here
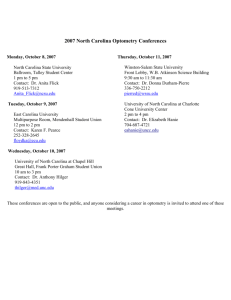
advertisement

Working Together to Improve Birth Outcomes in North Carolina Region IV and Region VI Infant Mortality Summit January 12-13, 2012 New Orleans Belinda Pettiford, MPH NC Division of Public Health, Women’s Health Branch Sarah Verbiest, DrPH, MSW, MPH University of NC at Chapel Hill, Center for Maternal and Infant Health Thanks to our amazing partners! Women, men, and families! NC Child Fatality Task Force Division of Medical Assistance (Medicaid) UNC Center for Maternal and Infant Health NC Community Health Center Association NC Healthy Start Foundation Community Care of North Carolina Perinatal Quality Collaborative of NC NC Chapter of March of Dimes Division of Mental Health, Dev. Disabilities, and Substance Abuse Svs. NC Medical, Pediatric, and NC OB/GYN Societies NC Academy of Family Practice Local health departments, local CCNC networks, and other providers Numerous universities, colleges, faith entities, and CBOs And the Division of Public Health (home of Title V and OMHHD) and many more! Every day, two babies die in North Carolina A society's infant mortality rate is considered an important indicator of its health, because infant mortality is associated with socioeconomic status, access to health care, and the health status of women of childbearing age. (Congressional Budget Office, 1992) Leading Causes of Infant Mortality Low Birth weight Prematurity Perinatal Conditions Related to Maternal Health Birth Defects Sudden Infant Death Syndrome (SIDS) About Two-Thirds of NC Child Deaths are Infants Infants 1 to 4 5 to 9 10 to 14 15 to 17 Deaths due to perinatal related conditions and birth defects are a major cause of death for children ages 1 to 9 years. 2008 child fatality data from State Center for Health Statistics Racial Distribution of North Carolina Live Births, 2010 There were 122,302 births in NC; 3.5% decrease from 2009. Approximately 24% of live births in North Carolina were to African Americans, 71% to Whites, and 5% to other races. While nearly 16% of NC live births are to women who report an Hispanic ethnicity, most of these Hispanic births are counted in the White racial category, according to NCHS vital statistics coding rules. Infant Mortality Rate North Carolina, 1988-2010 25 20 15 10 5 0 1988 1991 1994 1997 2000 Af. Am. 2003 White 2006 2009 Data Review o In 1988, NC’s overall IM rate was 12.5 per 1000 live births; the 2nd highest in the country. o The downward trend in the NC infant mortality rates has slowed since the mid-1990s, then fluctuated between 8.1 and 8.8 between 2000 and 2008. NC’s IM rate was at an all time low in 2010 (7.0 per 1000 live births); 44% reduction since 1988. o The largest decrease in 2010 was among non-Hispanic African American (19.6% reduction); NH White IMR declined 3.6%. o Racial disparities in IMR remain, with African American NH continuing to have an IMR more than two times (2.3) higher than White NH. Data Review The neonatal mortality rate (deaths occurring during the first 28 days of life) decreased 7.5% overall in 2010; there were substantial differences between whites and minorities. The White NH rate increased slightly (2.9%) while the African American NH rate decreased 14.0% (after showing a 13.8% increase the previous year). The Hispanic rate decreased 13.6% after showing a 4.8 percent increase the previous year. The post-neonatal mortality rate (28 days to one year) declined 19.2% overall in 2010, with White NH showing a decline of 10.5%, African American NH a decline of 30.8%, and Hispanics a decline of 15.4%. Birth Weight Data The percentage of infants delivered very low birthweight (less than 1500 grams) remained about the same in 2010 (1.7% in 2010 compared to 1.8% in 2009). However, NH African American women experience markedly higher rates of low and very low birthweight births (14.1%) than did NH White (7.8%) and Hispanics (6.3%). The percentage of babies that were delivered by Cesarean section decreased slightly to 31.4% -- down from 31.7% in 2009. Birth Weight Trends In 2010, more than one in ten (12.6 percent) of all resident births were premature (less than 37 weeks gestation). This is down slightly from 13.2% of all births in 2009. While the percentage of live births that are low birth weight has remained somewhat steady, the mortality rates in each birth weight category have decreased dramatically until recently. The greatest increase in low birthweight has been for babies born under 500 grams; steady for 2010 for a rate of 0.2%. Clinical / Quality Improvement Reducing Recurring PTB – 17P Initiative Increase appropriate utilization of 17P through a) education of public health leaders, clinicians, and women, b) addressing systems and access issues. Funded by DPH (via General Assembly) since 2006. Strong partnership with Medicaid and CCNC. www.mombaby.org – click 17P NC Community Health Centers NC has 27 federally qualified health centers 13 of 27 provide OB services Report to HRSA %LBW babies delivered and the trimester entered into prenatal care Majority pregnant women served are Hispanic women Recently received a special grant from HRSA to focus on tobacco cessation counseling NC Federally Qualified Health Centers Babies born (2005 – 2009) 7% born low birthweight 63% enter care in the first trimester High percent uninsured In 2010, the % of LBW babies born to Hispanic/Latina women was lower than the percent of LBW babies born to nonHispanic/Latina women (7% vs. 11%, respectively). Tobacco Cessation You Quit Two Quit Project – funded by former Health & Wellness Trust Fund (2008-2012) QI projects in 4 counties based in health departments Statewide educational and outreach efforts including NICUs New Project for Low SES Women of CBA funded by Fed Office of Women’s Health (2011-2013) Focused QI on 8 practices in one CCNC network Training and TA will be provided to all Chronic Disease and Pregnancy Care Managers within the CCLCF network Training opportunities will be made available to all practices within the network Hope to expand to a larger statewide QI program in the future www.YouQuitTwoQuit.com Patient Education Materials 18 www.MinuteToAsk.com Perinatal Quality Collaborative of NC (PQCNC) Mission: • Promote high value perinatal care • • • • Spread best evidenced practice and reduce variation Partner with families and patients Optimize resources Make North Carolina the best place to be born PQCNC Initiatives Hospital Based Initiatives: Eliminating elective deliveries under 39 Weeks gestation Reduce Catheter Associated Blood Stream Infections (CABSI) by 75% in participating centers Increase Exclusive Human Milk Mother - Baby Increase Exclusive Human Milk NICU Support for Intended Vaginal Birth (SIVB) Reducing Elective Deliveries <39 Weeks Decrease of 43% PQCNC Reduce CABSI Pregnancy Medical Home Improve birth outcomes in the North Carolina Medicaid population Provide evidence-based, high-quality maternity care to Medicaid patients Focus care management resources on those women at highest risk for poor birth outcome Improve stewardship of limited perinatal health resources In this program, quality improvement goals are aligned with cost savings goals – keeping more babies out of the NICU and avoiding associated expenses Methods Quality Improvement focus for Pregnancy Medical Home practices Identify outliers, work with them to improve performance Specific, required performance measures Support, training and resources Pregnancy Case Management is the key intervention Identify the population most at risk of poor birth outcome and focus resources on these women Pregnancy Medical Home Responsibilities Provide comprehensive, coordinated maternity care to pregnant Medicaid patients and allow chart audits for evaluation purposes for QI measures Postpartum visit must include: depression screening using a validated screening tool; addressing the patient’s reproductive life plan; and connecting the patient to ongoing care if it will not be provided in the PMH practice Provide information on how to obtain MPW, WIC, Family Planning Waiver Collaborate with public health OBCM to ensure high-risk patients receive care management Pregnancy Medical Home Responsibilities Eliminate elective deliveries (induction of labor and scheduled cesareans) before 39 weeks Maintain primary c-section rate at or below threshold level Primary C/S rate of 20% or lower Risk-adjusted (term, singleton,vertex) primary C/S rate of 16% or lower Offer and provide 17p to eligible patients Conduct standardized risk screening on all Medicaid patients Clinical integration with care management teams Priority Risk Factors focus on preterm birth prevention History of preterm birth (<37 weeks) History of low birth weight (<2500g) Chronic disease that might complicate the pregnancy Multifetal gestation Fetal complications (anomaly, IUGR) Tobacco use Substance abuse Unsafe living environment (housing, violence, abuse) Unanticipated hospital utilization (ED, L&D triage, hospital admission) Late entry to prenatal care/missing 2 or more prenatal appointments without rescheduling Provider request for care management assessment Benefits of being a Pregnancy Medical Home Support from CCNC network Data-driven approach to improving care and outcomes Incentives: Increased rate of reimbursement for global fee for vaginal deliveries to equal that of c-section global fee (similar increase for providers who do not bill global fee) $50 incentive payment for risk screening $150 incentive payment for postpartum visit No prior authorization required for OB ultrasounds What is CCNC? • Improves Health Outcomes & Reduces Care Costs: • • • • • • Manages care via population management strategies Supports the primary care medical home Care Management Services Community-based, provider-led Focuses on quality improvement Data driven CCNC Networks Programs & Campaigns Working with Communities to Reduce Disparities Healthy Beginnings 12 NC communities Primarily paraprofessionals provide outreach, care coordination and education with specific focus on breastfeeding promotion, folic acid, safe sleep, environmental tobacco reduction/elimination, healthy weight and reproductive life planning. Services provided to 900 women in 2010; with no infant deaths. Working with Communities to Reduce Disparities NC Healthy Start Programs Healthy Start Corps & Baby Love Plus 15 communities in our state Focus primarily within African American and American Indian communities. Include outreach, health education, case management, depression screening, interconception care, and community engagement. Most (80%) of the communities showed an improvement in birth outcomes among minority families in 2010. Community Health Ambassador (OMHHD) NC Maternal, Infant, and Early Childhood Home Visiting Program Goal: Coordinate an effective statewide planning and implementation system through a strong alliance with key partners in support of a continuum of home visiting services for families. North Carolina receives $3.2 million annually through the formula grant created by the Patient Protection and Affordable Care Act of 2010 (P.L. 111-148) to support evidence-based home visiting. North Carolina implementation: Supports four home visiting models: Nurse-Family Partnership Healthy Families America Parents as Teachers Early Head Start/Home Based Option Home Visiting cont. Seven sites at Local Health Departments & Community Based Organizations Partnership with the National Implementation Research Network and The Finance Project to support implementation and sustainability planning Current status: Implementation began on December 1, 2011 Oversight from the Governor’s Early Childhood Advisory Division of Public Health staff support sites in achieving fidelity to the model, learning continuous quality improvement and implementation science through training and technical assistance. Breastfeeding Promotion Breastfeeding Promotion NC Maternity Center Breastfeeding-Friendly Designation Expansion of Regional Training Center Infrastructure (6 centers that provide training and TA) Expansion of the Breastfeeding Peer Counselor Program (70 funded programs covering 86 Counties as of July 2011) Office of State Personnel Lactation Policy that covers all SPA employees with paid break time and space (the ACA only covers hourly workers) Child Care Regulation providing onsite space to mothers to pump or feed their infant (s) Trends in the percentage of infants ever breastfed and breastfed at least 6weeks, 6 & 12 months, NC WIC Program 1993-2010 Breastfeeding Challenges Poverty-in rural areas due to our unfortunate and uncomfortable history of slavery, breastfeeding is seen as a “poor” act and a reminder of the past since many slaves were wet nurses. PRAMS data shows that going back to work and school is a major barrier to continuation of breastfeeding. Race-there are assumptions by some providers that African American and American Indian women will not breastfeed so they may not “push” the issue. NC Infant Safe Sleep Campaign (formerly Back to Sleep) Established in 1994 Partnership with Division of Public Health (Title V) Adheres to American Academy of Pediatrics (AAP) Standards Administered by NC Healthy Start Foundation Uses evidence-based research, epidemiology, principles of public health Incorporates social marketing strategies Nationally recognized for outreach and social marketing Child care, communities, media, etc. (providers and public) Safe Sleep History in NC 1994 NC’s Back to Sleep Campaign started 2005 2003 NC SIDS Law for Childcare: ITS-SIDS BESST begins to strengthen community outreach 2006-2007 2011 HOPES begins with Advisory Group & 5 hospitals New AAP SIDS/SleepRelated Infant Death Policy www.nchealthystart.org • www.mamasana.org North Carolina leads the way… Largest and most comprehensive Shaken Baby Syndrome Prevention program in the United States. 3 basic components: Hospital education of parents of newborns Community reinforcements Media campaign www.PURPLEcryingnc.info What is PURPLE? Hospital Implementation 86 Hospitals (over 5,000 staff) across the state are participating in implementation Primary Care Provider Participation (as of April 2010) 373 offices participating; 96 out of 100 counties Collaboration with Center for Child & Family Health, UNC Injury Prevention Research Ctr, and National Ctr for Shaken Baby Syndrome Preconception Health Coalition Initiated in Jan 2007 ‐ leadership team formed Initial focus areas: pregnancy intendedness and healthy weight. NC Preconception Health Strategic Plan released in November 2008. From June 2008 –July 2011: 4 workgroups meeting regularly to move from strategies to action. Preconception Health Coalition Over 150 people. Representatives from DPI, DHHS, local health departments, public and private universities, community based organizations, non-profit agencies and consumers. Restructuring coalition so that instead of workgroups, the larger coalition will meets more frequently; will use webinar and videoconference to engage new participants. Minutes from meetings and other pertinent info available at www.everywomannc.org Women’s Wellness Materials Reproductive Life Planning Postpartum Visit Project NC Preconception Health Campaign March of Dimes is home of Campaign Funded by state and federal contracts Works closely with State’s NC Preconception Health Coalition and state leadership Focuses on educating public and health care providers about the importance of being healthy prior to pregnancy Grew out of state’s successful folic acid campaign NC Preconception Health Campaign Current Campaign Topics Folic acid Reproductive life planning Healthy weight Tobacco cessation Healthy weight trainings Empowering providers in public and private clinics across the state to use BMI as tool to start discussions about weight with their patients Link between overweight/obesity and maternal and infant health outcomes Common barriers for providers & patients Evidence-based Eat Smart Move More strategies Offering new Healthy Habits for Life booklet in English & Spanish for providers to use with their patients, BMI/gestation wheels, posters, etc. Successes 10-year NTD reduction of 39%; 72% reduction in western NC More than 550 health care practices and thousands of providers trained over 5-year period Consumer education using peer education – 100-150 lay health educators trained each year who in turn reach 5,000-10,000 women each year Preconception Peer Education Reach college-age population with targeted health messages emphasizing preconception health and healthcare. Train college students as peer educators. Arm peer educators with materials, activities and exercises to train their peers in college and in the community at large. NC Participating Universities A & T State University Duke University East Carolina University Fayetteville State University Johnson C Smith University NC Central University NC State University Shaw University UNC-Chapel Hill UNC-Greensboro Winston Salem State University Adolescent Pregnancy Prevention NC’s 2010 teen pregnancy rate was lowest in state history – 49.7 per 1000 live births (15-19 years) Currently supports 29 sites in the state 10 additional PREP (Prepare for Success) sites Healthy Youth Act – NC law requires all NC public schools to offer abstinence-based, comprehensive sex education to 7th through 9th graders. Innovations Life Course Perspective Motivational Interviewing Community Transformation Grant (NEW) Tobacco free living Active living and healthy eating High impact evidence-based clinical and other preventive services Policy & Collaborations Family Planning Waiver North Carolina’s Be Smart Family Planning Waiver program is designed to reduce unintended pregnancies and improve the wellbeing of children and families in N.C. by extending eligibility for family planning services to eligible women ages 19 through 55 and men ages 19 through 60 who meet the eligibility requirements for participation. N.C. Medicaid Family Planning Waiver (FPW) Program Update Based on the 2010 federal health care reform legislation, States now have the option to provide family planning services through a Medicaid State Plan amendment without the formal process of routinely needing to seek Federal approval for a waiver The Division of Medical Assistance submitted a State Plan amendment (SPA) to Centers for Medicare and Medicaid services (CMS) on 8/18/11. CMS approved North Carolina’s request to extend the current FPW through 1/31/12 while processing North Carolina’s SPA application for Family Planning Services FPW recipients who are at or below the 185% of the federal poverty level will continue to receive services under the new option. N.C. Medicaid FPW Program Update (cont.) In addition to providing services currently covered under the waiver, the State is proposing screening and treatment for STIs, which will be covered for any or all of the six periodic visits allowed under the new SPA program. The State is proposing screening only for HIV, which will be covered for any or all of the six periodic visits allowed under the new SPA program. Under the SPA, there will no longer be restrictions for eligibility based age to receive family planning services. The SPA will provide an opportunity for North Carolina to further reduce the rate of unintended pregnancies and improve the well-being of children and families by continuing the services previously covered under the FPW. Advocate for Environmental and Policy Changes that Support Preconception Health Maternity Leave Checklist and Benefits List created for state employees - covers benefit and health tips for women prior to pregnancy, during each trimester and postpartum. Advocate for Environmental and Policy Changes that Support Preconception Health Healthy Babies Healthy Business, a free intranet- based tool from March of Dimes now posted on the state health plan website Promote BMI assessment and healthy weight guidance in the family planning and maternity clinics Promoting appropriate gestational weight gain through trainings and/or web materials for public and private providers Tobacco Cessation Policies Smoke-Free Hospitals and Campuses House Bill 2 – Smoke-Free Restaurants and Bars Quitline – Free NRT 5As Counseling requirement for MH clinics; strongly encouraged in Title X clinics Alliance for Health and Other Groups trying to protect tobacco use prevention dollars Child Fatality Task Force Charged with making and implementing recommendations for changes to laws, rules and policies to support the safe and healthy development of our children and to prevent child abuse, neglect and death. Purpose is to develop a communitywide approach to understand the causes of childhood deaths, and identify any gaps or deficiencies that may exist in the delivery of services to children and their families. Comprised of Appointed Members (including legislators) to the Task Force and wider Membership on its Three Committees: Unintended Death Intended Death Perinatal Health http://www.ncleg.net/DocumentSites/Committees/NCCFTF/Homepage/ Perinatal Health Committee Comprised of over 125 members from across the state. Studied many different issues over the years – some brought forward by the public, partners and legislators Introduces fiscal items as well as policy items. Currently focusing on two new areas: Health Inequities in Birth Outcomes Synchronizing / Systematizing core public health messages for pregnant and new parents and families PHC: Focus on Disparities in Birth Outcomes Increase collective knowledge and understanding of health inequities in birth outcomes and any evidence and best practices available to address those inequities across North Carolina. Increase connections among members of the PHC and others who have an interest in working together on this issue. Develop a response to this issue which could include study, policy, research, program or legislative items. ONGOING Birth Equity Council Follow up to PHC Series – Initial Funding via NIH U13 25+ member leadership team representing a variety of sectors including Commerce 60+ member Council Purpose: develop an actionable strategic plan to address disparities in birth outcomes…then fund and implement Council in process of deciding on focus and framework for this work. Strong interest in addressing underlying social determinants of health Will launch over 15 stakeholder forums across NC as part of this process Timeline for completion and funding – Fall 2013 Contribution to Regional Efforts Women’s Integrated Systems for Health (WISH) A systems-based, integrated approach to the design and delivery of women’s health services, policies and programs to include mental health and wellness Distance Education Resources (Free) Orientation webinar series – archived Foundation - 6 online, self-paced modules Academy – intensive online, instructor led New MCH library knowledge pathway • Go to www.EveryWomanSoutheast.org – Training Funded by U.S. Health Resources &Services Administration’s Maternal &Child Health Bureau What is Every Woman Southeast? A coalition of leaders in Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina and Tennessee to build multi-state, multi-layered partnerships to improve the health of women and infants in the Southeast. Objectives Operationalize the life course model. Promote health equity. Train leaders to facilitate connectivity between sectors, to think about populations, and to address social determinants of health. Leverage policy and advocacy opportunities. Build on social media and social capital. Re-engage business and faith communities. Focus on the “grass tips” approach. Accomplishments to date Conducted an online survey Recruited Regional and State Teams Held planning meeting on March 2, 2010. Produced a compendium of activities Launched blog, website and Facebook page Launched webinar series National Preconception Summit Partner Team conversations, idea generating, study Logic model and grant submissions – In Progress www.EveryWomanSoutheast.org Questions? Belinda Pettiford – 919-707-5699 or b e l i n d a . p e t t i fo r d @dh h s . n c . g o v http://whb.ncpublichealth.com/ Sarah Verbiest – 919.843.7865 or s a r a h v @ m e d . u n c . e du