Echinocandins
advertisement

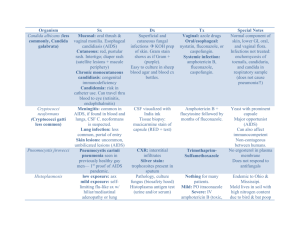
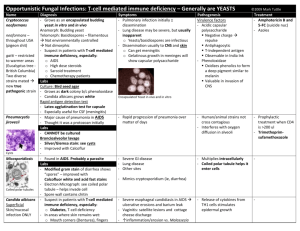
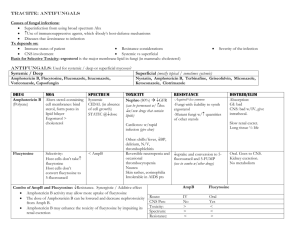
ANTIFUNGALS LauraLe Dyner, MD Pediatric Infectious Disease Fellow October 2008 Fungi Plant-like organisms that lack chlorophyll 1 of the 5 Kingdoms More than 100,000 species 400 known to cause disease in plants, animals, and humans Cell: Chitin cell wall Cell membranes have ergosterol Fungal Cell Structure Yeasts Candida Cryptococcus Rhodotorula Molds Aspergillus Zygomycetes Scedosporidium Cladosporidium Ulocladium Fusarium Paecilomyces Dimorphic Coccidioides Histoplasma Blastomycosis Paracoccidiodes Sporothrix Yeasts Unicellular Although some species form pseudohyphae Smooth in appearance Asexual reproduction (budding/fission) is more common than sexual reproduction Molds Multicellular “Fuzzy” in appearance Hyphae: determines the type of mold Mold spores can survive harsh environments Dimorphic Fungi Capable of growing in mold or yeast form Differs based on environmental condition Temperature CO2 Nutrients Coccidiomycosis: Fungal Disease Superficial/Subcutaneous Dermatophytes Candiadiasis Sporotrichosis Systemic Exogenous Blastomycosis, Histoplasmosis, Coccidiomycosis, Sporotrichosis Opportunistic Aspergillosis, Candidiasis, Cryptococcus, Zygomycosis Immunocompromised Hosts Neonates Oncology patients Bone Marrow Transplant patients Solid Organ Transplant patients Patients with primary immunodeficiencies Patients with HIV Invasive Fungal Infections Neutropenic patients are particularly at risk for fungal infections Percent of patients with neutropenia developing invasive fungal infections: By day 20 of neutropenia, 20% of patients By day 35 of neutropenia, 60% of patients Most infections due to Candida and Aspergillus Wingard, CID 2004;39:S38-43 Classes of Antifungals Polyenes: Amphotericin B Abelcet Ambisome (1958) (1995) (1997) Nucleosides: Allyamines: Flucytosine Terbinafine (1972) (1996) Azoles: Miconazole Ketoconazole Fluconazole Itraconazole Voriconazole Posaconzole (1978) (1981) (1990) (1992) (2002) (2006) Echinocandins: Caspofungin Micafungin Anidulafungin (2001) (2005) (2006) Amphotericin B Active against most fungal pathogens, but certain species; Resistant to A. terreus, Scedosporidium, C. lusitaniae, some zygomyces. Fluconazole Active against yeasts, but not molds. Voriconazole/ Itraconazole Very broad-spectrum activity against yeasts, molds, endemic fungi, but no activity against zygomyces. Posaconazole Very broad-spectrum activity against yeast, molds (e.g. Aspergillus spp., Fusarium spp., Scedosporium spp., some zygomyces) Echinocandins Active against yeasts and Aspergillus; not very active against other molds Classes of Antifungals Polyenes: Amphotericin B Abelcet Ambisome (1958) (1995) (1997) Nucleosides: Allyamines: Flucytosine Terbinafine (1972) (1996) Azoles: Miconazole Ketoconazole Fluconazole Itraconazole Voriconazole Posaconzole (1978) (1981) (1990) (1992) (2002) (2006) Echinocandins: Caspofungin Micafungin Anidulafungin (2001) (2005) (2006) Polyenes Amphotericin B, Ambisome, Abelcet Nystatin Polyenes Mechanism: Binds to ergosterol in the fungal cell membrane leakage of the intracellular cations and cell death Selectivity is based on the difference in fungal vs. mammalian cell membrane (ergosterol vs. cholesterol) Resistance is rare and mediated by changes in ergosterol content in fungal cell membrane Amphotericin Amphotericin: Antifungal activity Most Candida & Aspergillus Does not have activity against: Candida lusitaniae & guilliermondii Aspergillus terreus & some flavus Fusarium Scedosporidium Amphotericin: Toxicity Can also bind to cholesterol Its oxidation causes free radicals **Nephrotoxicity Electrolyte abnormalities Infusion reactions Dose-dependent Increases with other nephrotoxic medications Fever, rigors, headache, nausea, vomiting Anemia Thrombophlebitis Amphotericin: Drug Interactions Synergistic (increasing uptake) Rifampin Flucytosine Tetracyclines Antagonistic Imidazoles (Ketoconazole, Clotrimazole) Amphotericin Lipid Formulations AmBisome Abelcet Amphotec Amphotericin Lipid Formulations Major advantage is that they have less nephrotoxicity Require higher doses 3 mg/kg/day for candidiasis 4-6 mg/kg/day for invasive fungal infections Decreased severity and frequency of acute infusion reactions Classes of Antifungals Polyenes: Amphotericin B Abelcet Ambisome (1958) (1995) (1997) Nucleosides: Allyamines: Flucytosine Terbinafine (1972) (1996) Azoles: Miconazole Ketoconazole Fluconazole Itraconazole Voriconazole Posaconzole (1978) (1981) (1990) (1992) (2002) (2006) Echinocandins: Caspofungin Micafungin Anidulafungin (2001) (2005) (2006) Nucleoside Analogs Flucytosine Nucleoside Analogs Mechanism: DNA substrate analog that leads to incorrect DNA synthesis Only given PO Often used in combination with Amphotericin Should not be used as monotherapy Resistance develops rapidly through alteration of cytosine permease or altered metabolism Nucleoside Analogs Nucleoside Analogs: Antifungal activity Candida & Cryptococcus Does not have activity against: Molds *Well distributed in the CNS* Nucleosides: Toxicity Bone Marrow suppression Abdominal pain Loose stools Classes of Antifungals Polyenes: Amphotericin B Abelcet Ambisome (1958) (1995) (1997) Nucleosides: Allyamines: Flucytosine Terbinafine (1972) (1996) Azoles: Miconazole Ketoconazole Fluconazole Itraconazole Voriconazole Posaconzole (1978) (1981) (1990) (1992) (2002) (2006) Echinocandins: Caspofungin Micafungin Anidulafungin (2001) (2005) (2006) Allyamines Terbinafine Allyamines Mechanism: Reduced ergosterol biosynthesis Terbinafine specifically inhibits squalene epoxidase Highly lipophilic; accumulates in skin, nails, and fatty tissue Treats dermatophytes Terbinafine Classes of Antifungals Polyenes: Amphotericin B Abelcet Ambisome (1958) (1995) (1997) Nucleosides: Allyamines: Flucytosine Terbinafine (1972) (1996) Azoles: Miconazole Ketoconazole Fluconazole Itraconazole Voriconazole Posaconzole (1978) (1981) (1990) (1992) (2002) (2006) Echinocandins: Caspofungin Micafungin Anidulafungin (2001) (2005) (2006) Azoles 5-membered organic ring with either 2 or 3 nitrogen molecules 2 = Imidazoles 3 = Triazoles Imidazoles Clotrimazole Miconazole Ketoconazole Triazoles Fluconazole Itraconazole Voriconazole Posaconazole Triazoles Mechanism Inhibits the fungal cytochrome P450 14-alpha dexamethylase; an enzyme that acts in ergosterol biosynthesis Resistance Mutations in the target enzymes Upregulation of efflux transporters Triazoles Azole Drug Interactions Azole Inhibition of CYP P450 Increased serum concentration of coadministered drug or metabolite Oral hypoglycemics S-warfarin R-Wafarin Cyclosporin Tacrolimus Sirolimus Phenytoin Carbamezepine Triazolam, alprazolam, midazolam Diltiazem Lovastatin Isoniazid Rifabutin Quinidine Protease inhibitors (saquinavir, ritonavir) Busulfan Vincristine Cyclophosphamide Digoxin Loratidine and others… Azole Drug Interactions Rifampin Sirolimus Tacrolimus Cyclosporine Corticosteroids Fluconazole: Antifungal activity Most Candida species, Cryptococcus, Coccidioides Does not have activity against: Candida krusei (intrinsically resistant) Candida glabrata (dose-dependent resistance) Aspergillus Fluconazole Excellent bioavailability Metabolized by the liver (cytochrome P450) Cleared by the kidney Required renal dosing Few side effects Can see transaminitis Itraconazole: Antifungal activity Candida, Cryptococcus, Histoplasma, Coccidioides, Aspergillus Itraconazole Absorption is not reliable 55% for the solution Less with the capsule Metabolized by cytochrome P450 Cleared by the kidney Requires renal dosing Voriconazole: Antifungal activity Candida, Aspergillus, Fusarium, Scedosporidium Has coverage for fluconazole resistant species of Candida and Aspergillus Does not have activity against: Zygomycetes Voriconazole Bioavailability > 95% Metabolized by CYP2C19 Requires renal dosing for the IV formulation PO voriconazole does not require renal dosing Side effects Visual disturbances Photosensitivity Voriconazole: Drug Interactions Sirolimus levels can be dramatically increased Not advised while on Voriconazole May need to decrease: Tacrolimus Cyclosporine Coumadin Omeprazole Posaconazole: Antifungal activity Similar to Voriconazole Candida, Aspergillus, Fusarium, Scedosporidium Includes Zygomycetes Classes of Antifungals Polyenes: Amphotericin B Abelcet Ambisome (1958) (1995) (1997) Nucleosides: Allyamines: Flucytosine Terbinafine (1972) (1996) Azoles: Miconazole Ketoconazole Fluconazole Itraconazole Voriconazole Posaconzole (1978) (1981) (1990) (1992) (2002) (2006) Echinocandins: Caspofungin Micafungin Anidulafungin (2001) (2005) (2006) Echinocandins Caspofungin Micafungin Anidulafungin Echinocandins Only given IV Mechanism of Action Block fungal wall synthesis by inhibiting the enzyme 1,3 beta glucan synthase Echinocandins Echinocandins: Antifungal activity Most Candida & Aspergillus Does not have activity against: Cryptococcus Treatment of Fever and Neutropenia Consider adding antifungal coverage for fever lasting > 4-5 days. Empiric therapy Amphotericin (Gold Standard) Ambisome Itraconazole Caspofungin Voriconazole Treatment of Candidiasis Removal of the affected central line Treatment with Amphotericin, Ambisome, or Fluconazole Fluconazole would not be appropriate if the organism is resistant. Treatment of Aspergillus Voriconazole Amphotericin/Ambisome Surgical excision may be required in some cases Conclusion Important to consider first if you are treating a mold or yeast, then direct therapy if the organism is known Different antifungals have different spectrums of antifungal coverage Questions and Comments Resources IDSA (Infectious Disease Society of America) Centers for Disease Control Doctor Fungus UpToDate 2007 The 2006 American Academy of Pediatrics Redbook PREP American Academy of Pediatrics Questions 1999-2006