Renal Cases
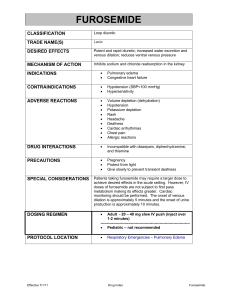
advertisement

Physiology Lab 1. 2. 3. If the H+ concentration of a blood sample is 40 × 10−9 Eq/L, what is the pH of the blood? A weak acid, HA, dissociates in solution into H+ and the conjugate base, A−. If the pK of this weak acid is 4.5, will the concentration of HA or A− be higher at a pH of 7.4? How much higher will it be? For the three sets of information shown in Table 4–3, calculate the missing values. 4. A man with chronic obstructive pulmonary disease is hypoventilating. The hypoventilation caused him to retain CO2 and to increase his arterial Pco2 to 70 mm Hg (much higher than the normal value of 40 mm Hg). If his arterial HCO3- concentration is normal (24 mEq/L), what is his arterial pH? Is this value compatible with life? What value of arterial HCO3- would make his arterial pH 7.4? 5. Figure below shows a titration curve for a hypothetical buffer, a weak acid. What is the approximate pK of this buffer? At a pH of 7.4, which is the predominant form of the buffer, HA or A−? Mr. Tony is a 66-year-old long-distance truck driver. Ten years ago, he was diagnosed with focal segmental glomerulosclerosis (a glomerular disease that causes nephrotic syndrome). Because he is constantly on the road, Roger found it difficult to have periodic check-ups. Recently, however, his symptoms were alarming—he had gained weight, his face and legs were swollen, and his pants no longer buttoned around the waist. Since these are signs that his physician had warned him about, he called in sick and made an appointment for a check-up. On physical examination, the physician noted periorbital edema, pitting edema of his extremities, ascites, and an S3 gallop. Plasma and 24-hr urine values are shown in Table below The physician ordered a strict low-Na+ diet and prescribed a loop diuretic, furosemide. After a few days, Roger called in to report that the furosemide wasn’t working—“nothing’s happening, doc.” The physician increased the dosage of furosemide and prescribed a second diuretic, spironolactone, to be taken at the same time. 1. As a consequence of long-standing focal segmental glomerulosclerosis, Roger developed nephrotic syndrome, a clinical complex characterized, first and foremost, by proteinuria. Why was Roger excreting large amounts of protein in his urine? 2. Why did Roger have hypoalbuminemia, and what is the expected effect on plasma oncotic pressure? 3. What mechanism can you propose for his hyperlipidemia? For his lipiduria? 4. Roger had generalized edema, caused in part by his hypoalbuminemia. How does hypoalbuminemia lead to generalized edema? 5. An additional cause of Roger’s edema was retention of Na+ and water by his kidneys. Propose a mechanism for increased Na+ and water reabsorption in nephrotic syndrome and explain how this increase would contribute to edema. 6. What is the meaning of his S3 gallop? 6. The presence of generalized edema is associated with increased total body Na+ content. If Roger’s total body Na+ content was increased, why did he have a normal plasma Na+ concentration? 8. Why did Roger’s physician place him on a low Na+ diet? 9. Roger needed to receive a diuretic in order to increase his Na+ and water excretion. Why was the initial dosage of furosemide ineffective? What was the rationale for increasing the dosage? 10. Why was spironolactone added to his treatment?