Epidermis
advertisement

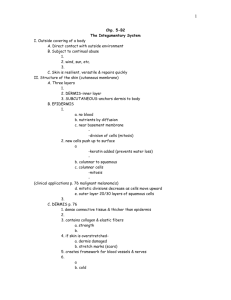
Biology 141 Integumentary System Chapter 5 The Integument Integument: Skin – largest body organ Integumentary System: – Skin – Hair – Nails Function: – Protection – Maintain body temperature – Provide sensory input Dermatology: medical specialty dealing with the integumentary system Structure of the Skin Cutaneous membrane: skin – Epidermis – superficial layer – Dermis – deep layer Subcutaneous membrane – Hypodermis – fat layer; not technically a part of the skin. Structure of the Skin The 2 layers of skin; – epidermis Multilayered epithelial tissue thinner – Dermis Connective thicker tissue Epidermis Cell types found in the epidermis: – Keratinocytes: multilayered Produce keratin protein (tough, water repellant) – Melanocytes Produces pigment melanin to protect nuclear DNA in keratinocytes – Langerhans cell Immune response – Merkel cells Contact Merkle discs to detect sensations Epidermis Tissue Layers Composed of different strata (layers) – outermost - dead cells – Innermost - Cells divide Cells Layers die as they are pushed upward originate from the deepest cell layer of columnar cells called the stratum germinativum. Sublayers of the Stratum germinativum Stratum basale ("base layer") – Cells of stratum basale are closest to the blood supply in the dermis and are thus the healthiest – Only these cells can reproduce Stratum spinosum ("spiny layer") – Cells are pushed from below and become "squished" and look "spiny" on cross sectional view – Because the cells are farther away from the dermal blood supply, they are less healthy and thus don't reproduce Basal Cell Carcinoma Low magnification (left) of skin cross-section of shows different layers (epidermis, dermis and subcutaneous tissue), and areas of tumor invasion. Higher magnification (right): tumor cells resemble those in the normal basal cell layer of the epidermis. Tumor cells appear to bud off from the epidermis and grow downward as islands and cords of basophilic cells with hyperchromatic nuclei. Epidermis Tissue Layers (deep to superficial) Stratum germinativum ("growth layer") – stratum basal – germination basement layer – Stratum spinosum – “thorn-like” Stratum granulosum "grainy layer" Stratum lucidum "clear layer" Stratum corneum “horny layer” (top layer) Epidermis: Tissue Layers stratum basal: – Single row of cuboidal or columnar keratinocytes. – Some are stem cells – Contains Melanocytes Langerhans cells Merkle cells and discs Epidermis: Tissue Layers stratum basal – – Damage to this layer damages stem cells Unable to regenerate skin Require skin grafts Grafts can be autologous (same individual) or transplanted from a donor. – Skin sheets can also be grown in the lab Epidermis: Tissue Layers stratum spinosum – multilayered keratinocytes – Few Langerhans cells and Melanocytes Epidermis: Tissue Layers stratum granulosum – Multilayered, flattened keratinocytes – Cells undergoing apoptosis – Secretes water repellant – cells loose nuclei, appear grainy – Keratohyalin (a precursor to keratin) forms in granules here Epidermis: Tissue Layers stratum lucidum: – Multilayered, dead keratinocytes with large amount of keratin – Translucent and flattened – Found only in thick skin (hairless) Fingertips Palms soles Epidermis: Tissue Layers stratum corneum: – – – – – Multilayered Flat, dead keratinocytes primarily keratin protein "horny layer" - cells have processes Flattened cells filled with keratin form "keratinized layer" and make this "keratinized stratified squamous epithelium" – Constant friction results in callus formation Dermis Dermis: – Connective tissue – Contains Blood vessels Nerves Glands Hair follicles Dermis 2 main regions: Papillary: upper layer Reticular: deep layer Dermis Papillary: upper layer lies next to the epidermis contains the derma papillae (projections into the upper epidermis) – epidermal ridges creat fingerprints, palm prints and footprints. – Contain capillaries – Contain Meisssner corpuscles (tactile receptors) – Contain free nerve endings Senses temperature, pain, itch, tickle Dermis Reticular: deep layer Attaches to the subcutaneous layer Dense irregular connective tissue contains more collagen fibers – increasing the strength of the skin. Contains: – Few adipose cells – Hair follicles – Nerves and Pacinian corpuscles (deep pressure) – Sebaceous glands (oil) – Sudoriforous glands (sweat) Accessory Structures Receptors: Meissner’s corpuscles and Pacinian corpuscles Meissner’s: located in the papillary layer of dermis – project into the papillae. – touch receptors Pacinian: spherical, onion-like – Lie deep in the reticular layer – pressure Sensory receptors in the Dermis Meissner’s Corpuscle detects light touch Papillary layer Pacinian Corpuscle detects deep touch (pressure) Reticular layer Dermis Tears in the reticular region of the dermis result in stretch marks. Incisions against the grain of the collagen fibers = wide scar Incisions with the grain = thin scar Structural Basis of Skin Color Skin color pigments: – Melanin – Hemoglobin – Carotene Melanin – number of melanocytes the same in all people – Amount of melanin produced varies – Accumulation results in Age spots Freckles moles Melanin Function: – Absorbs UV radiation – Prevents damage to DNA in epidermal cells – Neutralizes free radicals Hemoglobin Found in RBCs Skin color depends on amount of oxygen in the blood – Blue – cyanotic: low oxygen – Yellow - jaundice: high bilirubin Liver damage – Red – erythema: engorgement of capillaries Injury Heat Infection Inflammation Allergic reaction – White – pallor: low number of RBC Shock anemia Carotene Yellow-orange pigment found in egg yolks and orange vegetables – Precursor to vitamin A – Excessive dietary intake results in accumulation in the subcutaneous layer Albinism / Vitiligo Albinism: Inherited inability to synthesize melanin – Melanin is not produced in skin, hair, and eyes. Vitiligo: partial or complete loss of melanocytes in patches of skin – Immune system attacks and destroys melanocytes. Accessory Structures Hair: pili Columns of dead, keratinized cells compactly cemented together. hair shaft – portion of the hair that projects above the surface. root – portion below the surface extending into the dermis. Hair Hair shaft and root consist of 3 concentric layers of cells: – Medulla – Cortex – Cuticle Human Hair Cuticle showing scales No medulla, brown pigment granules in cortex Light medulla Hair Hair follicle: composed of the root sheath – encasement with 2 layers: – Internal root sheath produced by matrix, surrounds root – External root sheath extension epidermis of The Dermal root sheath is part of the dermis Hair bulb - enlarged region of the root containing the follicular papilla (involution of loose connective tissue). Hair arrector pili muscle – smooth muscle that upon contraction forces the skin into goose bumps. Accessory Structures Glands: sebaceous and sweat glands Sebaceous glands: Usually connected to hair follicles secretes sebum (oil) Moisturizes hair and skin – keeps hair pliable. – Keeps skin soft – Inhibits bacteria Acne: Inflammation of a sebaceous gland. Normal sebaceous gland Blocked sebaceous gland Sudoriferous Glands (Sweat glands) 2 main types of glands: eccrine and apocrine eccrine: – empty directly out through the skin surface – tubular with a coiled basal portion located deep in the dermis – Regulates body temperature apocrine: – – – – larger, empty directly into the hair follicle canal secretory portion located in the subcutaneous layer Excretory duct opens into hair follicle stimuli: psychic factors; emotions, sexual excitement Sudoriferous Glands Accessory structures and location Ceruminous Glands Modified ear. sweat glands in the external – Produce ear wax (cerumen) – Provides a sticky barrier Nails Tightly packed, hard, keratinized epithelial cells. Structure: – Nail body: visible portion Pink due to capillary bed – Free edge: part that extends past the digit White due to lack of capillaries – Nail root: portion buried in a fold of skin Nails Types of Skin 2 types of skin based on structure: – Thin (hairy) skin – Thick (hairless skin) Functions of the Skin Thermoregulation: – by sweat and blood flow – Excrete salts, water, and small amounts of CO2 and urea – Absorbs lipid molecules (vitamins A,D,E and K, drugs, lotions, poisons, heavy metals, steroids) Blood reservoir – 8-10% of blood flow Protection – Against external assault Cutaneous sensations – Tactile, pressure, pain, temperature, tickle Excretion and absorption Synthesis of vitamin D – UV light activates precursor molecules that can be modified by the liver. Vit. D produces calcitrol which aids in the absorption of calcium in the GI tract. Maintaining Homeostasis: Skin Wound Healing Wound routes: healing can occur via 2 – Epidermal Wound Healing – affects only the epidermis. – Deep Wound Healing – wound extends to dermis and subcutaneous layers Epidermal Wound Healing Injury response: – Basal cells detach from the basement membrane. – Hormone (epidermal growth factor) stimulates basal stem cells to divide to replace migrating cells. – Migrating cells move across wound – Cells stop migrating upon touching other cells (contact inhibition) Deep Wound Healing 4 phases: – Inflammatory: clot formation closes the wound, WBC kill invaders – Migratory: scab formation, epithelial cells migrate, fibroblasts produce fibrin for scar tissue – Proliferative: Extensive growth of epithelial cells, depositing collagen fibers – Maturation: Scab sloughs off, collagen fibers organize Development of the Integumentary System Epidermis is derived from the ectoderm Dermis is derived from the mesoderm Aging and the Integumentary System Most changes occur in the dermis – Collagen fibers decrease in number – Elastic fibers loose elasticity – Fibroblast (produce collagen and elastin) decrease in number – Decrease number of melanocytes – gray hair – Subcutaneous adipose tissue is lost – Healing is longer Sun Damage UV A rays: – Not absorbed by the ozone layer – Penetrate deep into skin and absorbed by melanocytes – Depress the immune system – Darken the skin UV B rays: – Some absorbed by ozone – Penetration of skin not as deep – Cause sunburn Sun Damage Sunscreen – Absorb UV B, but allow UV A rays to reach the skin Sunblock – Block both UV A and UV B rays Skin Cancer Basal cell carcinoma – 78% of all skin cancers – Tumors arise from the stratum basale – Rarely metastasize Squamous cell carcinoma – 20% of all skin cancers – Arise from squamous cell of epidermis – metastasize Malignant melanoma – 2% of all skin cancers – Arise from melanocytes – Metastasize rapidly (can kill within months) Skin Cancer Basal cell carcinoma squamous cell carcinoma melanoma Burns Burns are graded by severity: – First degree: only epidermis, red – Second degree: all epidermis and part of dermis, blisters – Third degree: all epidermis, dermis and subcutaneous layers, black – Fourth degree: muscle layers are burned Burns Half of all patients with over 70% of the body burned, dies. Estimating surface area for burns uses the rule of nines. Burns Head and neck (front and back) – 9% Each upper limb (front and back) – 9% Trunk (front and back) – 4 x 9% (or 36%) Each lower limb – 9% front – 9% back Perineum (anal and urogenital region) – 1% Pressure Ulcers Decubitus ulcers caused by constant deficiency of blood flow from prolonged pressure against an object. Occur most often in bedridden patients.