Improved Access, Efficiency & Capacity in Specialty
advertisement

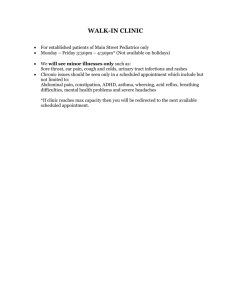
Advanced Access/Office Efficiency for Specialists www.pspbc.ca What are we trying to accomplish? Decrease the wait of patients for an appointment with a specialist Decrease the time patients spend at an appointment with a specialist Increase the use of a care delivery mechanism that is efficient, effective, and improves capacity (Group Medical Visit) Improve the provider and staff experience Improve the patient experience and outcomes 2 “Every system is perfectly designed to get the results it gets.” Systems work more efficiently, more effectively, and at a lower cost when they work with no delay 3 What’s the current state in your “system”? 4 What if…. You could offer your patients an appointment with the specialist of their choice at a time that was convenient for them? What would it take? © Tantau & Associates 5 Traditional model 100% booked Saturated schedules into the future No flexibility Triage & rework using expensive resources (MD and RN) Multiple appointment types Urgents and routines juggled Capacity: overbook and over there Continuity: delayed “Do last month’s work today.” 6 Advanced Access Model 65% open Referred patients are offered an appointment with any provider within five days Backlog eliminated (good vs. bad) Continuity is improved/maintained Capacity for new patients is increased Optimal ratio of new:return is maintained Increased patient, physician and staff satisfaction 35% booked Change how to do follow up “Do today’s work today.” 7 Benefits of Improved Access In Specialty, care is better, physicians, staff and patients are happier, costs are lower, and income is increased when the right people receive the right care and with minimal delay Decreased no-shows (decreased waste) Improved outcomes (more timely) Increased patient and referring GP satisfaction Increased provider and staff satisfaction Decreased cost/visit 8 Key Concepts for Access Improvement Balance demand and supply daily › Shape the demand for new and return › Reduce or plan for supply variation Reduce backlog Reduce scheduling complexity Optimize the care team 9 Measure of Access (delay): 3rd Next Available Appointment Choose appointment type Select day & time (e.g. Mondays at 11:00) Count days a patient waits Repeat weekly and chart Gold standard for 3rd next for specialist: 5 days 10 Ideal Access Aim Office Based Medical Specialty: › To offer an appointment within 5 days of the date of referral. Surgical Specialty: › To offer a surgical date within 5 days of agreeing that a surgical intervention is recommended. ©Tantau & Associates 11 Supply and demand Demand (referrals plus caseload) Caseload: creates real work reservoir Waiting: creates re-work waiting Supply (physician available to do the work) 12 Supply Number of appointment slots available to patients in a given day Needs to balance the demand for appointments Constant tension between new and return visits that must be taken into account 13 Demand (requests for services/time) New: › Referral from GP office › Referral from ER › Telephone calls › Specialist to Specialist referral › Returns (Follow-up) Physician-initiated (internally generated) › Requests patient come in for a follow-up visit (which is booked today) …/ 14 Balancing Supply and Demand Measure supply and demand Match demand with supply › Build in adjustments for predictable blips (long weekends, etc.) › Reduce appointment types (increases flexibility, patient focused) › Consider group visits to increase supply 15 Measuring Supply Choose a typical week in the future Count every available appointment slot Count pre-defined double-booking slots as two Does not include time booked for admin, teaching, rounds, etc. Result = available slots per week to meet patient demand 16 Measuring Demand Record every request for an appointment whether or not an appointment is booked Track “new” vs. “return” demand Count appointment requests from all sources (all referrals for a consult) Count the demand on the day request comes in 17 Determine Practice Caseload Paper records – count active charts EMR Billing software 18 Backlog Delay in your system which represents scheduled, but currently unmet clinical service Two types: › Good backlog = appropriate follow-up/planned future appointments › Bad backlog = today’s work pushed into the future e.g., patient needs to be seen today but cannot be accommodated To calculate backlog: › Count total booked appointments until 3rd next; Subtract “good” backlog. Balance = true backlog 19 Clearing Backlog Ideas: › Add ½ hour a day or a few hours a week › Increase hours on busiest days › Move some appointments from the future to any open slots in today or tomorrow’s schedule › Offload work (e.g., shared practices) › Increase supply – locum, RN, etc. …/ Continue to try to do today’s work today 20 Clearing Backlog Ideas › Review future schedule to determine appropriateness of appointments Reduce frequency for follow-up visits? › Adjust schedule to match trends › Block some :10 minute ‘do not book’ slots › Reduce appointment types short for regular visits/ long for physicals, etc. Continue to try to do today’s work today 21 Clearing Backlog – Long Term Ideas Make better utilization of MOA, RN, LPN and other team members’ skills to: – take BP, weight etc. – discuss medications with patient – review lab results – take patient histories • Consider group visits Continue to try to do today’s work today 22 Reducing Scheduling Complexity How many types of appointments do you have? Does your day follow your schedule of appointments as anticipated? Do you start and end appointments and your day on time? Reduce the number of appointment types you use Ensure truth in scheduling, i.e. schedule according to clinical need rather than template or habit Use “Freeze-Unfreeze” for “time out of office” such as vacation 23 Freeze / Unfreeze A “Practice Re-entry Survival Plan” Before holidays, all appointment slots for the physician’s first week back are frozen During the last week of the physician’s vacation, the MOA will gradually unfreeze part of the first week back from vacation 24 Benefits of Improved Office Efficiency Appointments start and end on time Work days start and end on time The office visit is optimized; patient-provider time is protected Rework and duplication of work is decreased, thereby increasing capacity › Rooms › Staff › Provider Satisfaction of patient, staff and provider are increased Costs/visit are decreased Income is increased 25 Key Concepts for Improving Efficiency Work is streamlined and standardized where possible The care team’s roles are optimized Needs are predicted and anticipated Source: IHI.org 26 Measure of Office Efficiency – Cycle Time This is a measure of the time an appointment takes for the patient The measure includes time between “check-in” and “check-out” Includes all segments of an appointment, including providerpatient interaction In Specialty, this may include more than one provider in the course of a visit Can be captured with the assistance of the patient 27 Get to Know Your Work 1. Complete assessment of common practice processes Each staff member has opportunity to evaluate what works well and what doesn’t › Evaluate the current state of these processes 2. Complete a clinic walk-through 3. Map your processes 28 Know your processes – activity Each practice team member fills out the “Know your Processes: Specialty” form You have ___ minutes for this activity 29 Steps for Improvement Each of the processes identified for improvement should be mapped in its current state Once you have mapped the current state of a process, identify some possible small tests of change that could improve the process Use the Plan, Do, Study, Act (PDSA) cycle to try small tests of change Measure baseline and outcomes 30 Process Mapping What is a “process”? › A series of connected steps or actions with an identifiable start and end point › Leads to a specific outcome Why map a process? › It illustrates “how things work in our clinic or program” › Includes several perspectives › Starting point for improvement 31 Process Mapping Oval - the start and end of the process Box - the tasks or activities of the process Diamond - a question is asked; a decision is required Arrow - the direction or flow of the process 32 Process mapping – activity Instructions In your groups, create a process map to illustrate one of the processes identified in “Know Your Processes” Start point: …………… End point: …………… You have ___ minutes for this activity 33 Analyze the process Where are the hand-offs? Is it clear who does what? Where are the delays? Is there duplication or rework? Are there identifiable areas where a small change could make an improvement? 34 Clinic Walk-through Have a staff member pose as a patient and walk-through a clinic process Tell the staff about the walk-through and ask them to act normally Start the process with the pre-process step and continue the process through to completion Document the starting time of each step in the process, what works well, what does not work well, what thoughts you have for improvement, what feelings you experienced during the process 35 Cycle Time - Patient flow through the clinic Patient enters clinic Registration Pre-Red Zone Clinic Room Provider-Patient Interaction Completion of procedures/orders Cycle time Red Zone Post-Red Zone Checkout Non-appointment time = 36 Improved Cycle Time - Patient flow through the clinic Patient enters clinic Registration Clinic Room Provider-Patient Interaction Completion of procedures/orders Checkout Non-appointment time = Pre-Red Zone Cycle time Red Zone Post-Red Zone 37 Optimize the Practice Care Team Who does what? Who could do what? Who should do what? 38 Structured Huddle What it is Brief morning meeting to › review schedule › deal with issues left over from previous day › anticipate needs for current day › give ‘heads up’ for anything special to be aware of › Brief – no more than 5-10 minutes Why use it Being proactive › helps ensure smoother patient flow › may help divert potential problems › improves communication between team members 39 http://adventuresinimprovingaccess.blogspot.com 40 Practice team activity – Planning for your small test of change What are we trying to accomplish? (Aim) How do we know a change is an improvement? (Measures) What changes can we make that will result in an improvement? Draft your small test of change with your practice team (e.g. each physician and MOA) Share your plan with the group (report-out) You have … minutes for this activity 41 Closing Next visit to be held ________ Don’t forget to send in your information for CMEs and remuneration for your time Good luck with your changes! 42