Chapter 3 Health Appraisal
advertisement

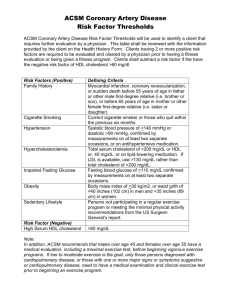
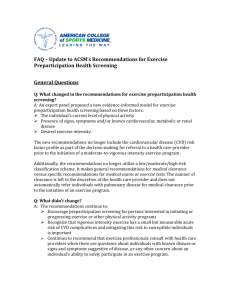
Chapter 2-3 Health Appraisal Pre-Assessment Screening & Risk Factor Assessments Key Issues In Chapter 3 • Always obtain a medical history or pre-exercise health risk appraisal on each participant. • Stratify individuals according to their disease risk. • Refer high-risk individuals to a healthcare provider for medical evaluation and a graded exercise test. Rationale for pre-testing and screening • Risk of both cardiovascular and musculoskeletal injuries are associated with exercise. • The risks increase with the intensity of the exercise. • The risks increases also in those individuals with known or previous injuries/diseases. • Therefore, it is crucial to know the medical history of individuals perform Health-Related Physical Fitness Testing • Physical fitness testing is useful for the following: – Identifying adverse S/S or conditions that might compromise well-being during exercise. – Provides an opportunity for individuals to be educated and motivated to adopt more healthful lifestyles – Helps in establishing goals to progress toward, and to evaluate progress. Rationale for Screening • Identify those with medical contraindication (see box 2.2 p. 17). • Identify those who should receive medical evaluation by MD prior to testing. • Identify those who should perform HRPF assessments administered by professional in clinical setting. • Identify those with other health risk/medical concerns. Pre-participation Health Screening • All facilities that offer exercise equipment or services should conduct pre-participation health screening of all new members and/or prospective users, regardless of age. • Conduct pre-participation health screening using one or more of several different instruments: – Comprehensive medical/health questionnaire (p. 20-21, 25). – Physical Activity Readiness Questionnaire (PAR-Q). – ACSM Risk Stratification Guidelines Types of Screening Instruments • A comprehensive medical/health questionnaire should include: – Medical diagnosis – Previous physical exam findings – History of symptoms – Recent illness, hospitalization, new medical diagnosis or surgical procedures – Orthopedic problems – Medication use and drug allergies – Lifestyle habits – Exercise and work history – Family history of disease • The PAR-Q is preferred when testing large numbers of individuals in a short period of time in a basic fitness assessment. Participants are directed to contact their physician if they answer “yes” to one or more questions. • The ACSM has low, moderate, and high risk strata based on the presence (or absence) of different risk factors. See page 18 (ACSM) ACSM Risk Stratification: Counting Risk Factors Box 2.2 ACSM 1. Family history (MI, coronary revascularization, or sudden death before 55 yrs in father or other male first-degree relative, or before 65 yrs in mother or other female first degree relative). 2. Cigarette smoking (current cigarette smoker or those who quit within the previous 6 months). 3. Hypertension (SBP 140 >mm Hg or DBP >90 mm Hg, confirmed on at least 2 separate occasions, or on antihypertensive medication). 4.Hypercholesterolemia: LDL>/=130; HDL<40; TC>/=200; or on lipid lowering medication. 5.Age: Men >/= 45, Women >/= 55 Blood Pressure Guidelines Systolic (mm Hg) Normal Pre-hypertensive Stage I Stage II <120 Diastolic (mm Hg) <80 120-139 140-159 80-89 90-99 >160 >100 ACSM Risk Stratification: Counting Risk Factors (cont) 6. Prediabetes: (fasting blood glucose of >110 mg/dl, confirmed by measurements on at least 2 separate occasions). 7. Obesity (body mass index of >30 kg/m2, or waist girth of >100 cm). 8. Sedentary lifestyle (persons not participating in a regular exercise program or meeting the minimal physical activity recommendations from the U.S. Surgeon General’s report—accumulating 30 minutes or more of moderate physical activity on most days of the week • • • • • ACSM: Check for these major signs or symptoms (Box 2.3, p. 23 ACSM) 1. Pain, discomfort (or other anginal equivalent) in the chest, neck, jaw, arms, or other areas that may be due to ischemia. 2. Shortness of breath at rest or mild exertion. 3. Dizziness or syncope. 4. Orthopnea (discomfort in breathing which is brought on or aggravated by lying flat) or paroxysmal nocturnal dyspnea (acute difficulty in breathing appearing suddenly at night, usually waking the patient after an hour or two of sleep). 5. Ankle edema. ACSM: Check for these major signs or symptoms (cont) • 6. Palpitations (forcible or irregular pulsation of the heart, perceptible to the individual, usually with an increase in frequency or force, with or without irregularity in rhythm) or tachycardia (rapid beating of the heart, typically over 100 beats per minute at rest). • 7. Intermittent claudication (a condition caused by lack of blood flow and oxygen to the leg muscles, characterized by attacks of lameness and pain, brought on by walking). • 8. Known heart murmur. • 9. Unusual fatigue or shortness of breath with usual activities. Using Screening Results for Risk Stratification • Once symptom and risk factor screening has been conducted using questionnaires, the individual considering exercise testing and prescription should be stratified according to disease risk. Stratification according to disease risk is important for several reasons: – To identify those in need of referral to a healthcare provider for more extensive medical evaluation. – To ensure the safety of exercise testing and participation. – To determine the appropriate type of exercise test or program. ACSM Risk Stratification Levels Box 2.1 ACSM Low risk: asymptomatic and meet no more than one risk factor threshold). Moderate risk : asymptomatic and meet the threshold for two or more risk factors. High risk: individuals with one or more signs/symptoms or known cardiovascular, pulmonary, or metabolic disease including diabetes mellitus. ACSM Recommendations for (A) Current Medical Examination* and Exercise Testing Prior to Participation and (B) Physician Supervision of Exercise Tests Low Risk Moderate High Risk Risk A. Moderate Exercise** A. Vigorous Exercise † † Not necessary† Not necessary Recommended Not necessary Recommended Recommended Not necessary Recommended B. Submaximal Test Not necessary B. Maximal Test Not necessary Recommended‡ Recommended * Within the past year. ** 3-6 METS; brisk walking; pace that can be sustained for 45 minutes; 40-60% maximal oxygen uptake. † Not essential, but not viewed as inappropriate. † † >6 METS; substantial cardiorespiratory challenge; >60% maximal oxygen uptake. ‡ Physician should be in close proximity and readily available. Other Issues •Informed consent (see ACSM P. 13). •Health/fitness facility standards and guidelines (Human Kinetics) •Certification Concepts and Purposes in Physical Fitness Testing Test Criteria Rationale: 1. Validity 1. To assess current fitness levels 2. Reliability 2. To identify special needs 3. Norms 3. To evaluate progress 4. Economy 4. To motivate and educate