Types of Cataract Surgery
advertisement

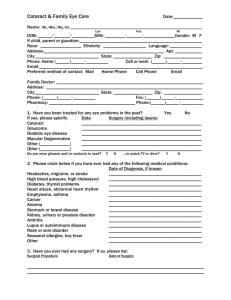
FACULTY DEVELOPMENT IN PRIMARY CARE With Support Provided by: Health Resources and Services Administration Grant # D55HP23200 Chief Complaint & History of Present Illness Chief complaint: “I have a change in vision” HPI: A 76 year old man presents with progressively worsening vision. The patient first noticed his vision getting worse about a year ago, so he went to the optometrist and got new glasses. At the time of his visit he was told he might be developing cataracts in both eyes. He now notes difficulty with reading and driving. He states that the vision loss is worse at night, so now he is afraid to drive at night because of the glare that he sees reflecting off of the other cars’ lights. In describing the vision change he states that he is seeing halos around lights when he looks directly into them. History of Present Illness Cont. He notes that the vision in both of his eyes has greatly decreased and that he sometimes sees double. He has not been able to differentiate between colors recently and he feels that most colors look “faded” to him. He is an avid reader and his vision change is greatly affecting his daily life. He is worried that he will become blind. Past Medical & Surgical History PMH: Asthma, High Cholesterol, Hypertension PSH: Angioplasty with one stent placement two years ago. Laparoscopic Cholecystectomy 10 years ago Medications & Asthma Severity Prescribed Medications: Albuterol inhaler 1 puff every 6 hours when needed. He uses his albuterol inhaler three to four times a week. He wakes up at night once a month with wheezing. He has never been intubated for his asthma, but has been hospitalized three times in the past 10 years due to asthma exacerbations. He has been on multiple courses of steroids throughout his life for Asthma. Advair diskus (fluticasone/salmeterol) inhaler 1 puff twice a day Medications and Allergies Medications Continued: Pravastatin 80 mg po q hs Hydrochlorothiazide 50 mg po q day Omega 3 fatty acids 1000 mg po q day Allergy- Aspirin- had hives Social History Patient worked as an executive in a pharmaceutical company. He retired about eight years ago and still does consulting work on the side. He traveled a lot for work and uses the computer a couple of hours per day. He lives with his wife in his multi level home. He has an active social life and a big family and support system. He is currently married and has three children from his wife and one son from a previous relationship. Drinks one cup of coffee a day, no other caffeine use. Drinks alcohol socially (about one glass of wine a month). He eats healthy and works out once a week by swimming laps at the local YMCA. Family History Mother deceased at 50 from Endometrial Cancer Father deceased at 90 from natural causes. 4 healthy children Health Maintenance Immunizations: • Influenza- this year • Pneumococcal- five years ago • Tdap 2 years ago, when grandson was born • Zostavax- never had • PPD- never had Health Maintenance • Colonoscopy about 5 years ago • Prostate exam – by urologist this year • CXR- 1 year ago • EKG- 1 year ago • Exercise stress test at Cardiologist this year. All normal Review of Systems General: Well groomed, proper hygiene Constitutional: No fevers, chills, or night sweats Skin: No lesions, no ulcers, no itching, no edema HEENT: No headache, ear pain, sinus pain or sore throat Eyes: + Cloudy Vision Breasts: No pain, no discharge, no changes noted. Respiratory: No active Dyspnea Heart: No palpitations, no dizziness, no chest pain. Hematological: No fatigue, no signs of easy bruising. GI: No reflux, no nausea, vomiting or diarrhea noted. No changes in bowel habits. No hematuria, no incontinence, no impotence Neurologic: No tremors, no headaches, paresthesias, dysarthria or gait instability. Psych: Denies anxiety or depression Comprehensive Geriatric Assessment Tools The following tools are utilized when performing a comprehensive geriatric assessment, along with a thorough history & physical exam: • • • • • • Fall Risk: Get Up and Go Test Barthal Index of ADL’s IADL’s Mini Mental Status Examination Clock Drawing Test Geriatric Depression Scale These account for the patient’s gait stability, fall risk, their functional capacity and ability to live independently, their mental status (which can vary with acute illness and can worsen with age related disease), their higher cognitive function, and any underlying depression that may worsen co-morbid conditions. Gait Stability Assessment Get up and Go Test: ■ ■ Scoring: 1 = Normal 2 = Very slightly abnormal 3 = Mildly abnormal 4 = Moderately abnormal 5 = Severely abnormal A patient with a score of 3 or more on the Get-up and Go Test is at risk of falling. The patient rises out of chair comfortably, walks forward steadily, pivots without difficulty and shows a steady gait while walking back. He scores a 1- Normal get up and go test with no gait abnormality noted. Assessment of mobility, balance, walking ability, & fall risk The Timed Up and Go Test (TUG) Instructions for administration The patient sits in the chair with his/her back against the chair back. On the command “go”, the patient rises from the chair, walks 3 meters at a comfortable and safe pace, turns, walks back to the chair and sits down. Timing begins at the instruction “go” and stops when the patient is seated. Scores range from 1 to 5 based on the observer's perception of the patient’s risk of falling. The patient should have one practice trial that is not included in the score Patient must use the same assistive device each time he/she is tested to be able to compare scores. Podsiadlo & Richardson 1991 TUG Normative Data for Community-Dwelling Older Adults Age years Gender N Mean Time (seconds) SD 95% CI 60-69 Male 15 8 2 7-9 Female 22 8 2 7-9 Male 14 9 3 7-11 Female 22 9 2 8-10 Male 8 10 1 9-11 Female 15 11 3 9-12 70-79 80-89 Steffen et al, 2002 Equipment required: standard armchair (approx. 46cm high) and stopwatch. Time to Administer: >3 min. ICF Domain: Activity Cut-Off Scores for TUG indicating risk of falls by population Population Cut-Off score (in seconds) Author Community dwelling adults >13.5* Shumway-Cook et al, 2000 Older stroke patients > 14* Andersson et al, 2006 Older adults already attending a falls clinic > 15* Whitney et al, 2005 Frail elderly > 32.6* Thomas et al, 2005 LE amputees > 19* Dite et al, 2007 Parkinson's Disease >7.95* Dibble et al, 2006 Barthal Index of ADLS Activities of Daily Living ■ ■ ■ ■ ■ ■ Bowels ■ 0 = incontinent (or need to be given enema) ■ 1 = occasional accident (once/week) ■ * 2 = continent Bladder ■ 0 = incontinent or catheterized and unable to manage ■ 1 = occasional accident (max. once per 24hrs) ■ * 2 = continent (for over 7 days) Grooming ■ 0 = need help with personal care ■ * 1 = independent face/hair/teeth/shaving Toilet use ■ 0 = dependent ■ 1 = needs some help, but can do something alone ■ * 2 = independent (on and off, dressing, wiping) Feeding ■ 0 = unable ■ 1 = needs assistance ■ * 2 = independent ■ ■ ■ ■ Transfer ■ 0 = unable – no sitting balance ■ 1 = major help (1 or 2 people, physical), can sit ■ 2 = minor help (verbal or physical) ■ *3 = independent Mobility ■ 0 = immobile ■ 1 = wheelchair independent, including corners ■ 2 = walks with help of one person (verbal or physical) ■ *3 = independent (but may use any aid, e.g., stick) Dressing ■ 0 = dependent ■ 1 = needs help, but can do about half unaided ■ * 2 = independent (including buttons, zips, laces, Stairs ■ 0 = unable ■ 1 = needs help (verbal, physical, carrying aid) ■ *2 = independent up and down Bathing ■ 0 = dependent ■ * 1 = independent (or in shower) TOTAL Score: (Circle score and calculate sum at bottom) Total possible score 0 – 20 with lower scores indicating increased disability. The patient scored a Total of 20 no Disability, no problems with transfers & the stairs. Instrumental Activities of Daily Living (IADL’s) ■ ■ ■ ■ ■ Ability to use telephone ■ * 1 = Operates phone on own initiative (looks up & dials) ■ 1 = Dials a few well-known numbers ■ 1 = Answers telephone but does not dial ■ 0 = Does not use telephone at all Laundry ■ 1 = Does personal laundry completely ■ * 1 = Launders small items; rinses stockings etc. ■ 0 = All laundry must be done by others Shopping ■ *1 = Takes care of all shopping needs independently ■ 0 = Shops independently for small purchases ■ 0 = Needs to be accompanied on any shopping trip ■ 0 = Completely unable to shop Housekeeping ■ * 1 = Maintains house alone or with occasional assistance ■ 1 = Performs light daily tasks such as dishwashing, bed making ■ 1 = Performs light daily tasks but cannot maintain acceptable level of cleanliness ■ 1 = Needs help with all home maintenance tasks ■ 0 = Does not participate in any housekeeping tasks. ■ ■ ■ ■ Mode of Transportation ■ 1 = Travels independently on public trans. or drives own car ■ * 1 = Arranges own travel via taxi but does not use public trans. ■ 1 = Travels on public trans. when assisted or accompanied by aid ■ 0 = Travel limited to taxi or car with assistance of another ■ 0 = Does not travel at all Food Preparation ■ *1 = Plans, prepares and serves adequate meals independently ■ 0 = Prepares adequate meals if supplied with ingredients ■ 0 = Heats and serves prepared meals or prepares meals but does not maintain adequate diet ■ 0 = Needs to have meals prepared and served Responsibility of own medications ■ * 1 = Is responsible for taking medication in correct dosage & time ■ 0 = Takes responsibility if medication is prepared in advance in separate dosages (pill box) ■ 0 = Is not capable of dispensing own medication Ability to handle finances ■ * 1 = Manages financial matters independently (budgets, writes checks, pays rent/bills, goes to bank) ■ 1 = Manages day-to-day purchases, but needs help with banking and major purchases. ■ 0 = Incapable of handling money Scoring: The patient receives a score of 1 for each item if his/her competence is rated at some minimal level or higher. Total score range is 0 – 8. A lower score indicates a higher level of dependence. The patient scored an 8, which is of independent function. Mini Mental Status Exam Mini Mental Status Exam: Results The patient correctly states the year and the season, he is not confused. He remembers all dates and objects. He is able to copy the object shown with the lines crossing over each other. The remainder of his MMSE had appropriate responses. His total score is 30, which reflects the highest score, no deficits Clock Drawing Test: Higher Executive Function & Dementia The patient draws the image shown in Figure A - normal Geriatric Depression Scale (15 point) Scoring: Score 1 point for each one selected. A score of 0 – 5 is normal. A score greater than 5 suggests depression. The patient scored a 1. He does not seem to have depression, but is fearful of driving at night. Physical Examination Vital Signs: BP- 126/88 Pulse- 72 regular RR-16 Temp.- 98.6 190 lbs. 5 ft. 10in. BMI=27.26 Vision Testing • Snellen Vision test was 20/40 in both eyes, without his glasses. • Visual Fields were decreased. Image: Snellen Chart Visual Acuity Testing • Contrast sensitivity testing- evaluates the ability to differentiate between an object and its background. • Contrast sensitivity was decreased in this patient. www.nap.edu Visual Impairments: Pelli-Robson contrast sensitivity chart (Pelli, Robson, & Wilkins, 1988) Visual Acuity Testing Cont. ■ Glare testing- done with a Brightness Acuity Test (BAT) to simulate glare from an artificial light source. Patients with cataracts may have good distance visual acuity in a dimly lit room, but experience a reduction in acuity from a bright light. * This patient had a reduction in visual acuity by the bright light* http://exton-vision-center-optometry.eggzack.com/cataract-testing Visual Acuity Testing Cont. Potential Acuity Meter (PAM) test projects an eye chart directly onto the retina the lens. This is often useful in estimating how much the cataract is contributing to the patient’s visual loss. ■ Color Vision Testing assesses the optic nerve and macula. ■ Optical coherence tomography (OCT) is probably the most helpful test for diagnosing macular pathology. ■ Pupil testing must be performed in all patients! * This patient had a decrease in visual acuity with these tests, but his pupils responded normally to light. ■ http://exton-vision-center-optometry.eggzack.com/cataract-testing Physical Examination • • • • • • • • • • General appearance: NAD, A&Ox3 Eyes: Pupils equally reactive to Light and Accommodation HEENT: TM intact b/l no erythema, no mastoid, no tragal tenderness. No erythema on tonsils. Negative sinus tenderness to palpation. No bruits, No cervical lymphadenopathy, neck supple, no thyromegaly Neuro: Cranial nerves 2-12 grossly intact bilateral, sensation intact b/l face, negative Brudzinski's sign, negative Kernig's sign, muscle strength intact bilateral upper and lower extremities. All Reflexes Normal, sensation to bilateral upper and lower extremities intact. Lungs: CTA B/L CVS: s1s2, RRR Abdomen: NT, ND, positive bowel sounds in all 4 quadrants, obese Back: No CVA tenderness Extremities: Normal VISION DECREASED BILATERAL EYES Laboratory Tests WBC: 5.6 Hb: 14.0, HCT: 38.7 PLT 265 FLP- Total cholesterol 200, triglycerides 130 HDL 70, LDL 130 Liver and Kidneys Normal Thyroid Function Tests Normal Glucose 105 (nonfasting) PSA 1.0 Negative Lymes titer RPR negative Vitamin B12, Folate and Vitamin D 25-OH normal Slit Lamp Exam Image From: http://en.wikipedia.org/wiki/Cataract Right Eye Left Eye Cataracts This patient was found to have a decrease in bilateral vision and Cataracts in both Eyes. This patient has a history of steroid use due to Asthma which could have contributed to his Cataract development. Causes of Cataracts: Age- As people age the protein in the eye clumps together forming a Cataract. Injury- Traumatic Cataract Wilson’s Disease- Genetic disorder where copper accumulates in organs. Down’s Syndrome Viruses and Bacteria Causes of Cataracts: Medication – i.e. Steroids, such as Prednisone Hypothyroidism Hyperparathyroidism Familial Genetic Cataracts Diabetes Mellitus Nicotine use (Tobacco Smoking) Causes of Cataracts: Sunlight- there is an increase incidence of Cataracts with exposure to UV Rays Statins- According to New Study by the NIH statins can increase the Incidence of Cataracts. http://well.blogs.nytimes.com/2013/09/25/statins-tied-to-cataract-risk/?_r=0 Causes of Congenital Cataracts: Congenital Cataracts due to Viruses, Bacteria or Parasites: • Herpes Simplex Virus • Rubella • Toxoplasmosis • Syphilis • Cytomegalovirus Cataracts ■ A cataract is an opacity in the crystalline lens of the eye. They cause degradation of vision and distort light passing through the lens. Cataracts are common in the elderly and 60% of Americans over the age of 60 have cataracts. Over 1.5 million cataract surgeries are done in the US annually. ■ The predominant complaint of patients with Cataracts is gradual vision loss. Patients also complain of blurry vision, glare, problem seeing when bright lights are present, and double vision. Treatment of Cataracts Most treatment of cataracts revolve around the patient’s vision complaints. If vision loss is severe and affects the patient’s quality of life, then Cataract Surgical Extraction is recommended. This is done by an Ophthalmologist. Most standards of surgery are when Vision by the Snellen chart is 20/40 or worse in the eye with the cataract. Cataract Surgery Cataracts are usually removed by the extracapsular technique in which the cataract is removed and a new lens is put in place. Laser treatment is sometimes required after the cataract is removed. In the US, Cataract surgery has approximately a 95% success rate. Types of Cataract Surgery 1. Phacoemulsification: Using a microscope the ophthalmologist makes an incision in the surface of the eye in or near the cornea. An ultrasound probe is placed in the eye and vibrations are used to dissolve the clouded lens. The fragmented pieces are then suctioned out through the same probe. Once the cataract is removed, an artificial lens is placed in the capsule. http://www.medicinenet.com/cataract_surgery/page3.htm#types Types of Cataract Surgery 2. Extracapsular cataract surgery: This procedure is used mainly for very advanced cataract that cannot be phacoemulsified. A large incision is made to remove the whole lens and an artificial lens is placed in the capsule. http://www.medicinenet.com/cataract_surgery/page3.htm#types Types of Cataract Surgery Cont. 3. Intracapsular cataract surgery: Ophthalmologist removes the lens and capsule and the new lens is placed in the iris. This is an uncommon type of cataract surgery but is used in traumatic cataracts. http://www.medicinenet.com/cataract_surgery/page3.htm#types Cataract Surgery Risks • • • • • • • • Inflammation after extraction Infection Bleeding Swelling Retinal detachment Glaucoma Secondary cataract Loss of vision Cataract Surgery Low risk Procedure is about an hour in length Usually requires Pre Operative Clearance Can be done in a same day ambulatory surgery setting or in a Hospital Operating Room Anesthesia for Cataract Surgery • Most cataract surgery is done using a topical anesthetic (eye drops) and/or under local anesthesia and sedation. • General Anesthesia is rarely used for Cataract Surgery and is used for patients with: Severe Anxiety Allergy to local anesthesia Children Cataract Treatment for this pt This patient was referred to an Ophthalmologist who recommended bilateral Cataract extraction under local sedation using the phacoemulsion technique. Follow Up Visit The patient saw his Ophthalmologist five days after surgery and was given a slit lamp exam and a Vision Test, which showed his vision improved after surgery. Two month Follow Up ■ Patient seeing well, able to read and drive at night. ■ He is back to taking his Omega 3 Fatty Acids and his Asthma is better controlled. Osteopathic Considerations In this 76 year old with bilateral cataracts and chronic asthma with periodic steroid use, there are several ways that osteopathic treatment can add to his treatment. In a patient with lifelong asthma and intermittent steroid use, there will be somatic dysfunctions from the asthma itself and from the chronic use of accessory muscles of breathing. Osteopathic treatment can reduce these somatic dysfunctions and reduce the work of breathing and could have a positive effect on the frequency, duration and severity of his chronic exacerbations. This could, in turn, reduce frequency and dosage of corticosteroids in the future. Osteopathic Considerations Cont. Additionally, manipulation of the eye via instrumentation and the procedure itself can cause cranial somatic dysfunctions, increased inflammation and swelling, which can be aided through maintaining cranial base mechanics. The vast majority of venous drainage from the skull is via the jugular vein. The jugular vein drains through the jugular foramen which is situated between the petrous portion of the temporal bone and the occiput. Checking this important area in this patient can help with drainage and may reduce swelling and help with pain, both of which can augment the healing process. Osteopathic Structural Exam • Cranial- zygoma depressed and restricted on R, temporal internally rotated on L OA ERrSBl,suboccipital tissues boggy with acute tissue texture changes and tenderness, R occipito-temporal restriction • C- C2 Rl, chronically tense SCM’s b/l, Scalenes tense L, tender points throughout • T-R- compliance of the thoracic cage reduced, stiffness through ribcage and T-spine, paraspinal muscles tense T3-L5 b/l, 12th rib inferior and post b/l, iliopsoas hypertonicity b/l. • Diaphragm- diminished motion inhalation and exhalation Osteopathic Treatment This patient would benefit from treatment as quickly as possible, even right after surgery, but most likely he would be seen several days post op. Because of his age, familiarity or lack of familiarity with osteopathic treatment and the acute nature of his situation, only gentle treatments should be used. • cr- a simple gentle base spread/ V- spread technique could help with temporal dysfunction and facilitate greater drainage from the face via jugular foramen “opening”. Gentle myofascial release and OA decompression should be tolerated and effective. • Thoracic cage- gentle seated articulatory technique to reduce thoracic and rib somatic dysfunctions and decreased compliance of thoracic should be effective and tolerated but if not, supine rib raising would be an additional or substitute treatment. Treatment Continued • R- BLT to 12th rib and or counterstrain to psoas tender points could be used to release iliopsoas and help with over diaphragm motion. • C- counterstrain and myofascial release techniques also should be well tolerated and effective, BLT could also be very effective and safe in this post op patient with acute and chronic somatic dysfunctions Internet References http://exton-vision-center-optometry.eggzack.com/cataract-testing http://en.wikipedia.org/wiki/Cataract http://well.blogs.nytimes.com/2013/09/25/statins-tied-to-cataract-risk/?_r=0 http://www.medicinenet.com/cataract_surgery/page3.htm#types http://www.nlm.nih.gov/medlineplus/cataracts.html References ▪ Current Medical Diagnosis and Treatment, Chapter 7 Disorders of the Eye and Lids on Access Medicine Accessed on December 8, 2013. ▪ Paine, D. et al Cataracts on Emedicine Health Assessed December 7, 2013. References • • • • • • Cheak-Zamora, N. C., Wyrwich, K. W., & McBride, T. D. (2009). Reliability and validity of the SF-12v2 in the Medical Expenditure Panel Survey. Quality of Life Research, 18 (6), 727–735. Podsiadlo, D. and Richardson, S. (1991). "The timed "Up & Go": a test of basic functional mobility for frail elderly persons." J Am Geriatr Soc 39(2): 142-148. Nasreddine, Z. S., Phillips, N. A., et al. (2005). "The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment." Journal of the American Geriatrics Society 53(4): 695-699. Rossetti, H. C., Lacritz, L. H., et al. (2011). "Normative data for the Montreal Cognitive Assessment (MoCA) in a population-based sample." Neurology 77(13): 1272-1275. Steffen, T. M., Hacker, T. A., et al. (2002). "Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds." Physical Therapy 82(2): 128-137. Ware JE, Kosinski M, Keller SD (1996). A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 34(3):220-233. (SF-12v1) Special Thanks to… Clinical Case by: Dr. Bernadette Riley, DO Mary Adar, DO, Assistant Professor, Dept. Family Medicine, NYIT College of Osteopathic Medicine Joseph Simone, DO Corri Wolf, PA-C, MS, RD, Assistant Professor, Dept. Physician Assistant Studies, NYIT School of Health Professions Rosemary Gallagher, PT, DPT, GCS, Assistant Professor, Dept. Physical Therapy, NYIT School of Health Professions B. Suzanne Diggle-Fox, PhD, RN, Assistant Professor, Dept. Nursing, NYIT School of Health Professions Grant Director: David P. Yens, PhD, Associate Professor, Family Medicine, NYIT College of Osteopathic Medicine