocrine cells which are hormone producing cells. G cells secrete the hormone gastrin into the bloodstream. 2. The submucosa is composed of areolar connective tissue. 3. The muscularis has three layers of smooth muscle: longitudinal, circular, and an inner oblique layer. 4. The serosa is a part of the visceral peritoneum. a. At the lesser curvature, the visceral peritoneum becomes the lesser omentum. 9 b. At the greater curvature, the visceral peritoneum becomes the greater omentum. 5. Endoscopy refers to visual inspection of any cavity of the body using an endoscope, an illuminated tube with lenses. Endoscopic examination of the stomach is called gastroscopy. In addition to diagnostic use for ulcers and other stomach disorders, it may be employed to halt bleeding, biopsy tumors, and remove foreign objects. D. Mechanical and Chemical Digestion in the Stomach 1. Mechanical digestion consists of peristaltic movements called mixing waves. 2. Chemical Digestion a. Chemical digestion consists mostly of the conversion of proteins into peptides by pepsin, an enzyme that is most effective in the very acidic environment (pH 2) of the stomach. The acid (HCl) is secreted by the stomach’s parietal cells. b. Gastric lipase splits certain molecules in butterfat of milk into fatty acids and monoglycerides and has a limited role in the adult stomach. 3. The stomach wall is impermeable to most substances; however, some water, electrolytes, certain drugs (especially aspirin), and alcohol can be absorbed through the stomach lining. Gastric Secretions • The gastric glands produce 2–3 L of gastric juice daily, composed mainly of water, hydrochloric acid, and pepsin. • Hydrochloric Acid • Gastric juice has a high concentration of hydrochloric acid (HCl) and a pH as low as 0.8. • HCl secretion does not affect the pH of the parietal cells that manufacture it because H+ is pumped out as fast as it is generated. The bicarbonate ions are exchanged for chloride ions from the blood plasma, and the Cl- is pumped into the lumen of the gastric gland. HCl accumulates in the stomach while bicarbonate ions accumulate in the blood. 10 Stomach acid has several functions: • It activates the enzymes pepsin and lingual lipase. • It breaks up connective tissues and plant cell walls. • It converts ferric ions to ferrous ions. • It contributes to nonspecific disease resistance by destroying ingested bacteria and other pathogens. Intrinsic Factor • Parietal cells also secrete a glycoprotein called intrinsic factor that is essential to the absorption of vitamin B12 by the small intestine. • The secretion of intrinsic factor is the only indispensable function of the stomach. Pepsin • Several enzymes are secreted as inactive proteins called zymogens. Chief cells secrete the zymogen called pepsinogen. • Hydrochloric acid removes some of the amino acids from pepsinogen and converts it to pepsin. The function of pepsin is to digest dietary proteins to shorter peptide chains. Other Enzymes • a. In infants, the chief cells also secrete gastric lipase and rennin. Protection of the Stomach • The living stomach is protected in three ways from the harsh chemical of its interior. • It has a highly alkaline mucous coat. • Epithelial cells are replaced every 3–6 days. • Tight junctions between epithelial cells prevent gastric juice from seeping between cells and digesting connective tissue. 11 E. Regulation of Gastric Secretion and Motility 1. Gastric secretion is regulated by nervous and hormonal mechanisms. Stimulation occurs in three overlapping phases: cephalic (reflex), gastric, and intestinal. 2. Cephalic Phase a. The cephalic phase consists of reflexes initiated by sensory receptors in the head. b. The cephalic phase stimulates gastric secretion and motility. 3. Gastric Phase a. The gastric phase begins when food enters the stomach. b. When the stomach walls are distended or when pH increases because proteins have entered the stomach and buffered some of the stomach acid, the stretch receptors and chemoreceptors are activated resulting in waves of peristalsis and continual flow of gastric juice. c. Hormonal negative feedback also regulates gastric secretions during the gastric phase. 1) Chemoreceptors and stretch receptors stimulate the ANS to release acetylcholine which stimulates the release of gastrin by G cells. 2) Gastrin stimulates growth of the gastric glands and secretion of large amounts of gastric juice. It also strengthens contraction of the lower esophageal sphincter, increases motility of the stomach, and relaxes the pyloric and ileocecal sphincters. 3) Acetylcholine released by parasympathetic fibers and gastrin secreted by G cells stimulate parietal cells to secrete more HCl when histamine is present. In other words, histamine enhances the effects of acetylcholine and gastrin. 4. Intestinal Phase a. The intestinal phase is due to activation of receptors in the small intestine. 12 b. When partially digested food enters the small intestine, it triggers the enterogastric reflex and the secretion of gastric inhibitory peptide (GIP), secretin, and cholecystokinin (CCK) by the intestinal mucosa. The effect is inhibition of gastric secretion. 5. Regulation of Gastric Emptying a. Gastric emptying is the periodic release of chyme from the stomach into the duodenum. b. Gastric emptying is stimulated by two factors: nerve impulses in response to distention of the stomach and stomach gastrin in response to the presence of certain types of foods. c. Most food leaves the stomach 2-6 hours after ingestion. Carbohydrates leave earliest, followed by proteins and then fats. d. Gastric emptying is inhibited by the enterogastric reflex and by the hormones CCK and GIP. e. Vomiting is the forcible expulsion of the contents of the upper GI tract (stomach and sometimes duodenum) through the mouth. Prolonged vomiting, especially in infants and elderly people, can be serious because the loss of gastric juice and fluids can lead to disturbances in fluid and acid-base balance. (Clinical Application) IX. PANCREAS A. The pancreas is divided into a head, body, and tail and is connected to the duodenum via the pancreatic duct (duct of Wirsung) and accessory duct (duct of Santorini). B. Pancreatic islets (islets of Langerhans) secrete hormones and acini secrete a mixture of fluid and digestive enzymes called pancreatic juice. C. Pancreatic Juice 13 1. Pancreatic juice contains enzymes that digest starch (pancreatic amylase), proteins (trypsin, chymotrypsin, and carboxypeptidase), fats (pancreatic lipase), and nucleic acids (ribonuclease and deoxyribonuclease). 2. It also contains sodium bicarbonate which converts the acid stomach contents to a slightly alkaline pH (7.1-8.2), halting stomach pepsin activity and promoting activity of pancreatic enzymes. 3. Inflammation of the pancreas is called pancreatitis and can result in trypsin beginning to digest pancreatic cells. D. Pancreatic secretion is regulated by nervous and hormonal mechanisms. The Pancreas • The pancreas is a soft, spongy gland posterior to the greater curvature of the stomach and outside the peritoneal cavity. It has both endocrine and exocrine functions. • Its endocrine part is the pancreatic islets, which secrete insulin and glucagon. • Most of the pancreas is exocrine tissue that secretes 1,200–1,500 mL of pancreatic juice per day. This secretion ends up in the main pancreatic duct running lengthwise through the gland. It empties into the small intestine through the hepatopancreatic ampulla or by way of a smaller accessory pancreatic duct in some people. • Pancreatic juice is an alkaline mixture of water, enzymes, zymogens, sodium bicarbonate, and other electrolytes. • The acinar cells secrete the enzymes and zymogens, whereas the gland ducts secrete the sodium bicarbonate. Bicarbonate buffers the hydrochloric acid from the stomach. • Pancreatic zymogens are trypsinogen, chymotrypsinogen, and procarboxypeptidase. Other pancreatic enzymes include pancreatic amylase, pancreatic lipase, ribonuclease, and deoxyribonuclease • 14 X. LIVER AND GALLBLADDER A. The liver is the heaviest gland in the body and the second largest organ in the body after the skin. B. Anatomy of the Liver and Gallbladder 1. The liver is divisible into left and right lobes, separated by the falciform ligament. Associated with the right lobe are the caudate and quadrate lobes. 2. The gallbladder is a sac located in a depression on the posterior surface of the liver. C. Histology of the Liver and Gallbladder 1. The lobes of the liver are made up of lobules that contain hepatic cells (liver cells or hepatocytes), sinusoids, stellate reticuloendothelial (Kupffer’s) cells, and a central vein. 2. The mucosa of the gallbladder is simple columnar epithelium arranged in rugae. There is no submucosa. The smooth muscle of the muscularis ejects bile into the cystic duct. The outer layer is the visceral peritoneum. Functions of the gallbladder are to store and concentrate bile until it is needed in the small intestine. D. The liver receives a double supply of blood from the hepatic artery and the hepatic portal vein. All blood eventually leaves the liver via the hepatic vein, E. Hepatic cells (hepatocytes) produce bile that is transported by a duct system to the gallbladder for concentration and temporary storage. 1. Bile is partially an excretory product (containing components of worn-out red blood cells) and partially a digestive secretion. 2. Bile’s contribution to digestion is the emulsification of triglycerides. F. The rate of bile secretion is regulated by nervous and hormonal mechanisms as well as by volume of hepatic blood flow and the concentration of bile salts in the blood . G. The liver also functions in carbohydrate, lipid, and protein metabolism; removal of drugs and hormones from the blood; excretion of bilirubin; synthesis of bile salts; storage of vitamins and minerals; phagocytosis; and activation of vitamin D. 15 H. The fusion of individual crystals of cholesterol is the beginning of 95% of all gallstones. Gallstones can cause obstruction to the outflow of bile in any portion of the duct system. Treatment of gallstones consists of using gallstone-dissolving drugs, lithotripsy, or surgery. Functions of the Liver • • • • Carbohydrate metabolism. • glycogenesis • glycogenolysis • Gluconeogenesis Lipid metabolism. • Stores some triglycerides. • Synthesizes lipoproteins. Protein Metabolism. • Deaminates amino acids – ammonia – urea. • Alpha protein synthesis. • Beta protein synthesis. • Albumin synthesis. • Prothrombin synthesis. • Fibrinogen synthesis. Processing of drugs and hormones. • Alcohol. • Penicillin. • Erythromicin. • Sulfanamides. • Thyroid Hormones. • Steroid Hormones. 16 • Phenobarbitol. • Breakdown of old erythrocytes. • Synthesis of bile salts. • • Emulsification of lipids. • Absorption of lipids. Storage of vitamins (A, B12, D, E, K) and minerals (iron and copper). The Gallbladder and Bile • The gallbladder is a sac about 10 cm long. • When bile is not needed for digestion, the hepatopancreatic sphincter is closed. Bile then fills up the bile duct and spills over into the gallbladder, which absorbs water and stores the bile for later use. • The liver produces 500–1,000 mL of bile per day. It is a yellow-green fluid containing minerals, bile pigments, bile salts, cholesterol, neutral fats, and phospholipids. • The principal bile pigment is bilirubin, derived from the decomposition of hemoglobin. • Bile acids are steroids synthesized from cholesterol. Bile acids are phospholipids that aid in fat digestion and absorption. They are not excreted in the feces but are reabsorbed in the ileum and returned to the liver. XII. SUMMARY OF DIGESTIVE HORMONES A. The effects of the four major digestive hormones - gastrin, secretin, CCK, and GIP - are to regulate gastric secretion and motility, as well as secretion of the pancreas, liver, and gallbladder. 1. Gastrin promotes secretion of gastric juice and increases gastric motility. 2. Secretin promotes secretion of bicarbonate ions into pancreatic juice and bile. It inhibits secretion of gastric juice and promotes normal growth and maintenance of the pancreas. It enhances the effects of CCK. Overall, it causes buffering of acid in chyme. 17 3. CCK stimulates secretion of pancreatic juice rich in digestive enzymes and ejection of bile into the duodenum . It also slows gastric emptying. B. There are other hormones secreted by and having effects on the GI tract. They include motilin, substance P, bombesin, vasoactive intestinal polypeptide, gastrin-releasing peptide, and somatostatin. XIII. SMALL INTESTINE A. Introduction 1. The major events of digestion and absorption occur in the small intestine. 2. The small intestine extends from the pyloric sphincter to the ileocecal sphincter. B. Anatomy of the Small Intestine 1. The small intestine is divided into the duodenum, jejunum, and ileum (Figure 24.21). 2. Projections called circular folds, or plicae circularies, are permanent ridges in the mucosa that enhance absorption by increasing surface area and causing chyme to spiral as it passes through the small intestine. The Small Intestine • Nearly all chemical digestion and nutrient absorption occur in the small intestine. The term "small" applies to its diameter, not its length. Circular folds, villi, and microvilli all serve to increase the surface area inside the small intestine. • Gross Anatomy • The small intestine is divided into three regions. • The duodenum constitutes the first 25 cm. It receives the stomach contents, pancreatic juice, and bile. Stomach acid is neutralized here, pepsin is inactivated by the elevated pH, and pancreatic enzymes take over the job of chemical digestion. • The jejunum comprises the next 2.5 m. 18 • The ileum forms the last 3.6 m and ends at the ileocecal junction. C. Histology of the Small Intestine 1. The mucosa forms fingerlike villi which increase the surface area of the epithelium available for absorption and digestion. a. Embedded in the villus is a lacteal (lymphatic capillary) for fat absorption. b. The cells of the mucosal epithelium include absorptive cells, goblet cells, enteroendocrine cells, and Paneth cells. c. The free surface of the absorptive cells feature microvilli, which increase the surface area . They form the brush border which also contains several enzymes. d. The mucosa contains many cavities lined by glandular epithelium. These cavities form the intestinal glands (crypts of Lieberkuhn). 2. The submucosa of the duodenum contains duodenal (Brunner’s) glands which secrete an alkaline mucus that helps neutralize gastric acid in chyme. The submucosa of the ileum contains aggregated lymphatic nodules (Peyer’s patches). Microscopic Anatomy • The largest folds of the intestinal wall are transverse to spiral ridges called circular folds. They occur from the duodenum to the middle of the ileum, where they cause the chyme to flow in a spiral path along the intestine. This slows its progress, allows more contact with the mucosa, and promotes more thorough mixing and nutrient absorption. • The mucosa also possesses villi, which have fingerlike shapes. The largest villi are in the duodenum, and they become progressively smaller in more distal regions of the small intestine. • A villus is covered with two kinds of epithelial cells— columnar absorptive cells and mucussecreting goblet cells. • The core of the villus is filled with areolar tissue containing a capillary network, an arteriole, a venule, and a lymphatic capillary called a lacteal. 19 • Each epithelial cell of a villus has a border of microvilli containing brush border enzymes that carry out contact digestion. Intestinal Secretion • The intestinal crypts secrete 1–2 L of intestinal juice per day, especially in response to acid, hypertonic chyme, and intestinal distension. Intestinal Motility • Contractions of the small intestine serve three functions: (1) to mix chyme with intestinal juice, bile, and pancreatic juice; (2) to churn chyme and bring it in contact with the mucosa for digestion and absorption; and (3) to move residue toward the large intestine. • Segmentation is the most common type of movement of the small intestine. Ringlike constrictions appear at several places along the intestine and then relax while constrictions occur elsewhere. The effect is to churn the contents of the intestine. D. Intestinal Juice and Brush Border Enzymes 1. Intestinal juice provides a vehicle for absorption of substances from chyme as they come in contact with the villi. 2. Some intestinal enzymes (brush border enzymes) break down foods inside epithelial cells of the mucosa on the surfaces of their microvilli. 3. Some digestion also occurs in the lumen of the small intestine. E. Mechanical Digestion in the Small Intestine 1. Segmentation, the major movement of the small intestine, is a localized contraction in areas containing food. 2. Peristalsis propels the chyme onward through the intestinal tract. F. Chemical Digestion in the Small Intestine 1. Carbohydrates are broken down into monosaccharides for absorption. 20 a. Intestinal enzymes break down starches into maltose, maltotriose, and alpha-dextrins (pancreatic amylase); alpha-dextrins into glucose (alphadestrinase); maltose to glucose (maltase); sucrose to glucose and fructose (sucrase); and lactose to glucose and galactose (lactase). b. In some individuals, there is a failure of the intestinal mucosal cells to produce the enzyme lactase. This results in lactose intolerance, the inability to digest the sugar lactose found in milk and other dairy products. It may be a temporary or long-lasting condition and is characterized by diarrhea, gas, bloating, and abdominal cramps after ingestion of diary products. 2. Protein digestion starts in the stomach. a. Proteins are converted to peptides by trypsin and chymotrypsin. Also, enzymes break peptide bonds that attach terminal amino acids to carboxyl ends of peptides (carboxypeptidases) and peptide bonds that attach terminal amino acids to amino ends of peptides (aminopeptidases). b. Finally, enzymes split dipeptides to amino acids (dipeptidase). 3. Most lipid digestion, in an adult, occurs in the small intestine. a. Bile salts break the globules of triglycerides (fats) into droplets, a process called emulsification. b. Pancreatic lipase, due to the increase exposed surface area of the droplets, can hydrolyze more triglycerides into fatty acids and monoglycerides. 4. Nucleic acids are broken down into nucleotides for absorption. G. Regulation of Intestinal Secretion and Motility 1. The most important mechanism for regulating small intestinal secretion is the action of local reflexes in response to the presence of chyme. 2. Hormones (vasoactive intestinal polypeptide or VIP) also assume a role. 21 3. Parasympathetic impulses increase motility; sympathetic impulses decrease motility. H. Absorption in the Small Intestine 1. Absorption is the passage of the end products of digestion from the GI tract into blood or lymph and occurs by diffusion, facilitated diffusion, osmosis, and active transport. 2. Absorption of Monosaccharides a. Essentially all carbohydrates are absorbed as monosaccharides. b. They are absorbed into blood capillaries. 3. Absorption of Amino Acids, Dipeptides, and Tripeptides a. Most proteins are absorbed as amino acids by active transport processes. b. They are absorbed into the blood capillaries in the villus. 4. Absorption of Lipids a. Dietary lipids are all absorbed by simple diffusion. b. Long-chain fatty acids and monoglycerides are absorbed as part of micelles, resynthesized to triglycerides, and formed into protein-coated spherical masses called chylomicrons. 1) Chylomicrons are taken up by the lacteal of a villus. 2) From the lacteal they enter the lymphatic system and then pass into the cardiovascular system, finally reaching the liver or adipose tissue. c. The plasma lipids - fatty acids, triglycerides, cholesterol - are insoluble in water and body fluids. 1) In order to be transported in blood and utilized by body cells, the lipids must be combined with protein transporters called lipoproteins to make them soluble. 2) The combination of lipid and protein is referred to as a lipoprotein. 3) 22 5. Absorption of Electrolytes a. Many of the electrolytes absorbed by the small intestine come from gastrointestinal secretions and some are part of digested foods and liquids. b. Active transport mechanisms are primarily used for electrolyte absorption. 6. Absorption of Vitamins a. Fat-soluble vitamins (A, D, E, and K) are included along with ingested dietary lipids in micelles and are absorbed by simple diffusion. b. Water-soluble vitamins (B and C) are absorbed by simple diffusion. 7. Absorption of Water a. Figure 24.25 reviews the fluid input to the GI tract. b. All water absorption in the GI tract occurs by osmosis from the lumen of the intestines through epithelial cells and into blood capillaries. c. The absorption of water depends on the absorption of electrolytes and nutrients to maintain an osmotic balance with the blood. XIV. LARGE INTESTINE A. Anatomy of the Large Intestine 1. The large intestine (colon) extends from the ileocecal sphincter to the anus. 2. Its subdivisions include the cecum, colon, rectum, and anal canal. 3. Hanging inferior to the cecum is the appendix. a. Inflammation of the appendix is called appendicitis. (Clinical Application) b. A ruptured appendix can result in gangrene or peritonitis, which can be lifethreatening conditions. 4. The colon is divided into the ascending, transverse, descending, and sigmoid portions. 23 The Large Intestine • Gross Anatomy • The large intestine begins with the cecum, a blind pouch inferior to the ileocecal valve. Attached to its lower end is the vermiform appendix. • The appendix is densely populated with lymphocytes and is an important source of immune cells. • The ascending colon begins at the ileocecal valve and passes up the right side of the abdominal cavity near the right lobe of the liver, where it becomes the transverse colon. This passes horizontally across the upper abdominal cavity, turns 90o downward, and becomes the descending colon. • At the pelvic inlet, the colon turns medially and downward, forming a roughly S-shaped portion called the sigmoid colon. Within the pelvic cavity, the colon straightens and becomes the rectum. • The rectum has three internal folds called rectal valves that enable it to retain feces while passing gas. • The final 3 cm of large intestine is the anal canal, which passes through the levator ani muscle and terminates at the anus. Here the mucosa forms longitudinal ridges (anal columns) with depressions between them (anal sinuses). • Large hemorrhoidal veins form superficial plexuses in the anal columns and, since they lack valves, are especially subject to distention, leading to hemorrhoids. • The anus is regulated by two sphincters—an internal anal sphincter composed of smooth muscle, and an external anal sphincter composed of skeletal muscle. Histology of the Large Intestine 1. The mucosa of the large intestine has no villi or permanent circular folds. It does have a simple columnar epithelium with numerous globlet cells. 24 2. The muscularis contains specialized portions of the longitudinal muscles called taeniae coli, which contract and gather the colon into a series of pouches called haustra. C. Mechanical movements of the large intestine include haustral churning, peristalsis, and mass peristalsis. D. The last stages of chemical digestion occur in the large intestine through bacterial, rather than enzymatic, action. Substances are further broken down and some vitamins are synthesized by bacterial action and absorbed by the large intestine. Microscopic Anatomy • The mucosa of the large intestine has a simple columnar epithelium in all regions except the anal canal, where it is stratified squamous. • There are no circular folds or villi in the large intestine, but there are intestinal crypts, which are deeper than in the small intestine and have a greater density of goblet cells. Mucus is their only significant secretion. Bacterial Flora and Intestinal Gas • The large intestine is densely populated with several species of bacteria referred to collectively as the bacterial flora. They ferment cellulose and other undigested carbohydrates and synthesize B vitamins and vitamin K, which are absorbed by the colon. • The average person expels about 500 mL of flatus per day. It is composed of nitrogen, carbon dioxide, hydrogen, methane, hydrogen sulfide, and the amines indole and skatole. Absorption and Motility • In the large intestine, food undergoes no further chemical digestion, but its volume is reduced as it passes through. The feces consist of 75% water and 25% solid matter, of which 30% is bacteria and 30% undigested fiber. • The most common type of colonic motility is a type of segmentation called haustral contractions, which occur about every 30 minutes. 25 • Stronger contractions, called mass movements, occur one to three times a day, last about 15 minutes each, and occur especially within an hour after breakfast. E. Absorption and Feces Formation in the Large Intestine 1. The large intestine absorbs water, electrolytes, and some vitamins. 2. Feces consist of water, inorganic salts, sloughed-off epithelial cells, bacteria, products of bacterial decomposition, and undigested parts of food. 3. Although most water absorption occurs in the small intestine, the large intestine absorbs enough to make it an important organ in maintaining the body’s water balance. F. Defecation Reflex 1. The elimination of feces from the rectum is called defecation. 2. Defecation is a reflex action aided by voluntary contractions of the diaphragm and abdominal muscles. The external anal sphincter can be voluntarily controlled (except in infants) to allow or postpone defecation. 3. Diarrhea refers to frequent defecation of liquid feces. It is caused by increased motility of the intestine and can lead to dehydration and electrolyte imbalances. 4. Constipation refers to infrequent or difficult defecation and is caused by decreased motility of the intestines, in which feces remain in the colon for prolonged periods of time. It may be alleviated by increasing one’s intake of dietary fiber and fluids. 5. Dietary fiber may be classified as insoluble (does not dissolve in water) and soluble (dissolves in water). Both types affect the speed of food passage through the GI tract and may produce a number of benefits in the GI tract as well as elsewhere in the body. There is evidence that insoluble fiber may help protect against colon cancer and that soluble fiber may help lower blood cholesterol level. 26 Defecation • In the intrinsic defecation reflex, stretch signals travel by the mesenteric nerve plexus to the muscularis of the descending and sigmoid colons and the rectum. This triggers a peristaltic wave that drives the feces downward, and it relaxes the internal anal sphincter. Defecation occurs only if the external anal sphincter is voluntarily relaxed at the same time. • The intrinsic reflex is relatively weak and usually requires the cooperative action of a stronger parasympathetic defecation reflex involving the spinal cord. This intensifies the peristaltic response and helps relax the internal anal sphincter. Chemical Digestion and Absorption Carbohydrates • Most digestible dietary carbohydrate is starch. • Carbohydrate Digestion • Starch is digested first to oligosaccharides two to eight glucose residues long, then into the disaccharide maltose, and finally to glucose, which is absorbed by the small intestine. • The process of starch digestion begins in the mouth. Salivary amylase hydrolyzes starch into oligosaccharides and functions best at the pH of the mouth cavity. It is denatured quickly upon contact with stomach acid. • Starch digestion resumes in the small intestine when the chyme mixes with pancreatic amylase that entirely converts it to oligosaccharides and maltose within 10 minutes. Its digestion is completed by the brush border enzymes maltase, sucrase, and lactase.. • Carbohydrate Absorption • In the plasma membrane adjacent to the brush border enzymes, there are transport proteins that absorb monosaccharides as soon as they are produced. Most of the absorbed sugar is glucose, which is taken up by a sodium-glucose transport protein (SGLT). 27 • After a high-carbohydrate meal, two to three times as much glucose is absorbed by solvent drag as by SGLT. Lipids • Fats are digested by enzymes called lipases. • Lingual lipase from the intrinsic salivary glands is activated by stomach acid, where it digests as much as 10% of the ingested fat. • Most fat digestion occurs in the small intestine through the action of pancreatic lipase. • In the small intestine, fats are first broken up into smaller emulsification droplets by lecithin and bile acids in the bile. When lipase digests fats, the products are two free fatty acids (FFAs) and a monoglyceride. Bile salts coat these and other lipids and form droplets called micelles. • Micelles pass between the microvilli of the brush border, and upon reaching the surface of the epithelial cell, they release their lipids. The lipids diffuse freely across the phospholipid plasma membrane. • Within the cell, the FFAs and monoglycerides are resynthesized into triglycerides. They are coated with a thin film of protein, forming droplets called chylomicrons. • Although some free fatty acids enter the blood capillaries, chylomicrons are too large to do so and much be first transported in the lymphatic lacteal. Proteins • Enzymes that digest proteins are called proteases or peptidases. They are absent from the saliva but begin their job in the stomach. • In the stomach, pepsin hydrolyzes any peptide bond between tyrosine and phenylalanine, thus digesting 10–15% of the dietary protein into shorter polypeptides. • In the small intestine, the pancreatic enzymes trypsin and chymotrypsin take over protein digestion by hydrolyzing polypeptides into even shorter oligopeptides. Finally 28 these are taken apart one amino acid at a time by carboxypeptidase, aminopeptidase, and dipeptidase. All three of these enzymes are found on the brush border. • Amino acid absorption is similar to that of monosaccharides. There are several sodiumdependent amino acid cotransporters for different classes of amino acids. Nucleic Acids • Nucleic acids are generally present in small quantities compared to the other polymers. The nucleases of pancreatic juice (deoxyribonuclease and ribonuclease) hydrolyze these to their component nucleotides. Nucleosidases and phosphatases of the brush border further break them down, and the products are transported across the intestinal epithelium by membrane carriers. Vitamins • Vitamins are absorbed unchanged. • The fat-soluble vitamins (A, D, E, and K) are absorbed with other lipids. • Water-soluble vitamins are absorbed by simple diffusion, with the exception of vitamin B12, an unusually large molecule that can only be absorbed if it binds to intrinsic factor from the stomach. Minerals • Minerals (electrolytes) are absorbed along the entire length of the small intestine. • Iron and calcium are unusual in that they are absorbed in proportion to the body's need, whereas other minerals are absorbed at fairly constant rates, regardless of need. Water • The digestive system is one of several systems involved in water balance. • The digestive tract receives about 9 L of water per day—0.7 L in food, 1.6 L in drink, 6.7 L in gastrointestinal secretions. About 8 L of this is absorbed by the small intestine and 0.8 L by the large intestine. Water is absorbed by osmosis. 29 • Diarrhea occurs when the large intestine absorbs too little water from the feces. • Constipation occurs when fecal movement is slow, too much water is reabsorbed, and the feces become hardened. XV. DEVELOPMENTAL ANATOMY OF THE DIGESTIVE SYSTEM A. The endoderm of the primitive gut forms the epithelium and glands of most of the gastrointestinal tract. B. The mesoderm of the primitive gut forms the smooth muscle and connective tissue of the GI tract. XVI. AGING AND THE DIGESTIVE TRACT A. General changes associated with aging of the digestive system include decreasing secretory mechanisms, decreasing motility of the digestive organs, loss of strength and tone of digestive muscular tissue and its supporting structures, changes in neurosecretory feedback, and diminished response to pain and internal sensations. B. Specific changes include reduced sensitivity to mouth irritations and sores, loss of taste, periodontal disease, difficulty in swallowing, hiatal hernia, cancer of the esophagus, gastritis, peptic ulcer, gastric cancer, duodenal ulcers, appendicitis, malabsorption, maldigestion, gallbladder problems, cirrhosis, acute pancreatitis, constipation, cancer of the colon or rectum, hemorrhoids, and diverticular disease of the colon. XVII. DISORDERS: HOMEOSTATIC IMBALANCES A. Dental caries, or tooth decay, is started by acid-producing bacteria that reside in dental plaque, act on sugars, and demineralize tooth enamel and dentin with acid. B. Periodontal diseases are characterized by inflammation and degeneration of the gingivae (gums), alveolar bone, periodontal ligament, and cementum. C. Peptic ulcers are crater-like lesions that develop in the mucous membrane of the GI tract in areas exposed to gastric juice. The most common complication of peptic ulcers is bleeding, which can lead to anemia if blood loss is serious. The three well-defined causes of peptic ulcer disease (PUD) are 30 the bacterium Helicobacter pylori; nonsteroidal anti-inflammatory drugs, such as aspirin; and hypersecretion of HCl. D. Diverticula are saclike outpouchings of the wall of the colon in places where the muscularis has become weak. The development of diverticula is called diverticulosis. Inflammation within the diverticula, known as diverticulitis, may cause pain, nausea, vomiting, and either constipation or an increased frequency of defecation. High fiber diets help relieve the symptoms. E. Tumors, both benign and malignant, may occur in any portion of the GI tract. One of the most common and deadly malignancies is colorectal cancer, second only to lung cancer in males and third after lung and breast cancer in females. Screening for colorectal cancer includes fecal occult blood testing, digital rectal examination, sigmoidoscopy, colonoscopy, and barium enema. F. Hepatitis is an inflammation of the liver and can be caused by viruses, drugs, and chemicals, including alcohol. 1. Hepatitis A (infectious hepatitis) is caused by hepatitis A virus and is spread by fecal contamination. It does not cause lasting liver damage. 2. Hepatitis B is caused by hepatitis B virus and is spread primarily by sexual contact and contaminated syringes and transfusion equipment. It can produce cirrhosis and possibly cancer of the liver. Vaccines are available to prevent hepatitis B infection. 3. Hepatitis C is caused by the hepatitis C virus. It is clinically similar to hepatitis B and is often spread by blood transfusions. It can cause cirrhosis and possibly liver cancer. 4. Hepatitis D is caused by hepatitis D virus. It is transmitted like hepatitis B and, in fact, a person must be coinfected with hepatitis B before contracting hepatitis D. It results in severe liver damage and has a high fatality rate. 5. Hepatitis E is caused by hepatitis E virus and is spread like hepatitis A. It is responsible for a very high mortality rate in pregnant women. 31 G. Anorexia nervosa is a chronic disorder characterized by self-induced weight loss, body-image and other perceptual disturbances, and physiologic changes that result from nutritional depletion. The disorder is found predominantly in young, single females and may be inherited. Individuals may become emaciated and may ultimately die of starvation or one of its complications. Treatment consists of psychotherapy and dietary regulation. DIGESTIVE NOTES I. Nutrients Polymers A. Carbohydrates B. Lipids C. Proteins D. Nucleic Acids II. Monomers A. monosaccharides B. monoglycerides and fatty acids C. amino acids D. nucleotides Digestive Functions and Processes A. Four Functions 1. ingestion 2. digestion a. mechanical b. chemical 3. absorption 4. defecation B. Three Principal Processes in Digestive Process 1. Motility - peristalsis, mixing waves, segmentation, mass peristalsis, haustral churning 2. Secretion – enzymes, hormones 3. Membrane Transport (absorption) III. Mouth (pH 6.35 – 7.0) A. Mechanical Digestion – Mastication B. Chemical Digestion 1. Salivary Amylase – breaks starch into maltose and alpha dextrins. 2. Lingual Lipase – breaks fats into monoglycerides and fatty acids. Bolus IV. Pharynx A. Deglutition 1. Buccal Phase 2. Esophageal Phase 32 B. Peristalsis V. Stomach (pH 0.8-1.5) A. Mechanical Digestion – Mixing Waves B. Chemical Digestion 1. Pepsin – (Pepsinogen + HCL) Breaks proteins into polypeptides. 2. Gastric Lipase – Lipids into monoglycerides and fatty acids. 3. Rennin – Curdles milk. C. Phases of Stomach Activity 1. Cephalic. 2. Gastric a. pH b. Stretching c. Chemicals 1. Acetylcholine 2. Histamine. 3. Gastrin. 3. Intestinal a. Secretin. b. Cholicystokinin. c. Gastric inhibiting peptide. VI. Liver A. Carbohydrate Metabolism 1. glycogenesis 2. glycogenolysis 3. gluconeogenesis B. Lipid Metabolism 1. Stores some triglycerides. 2. Forms lipoproteins. C. Protein Mebabolism 1. Deaminates amino acids – ammonia – urea. 2. alpha proteins. 3. beta proteins. 4. albumin. 5. prothrombin. 6. fibrinogen. D. Processing drugs and Hormones 1. alcohol 2. penicillin 3. erythromycin 4. sulfanamides 5. thyroid hormones 6. steroid hormones 33 E. Breakdown of old ethrocytes F. Synthesis of bile salts 1. emulsification of lipids. 2. absorption of lipids. G. Storage 1. Vitamin A, B12, D, E, K. 2. Iron and Copper. H. Phagocytosis VII. Pancreas A. Secretions 1. Alkaline secretions. (pH 7.4-7.8) 2. pancreatic amylase - starch to maltose and alpha dextrins. 3. trypsinogen – trypsin – proteins to polypeptides. 4. chymotrypsinogen – chymotrypsin – proteins to polypeptides. 5. procarboxypeptidase – carboxypeptidase - forms dipeptides 6. pancreatic lipase – triglycerides to monoglycerides and fatty acids. 7. ribonuclease – breaks down RNA into nucleotides. 8. deoxyribonuclease – Breaks down DNA into nucleotides. CCK and Secretin VIII. Small Intestine (pH 7.4 – 7.8) A. Surface area increased by 1. circular folds 2. villi 3. microvilli (brush border) 4. length B. Regions 1. duodenum (25 centimeters) 2. jejunum (2.5 meters) 3. ileum (3.6 meters) C. Mechanical Digestion - segmentation D. Chemical Digestion 1. Carbohydrates a. pancreatic amylase b. dextrinase - breaks down alpha dextrins. c. Maltase – breaks down maltose d. Sucrase – breaks down sucrose e. Lactase – breaks down lactose 2. Lipids a. bile – emulsifies lipids. b. Pancreatic lipase 34 3. Proteins a. trypsin b. chymotrypsin c. carboxypeptidase d. aminopeptidase – forms amino acids e. dipeptidase – forms amino acids f. 4. Nucleic Acids a. ribonuclease b. deoxyribonuclease c. nucleodidase – breaks down nucleotides d. phosphatases – breaks down nucleotides IX. Large Intestine (pH 7.4 – 7.8) A. Mechanical Digestion – haustral churning B. Chemical Digestion – Bacterial C. Defecation 1. diarrhea 2. constipation X. Hormones A. Absorptive Hormones - Insulin – glycogenesis, lipogenesis B. Postabsorptive Hormones 1. 2. 3. 4. glucagons – glycogenolysis, gluconeogenesis, lipolysis cortisol – gluconeogenesis, protein breakdown growth hormone - lipolysis epinephrine – glycogenolysis, lipolysis VII. METABOLIC ADAPTATIONS A. Your metabolic reactions depends on how recently you have eaten. During the absorptive state, which alternates with the postabsorptive state, ingested nutrients enter the blood and lymph from the GI tract, and glucose is readily available for ATP production. 35 1. An average meal requires about 4 hours for complete absorption, and given three meals a day, the body spends about 12 hours of each day in the absorptive state. (The other 12 hours, during late morning, late afternoon, and most of the evening, are spent in the postabsorptive state.) 2. Hormones are the major regulators of reactions during each state. B. Metabolism During the Absorptive State 1. Several things typically happen during the absorptive state. a. Most body cells produce ATP by oxidizing glucose to carbon dioxide and water. b. Glucose transported to the liver is converted to glycogen or triglycerides. Little is oxidized for energy. c. Most dietary lipids are stored in adipose tissue. d. Amino acids in liver cells are converted to carbohydrates, fats, and proteins. 2. Regulation of Metabolism During the Absorptive State a. Soon after eating, gastric inhibitory peptide and the rise in blood glucose concentration stimulate insulin release from pancreatic beta cells. In several ways, insulin stimulates absorptive state metabolism. C. Metabolism During the Postabsorptive State 1. During the postabsorptive state, absorption is complete, and the energy needs of the body must be satisfied by nutrients already present in the body. a. The major concern of the body during the postabsorptive state is to maintain normal blood glucose level (70 to 110 mg/100 ml of blood). b. Homeostasis of blood glucose concentration is especially important for the nervous system and red blood cells. 1) The dominant fuel molecule for ATP production in the nervous system is glucose because fatty acids are unable to pass the blood-brain barrier. 36 2) Red blood cells derive all of their ATP from glycolysis of glucose because they lack mitochondria and thus lack the Krebs cycle and electron transport chain. 2. Postabsorptive State Reactions a. Reactions that produce glucose are the breakdown of liver glycogen, gluconeogenesis using lactic acid, and gluconeogenesis using amino acids. b. Reactions that produce ATP without using glucose are oxidation of fatty acids, oxidation of lactic acid, oxidation of amino acids, oxidation of ketone bodies, and breakdown of muscle glycogen. 3. Regulation of Metabolism During the Postabsorptive State a. The hormones that stimulate metabolism in the postabsorptive state sometimes are called anti-insulin hormones because they counter the insulin effects that dominate the absorptive state. The most important anti-insulin hormone is glucagon. b. A low blood glucose level also activates the sympathetic branch of the ANS. D. Metabolism During Fasting and Starvation 1. Fasting means going without food for many hours or a few days whereas starvation implies weeks or months of food deprivation or inadequate food intake. a. Catabolism of stored triglycerides and structural proteins can provide energy for several weeks. b. The amount of adipose tissue determines the lifespan possible without food. 2. During fasting and starvation, nervous tissue and red blood cells continue to use glucose for ATP production. 3. During prolonged fasting, large amounts of amino acids from tissue protein breakdown (primarily from skeletal muscle) are released to be converted to glucose in the liver by gluconeogenesis. 37 4. The most dramatic metabolic change that occurs with fasting and starvation is the increase in formation of ketone bodies by hepatocytes. a. Ketogenesis increases as catabolism of fatty acids rises. b. The presence of ketones actually reduces the use of glucose for ATP production, which in turn decreases the demand for gluconeogenesis and slows the catabolism of muscle proteins. 5. Alcohol absorption is slower in the stomach than in the small intestine due to the increased surface area for absorption in the small intestine. VIII. HEAT AND ENERGY BALANCE A. A normal body temperature is maintained by a delicate balance between heat-producing and heatlosing mechanisms. B. Metabolic Rate 1. The overall rate at which heat is produced is termed the metabolic rate. a. Measurement of the metabolic rate under basal conditions is called the basal metabolic rate (BMR). b. BMR is a measure of the rate at which the quiet, resting, fasting body breaks down nutrients to liberate energy. c. BMR is also a measure of how much thyroxine the thyroid gland is producing, since thyroxine regulates the rate of ATP use and is not a controllable factor under basal conditions. 3. Heat is a form of kinetic energy that can be measured as temperature and expressed in units called calories. a. A calorie, spelled with a little c, is the amount of heat energy required to raise the temperature of 1 gram of water from 140C to 150C. b. A kilocalorie or Calorie, spelled with a capital C, is equal to 1000 calories. 38 C. Body Temperature Homeostasis 1. If the amount of heat production equals the amount of heat loss, one maintains a constant core temperature near 370C (98.60F). a. Core temperature refers to the body’s temperature in body structures below the skin and subcutaneous tissue. b. Shell temperature refers to the body’s temperature at the surface, that is, the skin and subcutaneous tissue. c. Too high a core temperature kills by denaturing body proteins, while too low a core temperature causes cardiac arrhythmias that can result in death. 2. Heat Production a. The production of body heat is influenced by metabolic rate and responses that occur when body temperature starts to fall. b. Factors that affect metabolic rate include exercise, hormones, the nervous system, body temperature, ingestion of food, age, and other factors such as gender, climate, sleep, and malnutrition. c. Heat conservation mechanisms include vasoconstriction, sympathetic stimulation, skeletal muscle contraction (shivering), and thyroid hormone production. 3. Heat is lost from the body by radiation, evaporation, conduction, and convection. a. Radiation is the transfer of heat from a warmer object to a cooler object without physical contact. b. Evaporation is the conversion of a liquid to a vapor. Water evaporating from the skin takes with it a great deal of heat. The rate of evaporation is inversely related to relative humidity. c. Conduction is the transfer of body heat to a substance or object in contact with the body, such as chairs, clothing, jewelry, air, or water. 39 d. Convection is the transfer of body heat by a liquid or gas between areas of different temperature. 4. Hypothalmic Thermostat a. The hypothalmic thermostat is the preoptic area. b. Nerve impulses from the preoptic area propagate to other parts of the hypothalamus known as the heat-losing center and the heat-promoting center. 5. Several negative feedback loops work to raise body temperature when it drops too low or raises too high. 6. Hypothermia refers to a lowering of body temperature to 350C (950F) or below. It may be caused by an overwhelming cold stress, metabolic disease, drugs, burns, malnutrition, transection of the cervical spinal cord, and lowering of body temperature for surgery. XIV. REGULATION OF FOOD INTAKE A. Two centers in the hypothalamus related to regulation of food intake are the feeding (hunger) center and satiety center. The feeding center is constantly active but may be inhibited by the satiety center. B. Among the stimuli that affect the feeding and satiety centers are glucose, amino acids, lipids, body temperature, distention of the GI tract, and choleocystokinin. X. NUTRITION A. Guidelines for healthy eating include eating a variety of foods; maintaining healthy weight; choosing foods low in fat, saturated fat, and cholesterol; eating plenty of vegetables, fruits, and grain products; using sugar only in moderation; using salt and sodium only in moderation; and drinking alcohol only in moderation or not at all. 1. The Food Guide Pyramid shows how many servings of the five major food groups to eat each day. 40 2. Foods high in complex carbohydrates serve as the base of the pyramid since they should be consumed in largest quantity. B. Minerals are inorganic substances that help regulate body processes. 1. Minerals known to perform essential functions include calcium, phosphorus, sodium, chlorine, potassium, magnesium, iron, sulfur, iodine, manganese, cobalt, copper, zinc, selenium, and chromium. C. Vitamins are organic nutrients that maintain growth and normal metabolism. Many function in enzyme systems as coenzymes. 1. Most vitamins cannot be synthesized by the body. No single food contains all of the required vitamins – one of the best reasons for eating a varied diet. 2. Based on solubility, vitamins fall into two main groups: fat-soluble and water-soluble. a. Fat-soluble vitamins are emulsified into micelles and absorbed along with ingested dietary fats by the small intestine. They are stored in cells (particularly liver cells) and include vitamins A, D, E, and K. b. Water-soluble vitamins are absorbed along with water in the GI tract and dissolve in the body fluids. Excess quantities of these vitamins are excreted in the urine. The body does not store water-soluble vitamins well. They include the B vitamins and vitamin C. c. Vitamins C, E, and beta-carotene (a provitamin) are termed antioxidant vitamins because they inactivate oxygen free radicals. 3. Most physicians do not recommend taking vitamin or mineral supplements except in special circumstances, and instead suggest being sure to eat a balanced diet that includes a variety of food. 41 X. DISORDERS: HOMEOSTATIC IMBALANCES A. Body Temperature Abnormalities 1. Fever is an elevation of body temperature that is due to resetting of the hypothalamic thermostat. The most common cause of fever is a viral or bacterial infection. 2. Heat Cramps, Heat Exhaustion, and Heatstroke a. Heat cramps are painful skeletal muscle contractions which are due to profuse sweating that removes water and salt from the body. b. Heat exhaustion (heat prostration), due to fluid and electrolyte loss, results in a normal or below normal body temperature, profuse perspiration, nausea or vomiting, cramps, and dizziness or fainting. Blood pressure may also decrease as a result. c. Heatstroke (sunstroke) occurs when the temperature and relative humidity are high, making it difficult for the body to lose heat by normal means. It results in decreased blood flow to the skin, reduced perspiration, and sharply rising body temperature. Immediate cooling of the body must occur to prevent permanent brain damage. B. Obesity is defined as a body weight more than 20% above desirable standard as the result of excessive accumulation of fat. 1. Even moderate obesity is hazardous to health. 2. Obesity is implicated as a risk factor in cardiovascular disease, hypertension, pulmonary disease, non-insulin dependent diabetes mellitus (type II), arthritis, certain cancers (breast, uterus, and colon), varicose veins, and gallbladder disease. C. Malnutrition refers to a state of poor nutrition. 1. Causes of malnutrition include undernutrition, which can be caused by fasting, anorexia nervosa, deprivation, cancer, gastrointestinal obstructions, inability to swallow, renal disease, and poor dentition. 42 2. Other causes of malnutrition are imbalance of nutrients, malabsorption of nutrients, improper distribution of nutrients, inability to use nutrients (as in diabetes mellitus), increased nutrient requirements (due to fever, infections, burns, fractures, stress, and exposure to heat or cold), increased nutrient losses (diarrhea, bleeding, glycosuria, and fistula drainage), and overnutrition (excess vitamins, minerals, and calories). 3. Protein-calorie undernutrition may be classified into two types based on which factor is lacking in the diet. a. Kwashiorkor results from a deficient protein intake despite normal or nearly normal calorie intake. b. Marasmus is caused by inadequate intake of both protein and calories. Anaerobic fermentation – The conversion of pyruvic acid to lactic acid. This process does not require oxygen. It is anaerobic. This process produces a net of 2 ATPs. Aerobic respiration – The metabolic pathway which breaks down pyruvic acid to carbon dioxide and water and generates up to 36 ATPs from each glucose molecule. Requires oxygen. Chemiosmosis – The process which occurs at the inner mitochondrial membrane and uses energy captured during glycolysis, the oxidation of pyruvic acid (formation of acetyl CoA), and the Kreb’s cycle to pump hydrogen and create a hydrogen gradient. The flow of hydrogen is then used to generate ATP Glycogenesis – The formation of glycogen from glucose. Glycogenolysis – The breakdown of glycogen to glucose. Gluconeogenesis – The formation of glucose from a noncarbohydrate source such as amino acids and lipids. Lipogenesis – The formation of lipids (fat). Lipolysis – The breakdown of lipids (fat). 43 Beta oxidation – The catabolism of fatty acids involving the removal of two carbon atoms at a time from the fatty acid. Ketone bodies – Breakdown components of fatty acids which accumulate during oxidation of fats. Deamination – The removal of the amino group from an amino acid. Uric Acid – A substance formed during the breakdown of nucleic acids. 44