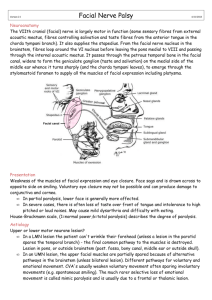
cranial nerve palsy
advertisement

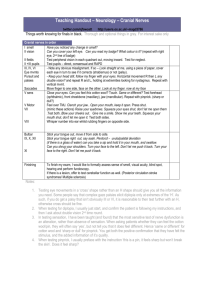
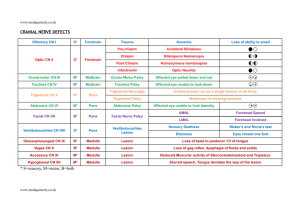
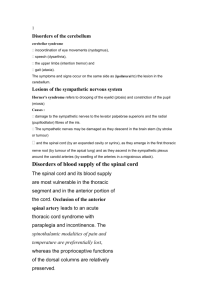
Cranial nerves: signs of disorder, examination. doc. MUDr. Valja Kellerová, DrSc. Department of Neurology Cranial nerves • provide motor and sensory innervation for the head and neck • damage of motor neurons results in cranial nerve palsy (central or peripheral?) • motor pathways for cranial nerves are composed of how many neurons? • where are they located? Cranial nerve palsy • The upper motor neuron – lesion results in an upper motor neuron weakness, central palsy • in: cortex, internal capsule, or brain stem above the nucleus • The lower motor neuron – lesion results in an lower motor neuron weaknesss, peripheral p. • in: the nucleus in the brain stem (the cell bodies form nuclei), or in any lower part of the cranial nerve Olfactory nerve disorders • hyposmia/anosmia: bilateral and transient – rhinitis • unilateral: – damage of the fila olfactoria – through cribriform plate of the ethmoid bone head trauma - skull fractures – olfactory bulb and tract damage – tumours – meningeoma, glioma • uncinate fits – olfactory hallucinations (unpleasant) lesion in the olfactory cortex (uncus gyri hippocampi) – tumour - glioblastoma Olfactory nerve examination • Testing the ability to smell or to identify different smells: – each nostril separately – the patient tries to identify the odor with eyes closed – recommended: perfume (flowers), spice (cinnamon, peppermint…), coffee, tobacco, soap… – avoid substances which irritate the trigeminal nerve (ammonia, vinegar…) Optic tract and manifestations of its damage • the ocular systém reverses the image • optic chiasma – partial decussation • damage anterior to the chiasma: – scotoma – monocular blindness • lesion at the chiasma: – heteronymous hemianopsia • damage posterior to the chiasma: – homonymous hemianopsia • lesion in the optic radiation: – quadrantanopsia • lesion to the visual cortex: – one side – homonymous hemianopsia – bilateral – cortical blindness Mumenthaler Optic nerve examination • visual acuity • optic fundus and disc: – papilloedema – prominence is measured in dioptres – in increased intracranial pressure (brain tumour?) – contraindication of lumbar punction! • visual fields – gross testing by confrontation Impaired ocular movement 1 • Disorders of gaze (supranuclear, central), or conjugate deviation of the eyes: – horizontal • the frontal lesion – tonic deviation of the eyes towards the lesion Lindsay Impaired ocular movement 2 • Disorders of gaze (supranuclear, central), or conjugate deviation of the eyes: – horizontal • the pontine lesion – tonic deviation away from the lesion Lindsay Impaired ocular movement 3 • Disorders of gaze – vertical • upward gaze and convergence are lost • in midbrain tectum lesion = Parinaud´s syndrome Netter Impaired ocular movement 4 Lesions of the cranial nerves (peripheral palsy): • III (oculomotor) • IV (trochlear) • VI (abducens) – with paralytic strabismus – with double vision (diplopia) Oculomotor palsy • ptosis (levator palpebrae m.) • divergent strabismus (the affected eye deviates laterally) • paralysis of the eye movements and accommodation • pupil dilatation (mydriasis), • reaction to light is absent Oculomotor palsy - paralysis of the eye movements (left eye) Oculomotor palsy (on the right side) • divergent strabismus • mydriasis • paralysis of the eye movements Perkin Trochlear palsy • rare • weakness of downward gaze • double vision when looking downwards • the head may tilt to the opposite side to minimise the diplopia • diplopia is vertical Right fourth nerve palsy, the paretic eye turns up- and outwards; head tilting Abducent palsy • convergent strabismus • failure of abduction on the affected eye (on looking to the paralysed side) • horizontal diplopia Left sixth nerve palsy (looking to the left) III, IV, VI cranial nerve examination • palpebral fissures (symmetrical? ptosis?) • position of the bulbs (parallel? strabismus convergent or divergent?) • ocular movements (full range? limitations?) • nystagmus (direction? degree?) • pupils: shape, size in mm (dilated – mydriasis, constricted – miosis) equality (isocoria? anisocoria?) reaction to light (light reflex): direct and consensual near reaction to accommodation and convergence Trigeminal nerve disorders • the fifth nerve: – sensory fibres subserve facial sensation (half of the face, 3 divisions) – motor fibres (in the mandibular division) innervate the muscles of mastication (masseter, pterygoids and temporalis) • disorders: – sensory loss – muscle weakness, atrophy (in peripheral palsy) – neuralgia Trigeminal nerve examination • pressure to points where the divisions emerge –painful • sensation (each division separately) for – pain – temperature – light touch • corneal reflex – blink response (trigemino-facial r.) – symmetrical? • masseter reflex (jaw jerk) • motor function of the masseter, temporal and pterygoid muscles Facial palsy • upper motor neuron lesion, central paralysis: the upper branch is less affected (because the rostral part of the nucleus is innervated bilaterally) paralysis is marked on the muscles in the lower half of the face, on the opposite side • lower motor neuron lesion, peripheral paralysis: paralysis of all facial muscles on the same side Mumenthaler Facial palsy Central Facial palsy Peripheral: • the upper branches – flattened wrinkles on the forehead – lagophthalmos an attempt to close the eyes the one eye does not close – Bell´s phenomenon the eyeball rotates upwards Facial palsy Peripheral: • the lower branches – flattening of nasolabial fold – mouth angle drop – asymmetrical: • smile • showing teeth • purse lips Facial nerve examination • observation • testing of the upper branches: – to wrinkle forehead (raise eyebrows) – to frown – to close eys tightly (persisting fissure in mm) • to close eyes against the resistance • testing of the lower branches: – – – – – to smile to show one´s teeth to purse the lips up to blow out the cheeks to whistle Primitive (prefrontal) reflexes Axial reflexes: • glabellar, nasopalpebral reflex - physiological, blink response (lowered/absent in peripheral facial palsy) Primitive (prefrontal) reflexes: • pout reflex - a pout response = protrusion of the lips (snout reflex or labial reflex) to tap • sucking reflex (to light touch) • grasp reflex (Janiševski´s reflex) – their presence in adults is pathological – suggests a lesion of the frontal lobe Vestibulocochlear nerve disorders • Auditory function - hearing loss • Vestibular function: – vertigo (an illusion of rotatory movement), vomiting… – nystagmus (a rhythmical oscillation of the eyes) • a slow drift in one direction, followed by a fast corrective movement • nystagmus direction – in terms of the fast phase • horizontal, vertical, rotatory, diagonal, mixed… • nystagmus: grade I, II, III – tonic deviations • towards the damaged side • in peripheral vestibular lesions – „harmonious“ vestibular sy • dependence on the head position Examination - tonic deviations • Hautant´s test – deviation of the arms - in angular degrees • Barány´s pointing test • (Unterberger gait test, stepping, marching test) • Romberg´s test • dependence of the fall direction on the head position • vestibular ataxia – gait with the eyes closed – deviation from the straight direction Disorders of the lower cranial nerves Lesions of the cranial nerves (peripheral palsy): • IX (glossopharyngeal) mixed • X (vagus) mixed • XI (accessory) motor – palatal weakness - bilateral – nasal quality of speech – pharyngeal weakness - bilateral – dysphagia – vocal cord paresis – hoarseness of the voice or dysphonia – the shoulder is dropped – the patient cannot turn the head to the healthy side IX, X, XI cranial nerve examination • swallowing difficulty? • assess the soft palate – at rest (symmetrical? palatal arch is drooped?) – during phonation (elevation?) • gag reflex (pharyngeal) – symmetrical? • accessory nerve (external branch): – sternomastoid muscle – trapezius muscle Lindsay Hypoglossal paralysis and examination • paralysis: – upper motor neuron paralysis • tongue deviates opposite to the lesion • mild weakness – lower motor neuron paralysis • tongue deviates to the side of the lesion • atrophy • fasciculation • examination: – inspection – mobility of the tongue Lindsay Bulbar and pseudobulbar palsy bulbar (nuclear) • bilateral affection of the lower cranial nerves IX-XII or their nuclei in the oblongata • lower motor neuron lesion, peripheral palsy • dysarthria, dysphagia, n.VII,V • masseter reflex absent • tongue atrophy, fasciculations • cause: polyradiculoneuritis Guillain-Barré syndrome), brainstem lesions – tumours, meningoencephalitis, motor neuron disease pseudobulbar (supranuclear) • bilateral lesion of corticobulbar tract • upper motor neuron lesion, central palsy • dysarthria, dysphagia, n.VII,V • masseter reflex increased • emotional lability (unprovoked crying or laughing) • frontal type of the gait • cause: cerebrovascular disease, arteriosclerosis (multi-infarct conditions)