The Obstetrical Client
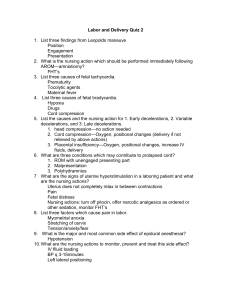
advertisement

Care of the Childbearing Family NCLEX Preparation Module 8 1 Maternal-Newborn Nursing in Registered Nursing Practice Registered Nurse, RN Registered Nurse Certified, RNC Clinical Nurse Specialist, CNS Nurse Practitioner, NP Certified Nurse Midwife, CNM 2 Legal Concepts in Maternal-Newborn Nursing Scope of Practice Standards of Nursing Care National Nursing Organizations Healthcare Agency Policies and Procedures 3 Ethical Issues in Maternal-Newborn Nursing Ethics versus Laws Common ethical issues Maternal-Fetal Conflict Abortion Intrauterine Fetal Surgery Reproductive Assistance Embryonic Stem Cell Research 4 Legal Issues in Maternal-Newborn Nursing Informed consent Confidentiality 5 Implications for Nursing Practice Advances in science and technology Provide information, not opinion Remain neutral Support patients even if you do not agree with their decisions 6 Concepts in Contemporary Childbirth Health care delivery settings Acute care, birthing centers Public health, school and college health Adolescent pregnancy centers Outpatient clinics, physician's offices Home care visits Complementary Alternative Medicine Homeopathic and herbal remedies Evidence-based practice 7 Maternal-Newborn Terminology Abortion Abruptio Placentae Amenorrhea Amniotomy APGAR Braxton-Hicks contractions Caput Succadeum Cephalhematoma Chadwick's sign Colostrum 8 Maternal-Newborn Terminology D.I.C. Dilation Effacement Endometriosis Endometritis Gestational age Gravida Hyperemesis Gravidarium Leukorrhea Leopold's Maneuvers Lightening Linea Nigra 9 Maternal-Newborn Terminology LMP and LNMP Lochia Mastitis “Morning Sickness” Parity Placenta Previa Pregnancy Induced Hypertension Premature rupture of membranes Primigravida Pyelonephritis 10 Maternal-Newborn Terminology Quickening Station Sexually Transmitted Infection Teratogenesis Threatened abortion Toxic Shock Syndrome 11 Maternal-Newborn Terminology (continued) T.O.R.C.H. Infections T= toxoplamosis O= other; gonorrhea, chlamydia, syphilis, varicella, hep B, Group B streptoccal, HIV; R= rubella C= cytomegalovirus H= herpes Urinary Tract Infection 12 Female Reproductive Cycle Ovarian Cycle - Follicular and luteal phases Endometrial Cycle - Menstrural, proliferative, secretory and ischemic phases Menstruation 13 Female Reproductive Anatomy External Genitals -Mons Pubis -Labia Majora - Clitoris - Uretral Meatus & Skene’s Glands - Vaginal Vetibule - Perineal Body Breasts Internal Reproductive Organs - Vagina - Uterus - Uterine Corpus - Cervix - Uterine Ligaments - Fallopian Tubes - Ovaries - Bony Pelvis - Bony Structure - Pelvic Floor 14 Organs of the Female Reproductive System Photo Source: National Assets Library, Health Education Assets Library, (HEAL), Royal University of Ireland, Public Domain, http://www.healcentral.org/healapp/showMetadata?metadataId=4912 15 Male Reproductive Anatomy External Genitals - Penis - Scrotum Internal Reproductive Organs - Testes - Epididymis - Vas Deferens - Ejaculatory Ducts - Urethra - Accessory Glands 16 Photo Source: U.S. National Cancer Institute's Surveillance, Epidemiology and End Results (SEER) Program, http://training.seer.cancer.gov/module_anatomy/unit12_2_repdt_male.html 17 Male Reproductive System Spermatogenesis Testosterone Testicular Self Exam (TSE) 18 Women’s Gynecologic Health Issues Gynecological Screening & Procedures Breast Self-Examination- “7 P”- position, pads, pressure, perimeter, pattern of search, practice with feedback, plan of action Mammography Pelvic Exam Pap Smear Sexually transmitted infection screening 19 Nurse's Role in Infertility Evaluation and Family Planning Role of the nurse Common Infertility Testing Comprehensive history and physical examination Sperm Count Basal body temperature chart Hormone evaluation 20 Nurse's Role in Infertility Evaluation and Family Planning Additional infertility procedures Ultrasound Hysterosalpingogram Endometrial biopsy Postcoital test Ovulation induction Therapeutic insemination Assisted reproductive technology 21 Nurse's Role in Family Planning Common Contraceptive Methods Nurse's role as an educator regarding common methods available to a woman and her partner Sterilization-tubal ligation and vasectomy Hormonal agents-implants, injections, oral, patches, vaginal ring, emergency contraception Intrauterine devise 22 Common Contraceptive Methods Condom- male and female Sponge Spermicides Diaphragm or Cervical Cap Natural Family Planning (Sympto-Thermal) Abstinence Breastfeeding Coitus Interruptus 23 Common Gynecologic and Urinary Health Problems Premenstrual Syndrome (PMS) Menopause and Hormone Replacement Therapy (HRT) Endometriosis Toxic Shock Syndrome (T.S.S.) Pelvic Inflammatory Disease (P.I.D.) Urinary Tract Infections (U.T.I.) Vaginitis and Vaginosis Breast and cervical cancer 24 Premenstrual Syndrome A clustering of signs and symptoms that occur only during the luteal phase in ovulatory cycles Severity can be mild to severe Many treatments are available to manage the symptoms Education and prevention 25 Menopause and Hormone Replacement Therapy Perimenopause may begin in mid thirties Hot flashes, insomnia, vaginal dryness Depression, mood swings, irritibility Osteoporosis Controversy regarding routine use of HRT Use for shortest period of time at lowest dose 26 Common Gynecologic and Urinary Health Problems Endometriosis Condition where endometrial tissue is found outside the uterine cavity Tissue responds to hormonal changes and bleeds resulting in inflammation, scarring and adhesions in pelvis and on peritoneum Many treatments are available to stop or slow the growth of the abnormal tissue 27 Common Gynecologic and Urinary Problems Toxic Shock Syndrome (TSS) Caused by Staphylococcus aureus May be related to tampon use and barrier contraceptives left in place more than 48 hrs. S&S – Early signs Fever > 38.9C or 102F Rash on trunk Hypotension, dizziness, vomiting, watery diarrhea Treatment – Hospitalization, IVs, Antibiotics 28 Common Gynecologic and Urinary Problems Pelvic Inflammatory Disease (PID) More common with multiple sexual partners Inflammatory disorders of upper female genital tract – endometritis, salpingitis, tubo-ovarian abscess, pelvic abscess, pelvic peritonitis Frequent organisms – chlamydia and gonorrhea Closely associated with infertility Treatment – IVs, pain medication, IV antibiotics, bedrest, antipyretics 29 Common Gynecological and Urinary Problems Urinary Tract Infections Pyelonephritis (Upper UTI) Often preceded by cystitis or bladder infection (lower UTI) More common in latter pregnancy or early post partum Frequency, urgency and dysuria seen with UTI May present with fever, chills, costovertebral angle (CVA) tenderness, flank pain, nausea and vomiting Treatment for cystitis is oral antibiotics Treatment for pyelonephritis is IV therapy for antibiotics and hydration, urinary analgesics, pain management and bed rest 30 Vaginitis and Vaginosis A common reason to seek gynecologic care May be asymptomatic or part of a woman's normal flora Common imbalance or normal flora in the vagina may include candida vaginitis, bacterial vaginosis, and Group B streptococcus Trichimonas, Human Papilloma Virus (HPV), Herpes Simplex type I and II (HSV), Hepatitis B and Syphillis Gonorrhea and Chlamydia Early diagnosis and treatment 31 Breast and Cervical Cancer Breast is leading cancer killer second only to lung cancer in women Annual well-woman evaluation can aid in early diagnosis of cancer PAP smear and preventive immunizations for cervical cancer are helpful Mammogram annually can aid in early detection which offers lower death rate and more treatment options which are less invasive 32 Nurse's Role with Intimate Partner Violence Approximately 1.5 million women are physically assaulted by an intimate partner annually in US. Does not stop because the women become pregnant. • 3 categories include: psychological, physical, and sexual abuse • Universal screening important at every health care encounter for symptoms of abuse 33 Nurse's Role with Intimate Partner Violence Awareness violence of signs and knowledge about the phases of Careful nursing assessment with standard questions while the victim is alone Knowledge of appropriate resources and health care personnel who can assist and follow up, provide legal advise and support 34 Signs of Intimate Partner Violence Signs of pain – grimacing, unsteady gait, complaints of abdominal pain Bruises especially of the arms, lacerations, burns, evidence of old fractures. Discrepancy between the explanation and the types of injuries Flattened affect, anxiety, depression, panic attacks, suicide attempts Late prenatal care, missed appointments 35 Intimate Partner Violence Cycles Tension Building Phase Battering Phase Honeymoon Phase 36 Questions Regarding Intimate Partner Violence Assessment should be part of all health encounters Have you been threatened, hit, slapped, kicked, choked or otherwise physically hurt by anyone within the last year? Has this happened since you have been pregnant? Within the last year, has anyone forced you to have sexual activities? Are you afraid of anyone? Be aware of resources for referral. 37 Conception, Fetal Development, Gestational Risk and Fetal Well-being Conception requires the maturation of gametes (sperm & ova) Ovulatory menstrual cycle includes preparation of uterine lining for implantation Patent female and male reproductive system allows passage of sperm and ova Fertilization of sperm & ova (zygote created) Implantation of ovum into secretory endometrium Hormonal support from the corpus luteum 38 Conception, Fetal Development, Gestational Risk and Fetal Well-being Stages of fetal development include: Pre-embryonic stage - First 14 days of human development starting at the time of fertilization Embryonic stage - Beginning of the third week through approximately 8 weeks Fetal stage - From 9 weeks until birth (at approximately 40 weeks after the last normal menstrual period). All major organs are formed by 8-12 weeks. 39 Conception, Fetal Development, Gestational Risk and Fetal Well-being Amniotic sac and fluid The fetal membranes consist of the amniotic and chorionic membranes that cover the fetal surface of the placenta which contains, protects and supports the fetus and the amniotic fluid. Amniotic fluid Cushions and protects the fetus Controls temperature Permits symmetrical growth of the embryo Prevents adhesion to the amniotic membranes Allows for freedom of movement 40 Conception, Fetal Development, Gestational Risk and Fetal Well-being Umbilical Cord Contains blood vessels (one large vein and two smaller arteries) Carries oxygen, waste products, and nutrients between the fetus and placenta Wharton’s Jelly - Helps prevent compression of the cord No nerves in the cord 41 Conception, Fetal Development, Gestational Risk and Fetal Well-being Placenta provides for: Metabolic and nutrient exchange between the embryo/fetus and the mother Fetal oxygen and carbon dioxide exchange Excretion of fetal waste products Hormones which support the pregnancy and are responsible for the metabolism of sugar 42 Conception, Fetal Development, Gestational Risk and Fetal Well-being Fetal heart and circulatory system make intrauterine life possible The ductus venosus empties directly into the fetal vena cava the right atrium and the left atrium via the foramen ovale left ventricle aorta. Blood returning from head and upper body via the superior vena cava empties into right atrium through tricuspid valve right ventricle pulmonary artery ( small amount to the lungs for nourishment) ductus arteriosus descending aorta placenta Fetal heart is under the control of it's own pacemaker. Decreased oxygen to the fetus evokes changes in the heart rate and blood pressure 43 Conception, Fetal Development, Gestational Risk and Fetal Well-being Factors affecting fetal well-being: Quality of sperm or ovum Intrauterine environment First trimester exposure to hazardous agents Maternal nutrition, hyperthermia, chronic diseases including diabetes, thyroid, cardiac, and circulatory Substance abuse Known or unknown infections 44 Fetal Circulation Photo Source: Little Hearts Matter, A registered charity in the UK, public domain, http://www.lhm.org.uk/patients/lhm/medical/general/circulation.asp 45 Barriers to Prenatal Care in U.S. Sociodemographics Insurance/finances Inadequate care providers for low income Child care Delay in onset of prenatal care Cultural factors Transportation Attitudes 46 Physical Changes During the Antepartum Period and Maternal Nutrition Signs of pregnancy Presumptive (generally subjective) Probable (objective) Positive (diagnostic) 47 Physical Changes During the Antepartum Period and Maternal Nutrition Expected Physical Changes - Cardiovascular Blood volume increase Physiological anemia Vital signs stable Increased clotting factors Edema 48 Physical Changes During the Antepartum Period and Maternal Nutrition Expected Physical Changes- Respiratory Oxygen consumption increases with decrease airway resistance Deeper respirations and upward pressure on diaphragm 49 Physical Changes During the Antepartum Period and Maternal Nutrition Expected Physical Changes - Gastrointestinal and Urinary Systems Nausea, vomiting, constipation, slowed peristalsis Bladder capacity increases and tone decreases; risk of UTIs increases 50 Physical Changes During the Antepartum Period and Maternal Nutrition Expected physical changes - Integumentary System Hyperpigmentation Linea Nigra Melasma 51 Physical Changes During the Antepartum Period and Maternal Nutrition Expected Physical Changes - Reproductive System Uterine enlargement 12 weeks – At Symphysis 16 weeks – Midway between symphysis and umbilicus 20 weeks – At the umbilicus 36 weeks - Near xyphoid process Photo Source: Wellcome Library London, Creative Commons, http://medphoto.wellcome.ac.uk/ 52 Determination of Estimated Day of Delivery (EDD) Nagele’s Rule Subtract 3 months from that date then add 7 days 1st day of LNMP (last normal menstrual period) Example: LNMP: September 10, 2006 Expected Due Date (EDD): June 17, 2007 53 Maternal Nutrition Nutritional Assessment Considerations Nutritional deficits present at the time of conception and during the early prenatal period Maternal age is important, especially in adolescent pregnancy Number of pregnancies and the interval between each pregnancy 54 Maternal Nutrition Maternal weight gain depends on BMI (Basal Metabolic Index) and pre pregnant nutritional state Weight Gain ranges: Underweight woman: 28 -40 lbs (12.5 -18kg.) Normal-weight woman: 25-35 lbs (11.5-16kg.) Overweight woman: 15-25 lb (7 - 11.5kg.) Obese woman: at least 15 lbs. (7.0 kg.) Gain of 3.5 lb (1.6 kg) during 1st trimester Gain of about 1 lb (0.4 kg) weekly rest of pregnancy 55 Maternal Nutritional Requirements The recommended daily allowance for calories - Increase 300 kcal/day during the second and third trimesters. Recent changes: • No extra daily calories in 1st trimester • 340 in 2nd trimester • 452 in 3rd trimester. 56 Maternal Nutritional Requirements Carbohydrates- source of energy and fiber Proteins-growth and repair of tissues Fats-essential fatty acids and vitamins Minerals-calcium, phosphorous, iodine, sodium, zinc, magnesium and iron Iron supplementation and education regarding high iron foods 57 Maternal Nutritional Requirements Fat soluble vitamins A (growth of epithelial cells in GI track) ,D (absorption and use of Calcium and Phosphorus),E (enzymatic and metabolic reactions) and K (synthesis of prothrombin) Water soluble vitamins C (development of connective and vascular tissue), B complex (cell respiration, glucose oxidation and energy metabolism) and folic acid 0.4 mg daily for, prevention of neural tube defects Fluids 58 Special Maternal Nutritional Issues Vegetarianism Lactose Intolerance Eating Disorders Anorexia Nervosa Bulemia Nervosa •Pica •Common GI Discomforts •Cultural, ethnic and religious influences •Psychosocial factors 59 Special Nutritional Considerations Nutrition for the pregnant adolescent Postpartum nutritional support Breastfeeding Non-nursing woman woman 60 Psychosocial Aspects of Pregnancy 1st trimester 2nd trimester 3rd trimester 61 Common Issues of Concern During the Childbearing Years Three major tasks of childbearing families Nurses need to assess the family unit Pregnancy and birth effects on the childbearing family 62 Fetal Diagnostic Tests Ultrasonography Fetoscope Alpha-Fetoprotein Screening Amniocentesis Nonstress test Vibroacoustic Stimulation Contraction Stress Test Biophysical Profile Maternal assessment of fetal movement “kick counts” Photo Source: Wikimedia Commons, U.S. Food & Drug Administration (Public Domain), http://commons.wikimedia.org/wiki/Image:Fetal-endoscope.gif 63 Potential Complications During Pregnancy During initial antepartal care, risk factors may be discovered or determined as labor progresses Risk factors include age, number of pregnancies, poor or excessive nutrition, cardiovascular or hypertensive disease Problems experienced during previous pregnancies, diabetes, drug abuse, infections and other factors may complicate pregnancy 64 Danger Signs in Pregnancy Assess and report immediately: Vaginal bleeding in any amount - May indicate placenta previa Premature rupture of membranes - Predisposes mom and baby to infection Edema of face or hands, abdominal pain, epigastric pain - Consider preeclampsia Severe, persistent headaches and visual disturbances Consider preeclampsia 65 Danger Signs in Pregnancy Report any of the following immediately: Fever and/or chills Painful urination Persistent nausea & vomiting Change in, or absence of fetal movement for 6-8 hrs. 66 Placenta Previa Placenta implants near or over the cervical opening (cervical os) Painless vaginal bleeding which may occur in the 3rd trimester Soft non tender uterus Vaginal exams are NEVER performed Birth by cesarean indicated if the placenta does not migrate up the uterine wall as gestation progresses 67 Nursing Management with Placenta Previa Assess the amount and character of bleeding Monitor Fetal Heart Tones (FHT) and activity monitoring (kick count) Bedrest and no sexual activity Report signs of preterm labor Conservative management of pregnancy 68 Abruptio Placenta Complete of partial premature separation of the placenta from uterus Precipitating Factors Blunt trauma to abdomen Drug abuse, especially cocaine Hypertension Premature rupture of membrane Smoking 69 Abruptio Placenta (continued) Medical emergency because of the risk of maternal hemorrhage and fetal demise May develop Disseminated Intravascular Coagulation (DIC) Bleeding may be obvious or concealed Concealed bleeding may lead to uterine tenderness and abdominal pain Monitoring may reveal elevated uterine resting tone and a rising FHT 70 Nursing Management of Abruptio Placenta Assess amount and character of bleeding Assess abdominal/uterine tenderness, contractions and resting Monitor for shock Assess FHT and activity Measure fundal height since concealed bleeding may be present Provide emotional support Prepare for possible C-Section 71 Ectopic Pregnancy Any gestation outside the uterus Most frequently in fallopian tube As the conceptus grows it causes distention, then possible rupture of site which usually occurs within 12 weeks gestation Any condition that diminishes tubal patency may predispose a woman to an ectopic pregnancy 72 Assessment of a patient with an Ectopic Pregnancy History of missed periods and symptoms of early pregnancy Abdominal pain, may be localized to one side Rigid, tender abdomen; sometimes abnormal pelvic mass Bleeding if present may be severe and lead to shock Low hemoglobin, hematocrit, rising white blood count (WBC) Human chorionic gonadotropin (hCG) usually lower than in intrauterine pregnancy 73 Nursing Interventions with Ectopic Pregnancy Prepare patient for surgery. Institute measures to control bleeding/treat shock if hemorrhage severe and continue to monitor postoperatively May be given methotrexate instead of surgery Allow patient to express feelings about loss of pregnancy and concerns about future pregnancies. 74 Patient with Abortion Spontaneous Induced or elective Monitor blood loss Observe passage of tissue Emotional support 75 Disseminated Intravascular Coagulation Complication sometimes seen in high risk pregnancies Pathologic clotting disorder Clotting factors, platelets and fibrinogen are used up inappropriately Widespread internal and external bleeding seen with inappropriate clotting in other locations Treatment with whole blood, packed RBCs and cryoprecipitate 76 Pregnancy Induced Hypertension Also known as preeclamsia and if progression occurs eclampsia Major cause of maternal and fetal death. Preeclampsia BP greater than 140/90 Proteinuria dipstick 1-2+ or greater than 3g/L in 24 hour specimen 77 Severe Preeclampsia BP 160/110 or above Hyperreflexia Extensive edema including pulmonary edema Headache and visual disturbances Abdominal pain in the right upper quadant or epigastric area Nausea & vomiting Decreased urine output ↑ proteinuria (3-4+) 78 Severe Preeclampsia Maternal complication may include hemorrhage including cerebral, cardiac or other organ failure and pulmonary edema Severe maternal complications include DIC and/or HELLP Hemolysis Elevated Liver enzymes, Low Platelets Syndrome Fetal complication may include intrauterine growth restriction and fetal distress from hypoxia 79 Eclampsia Grand mal seizure hearlds eclampsia Temporary coma may follow May occur in pregnancy, L&D, or postpartum Deliver as soon as possible when stable 80 Eclampsia Pharmacologic Treatments Magnesium Sulfate (MgSO4) is used to control seizures Toxic effects Depressed reflexes Depressed respirations Oversedation Circulatory collapse Calcium Gluconate serves as an antidote to MgSO4 81 Nursing Management with Preeclampsia Frequent VS especially BP Assess deep tendon reflexes Assess Fetal Heart Rate (FHR) and observe for signs of labor Test urine for protein, I & O, Foley catheter Bedrest/position on side Have oral airway, O2, and suction available Decrease environmental stimuli Implement seizure precautions Magnesium Sulfate with close observation Calcium Gluconate prn Seizure precautions 82 Diabetes in Pregnancy Gestational Occurs only during pregnancy Can usually be managed by diet and exercise alone Pregestational Diabetic prior to conception Requires insulin adjustment as pregnancy progresses 83 Gestational Diabetes May cause Polyhydramnios (excessive amniotic fluid) Macrosomia (large fetus) or Intrauterine Growth Restriction (IUGR) Dystocia (difficult labor and delivery) Fetal anomalies - more common in pregestational diabetes Associated with increased incidence of preeclampsia, premature birth, stillbirth, neonatal hypoglycemia, respiratory distress syndrome, and jaundice. Diabetes in Pregnancy Risk Factors Family history of diabetes in first-degree relatives Poor obstetric history Previous macrosomic infant Previous newborn with congenital abnormalities High parity Nursing Considerations Monitor fetal well-being Monitoring to maintain glucose in normal range Frequent antepartum visits Educate patient on glucose monitoring, diet guidelines, and about the effects of high blood sugar on the mother and the fetus Measure urine for protein and ketones 85 Patient with Hyperemesis Gravidarum Persistent, uncontrollable vomiting, unknown cause lasting throughout pregnancy Requires medical attention because of risk of dehydration, fluid/electrolyte imbalance, ketosis and metabolic alkalosis May require hospitalization for IV hydration, nutritional supplements and prevention or correction of electrolyte imbalance Emotional support 86 Rh Incompatibility Rh negative mother Rh positive fetus Maternal antibodies from exposure to Rh positive blood cross placenta and destroy fetal RBCs Rh Immune Globulin (RhoGam) given to mother at 28 weeks gestation and within 72 hours of birth of Rh positive infant 87 Infections in Pregnancy “TORCH” infections place mother and fetus in jeopardy due to associated complications T = toxoplamosis O = other; gonorrhea, chlamydia, syphilis, varicella, hep B, Group B streptoccal, HIV R = rubella C = cytomegalovirus H = herpes 88 Infections in Pregnancy (continued) TORCH - Some related complications include: Congenital heart defects Physical fetal anomalies Intrauterine growth restriction Mental retardation Brain dysfunctions including encephalitis and hydrocephalus 89 Infections in Pregnancy (continued) Toxoplasmosis- a protozoan Avoid raw or undercooked meat Avoid contact with an infected cat or feces Resultant problems: Spontaneous abortion Hydrocephalus Blindness Deafness Mental retardation 90 Infections in Pregnancy (continued) Gonorrhea- a bacterium that may Cause endocervicitis Cross the placenta Cause spontaneous abortion Result in preterm delivery Premature Rupture of Membranes (PROM) Blindness which can be prevented with Erythromycin eye ointment given after birth 91 Infections in Pregnancy (continued) Syphilis- is a sexually transmitted spirochete that can Cause congenital syphilis Cross the placenta Cause spontaneous abortion Cause preterm labor, stillbirth Result in fetal demise Cause disorders of CNS, teeth and cornea 92 Infections in Pregnancy (continued) Chlamydia- a virus-like bacteria that is the Most common Sexually Transmitted Infection (STI) in the U.S. It can cause: Weakness of fetal membranes PROM Preterm labor Chorieamnionitis Fetal conjunctivitis Pneumonitis 93 Infections in Pregnancy (continued) Varicella (chicken pox) - An acute maternal infection during weeks 13-20 that is most damaging to newborn which can cause: Limp hypoplasia Cutaneous scars Chorioamnionitis Cataracts Microcephaly Intrauterine Growth Restriction (IUGR) 94 Infections in Pregnancy (continued) Hepititis B virus Many modes of transmission including semen, vaginal secretions, breast milk Readily crosses the placental barrier Prematurity, low birth weight, neonatal death Newborn fever, jaundice, liver enlargement Chronic maternal infection develops into newborn infection 90% of the time Infant receives immune globulin and vaccine at birth 95 Infections in Pregnancy (continued) Group B Streptococcus- gram positive bacterium Leading cause of life-threatening perinatal infection 10-30% of women asymptomatic carriers Maternal infections-intraabdominal abscesses, meningitis, fasciitis, sepsis Preterm labor, PROM Newborn sepsis, severe respiratory infection, apnea, shock, CNS infection 96 Infections in Pregnancy (continued) Human Immunodeficiency Virus (HIV) Retrovirus causes a breakdown in the immune system Perinatal infection transmitted at birth and through breast milk High levels of maternal circulating virus can lead to fetal transmission Fetal enlarged liver and spleen, adenopathy, failure to thrive (FTT), persistent thrush, severe cradle cap, Chronic bacterial infections, sepsis, septic arthritis Mother and newborn treated with Zidovudine 97 Infections in Pregnancy (continued) Rubella virus is transmitted by nasopharyngeal droplets and direct contact. Greatest risk first trimester but can cross the placenta Spontaneous Abortion (SAB) Microencephalopathy Congenital cataracts Congenital heart disease Deafness Intrauterine Growth Restriction (IUGR) Mental retardation 98 Infections in Pregnancy (continued) Cytomegalovirus is a member of the herpes group and eventually infects most humans Highest rate of infection ages 15-35 Primary maternal infection may lead to SAB Newborn jaundice, enlarged liver and spleen Chorioretinitis CNS abnormalities IUGR Hearing loss 99 Infections in Pregnancy (continued) Herpes virus is sexually transmitted and highly contagious Viral shedding with active lesions, before eruption and after healing; virus migrates to sensory ganglion Newborn transmission occurs during contact with lesions and after Rupture of Membrane (ROM) Primary maternal infection poses greatest risk to fetus Preterm labor, SAB, IUGR Neonate highly contagious – ISOLATE and observe for fever, poor suck reflex, jaundice, seizures, lesions. Treat with Antiviral therapy 100 Other Vaginal Infections-Newborn Considerations Trichomoniasis can lead to PROM and post partum Human Papilloma Virus- Condyloma Acuminatancan lead endometritis to epithelial tumors of the larynx Candidiasis vaginal “imbalances” can lead to thrush, feeding difficulties and be transmitted to the nipple 101 Substance Abuse Addiction to or continued use of illegal or prescribed substances or drugs Substance abuse during 1st trimester places fetus at greatest risk Risk increases with strength, amount, frequency and route of administration Alcohol abuse is the number one cause of preventable mental retardation in the U.S. Can lead to Fetal Alcohol Syndrome (FAS) 102 Substance Abuse (continued) Early prenatal care helpful to identify abuse early This may help to prevent further complications Women on heroin are placed on methadone to help protect fetus Infants may withdraw from substances depending on what was used and when 103 Premonitory Signs of Labor Lightening Braxton Hicks Contractions Cervical changes Increased vaginal secretions Bloody Show Sudden burst of energy Weight loss Rupture of Membranes (ROM) True versus False Labor 104 Labor Signs True Labor • Contractions regular • Back to abdomen discomfort • Cervical dilation & effacement • Increase in frequency, duration, and intensity False Labor • • • • Irregular contractions Abdominal discomfort No dilation or effacement Inconsistent frequency, duration, and intensity 105 Stages of Labor Processes and stages of labor and birth Nursing assessments during labor Nursing management during labor 106 Stages of Labor First Stage begins with the onset of true labor to complete cervical effacement and dilation Divided into 3 phases: Latent phase : 0-3 cm dilated Active phase: 4-7 cm dilated Transitional phase: 8-10 cm dilated Stages of Labor First Stage Latent Phase or sometimes called early labor Irregular, short contractions lasting 20 to 40 seconds Dilation of the cervix from 0 to 3 cm. Behavior: talkative, excited 108 Stages of Labor First Stage Active Phase Cervical dilation measures 4 to 7 cm Contractions are 5 to 8 minutes apart and last 45 to 60 seconds. Behavior: more focused, concerned 109 Stages of Labor First Stage Transition Phase Cervical dilation measures 8 to 10 cm Contractions are 1 to 3 minutes apart and 60 to 90 seconds. Behavior: feelings of losing control Feels urge to push. 110 Stages of Labor Second Stage - complete cervical dilation to delivery of the neonate Crowning Occurs when the fetal head is encircled by the external opening of the vagina Birth is imminent 111 Stages of Labor Second Stage Positional changes of the fetus take place. These are called Cardinal Movements. The head enters the inlet of the pelvis in a transverse position Descent - Occurs throughout labor as the fetus moves down into the pelvic inlet. 112 Stages of Labor Second Stage Positional changes of the fetus continue with Flexion – This occurs as the fetal head descends and meets resistance causing the fetal chin to flex downward onto the chest. Internal Rotation – The fetal head moves to an oblique position as it enters the midplane (the smallest diameter of the pelvis). The head rotates to an anterioposterior position to fit through the pelvic outlet. 113 Stages of Labor Second Stage Positional changes of the fetus continue with Extension – The head extends to pass under the symphysis pubis. Restitution – As the head is born, the neck untwists, turning the head to one side (restitution), and aligns with the position of the back in the birth canal. 114 Stages of Labor Second Stage Positional changes of the fetus continue with External Rotation – As the shoulders rotate to the anteroposterior position, the head turns farther to one side (external rotation). Expulsion – the anterior shoulder moves under the symphysis pubis and is born followed quickly by the rest of the body 115 Stages of Labor Third Stage Placenta Separation Signs: umbilical cord lengthening, gush of blood, and change in uterine shape. Placenta delivery Avoid pressure on an uncontracted uterus to avoid inversion of the uterus 116 Stages of Labor Fourth Stage Recovery - From delivery of the placenta, approximately 1 to 4 hours after birth. Focus - Stabilizing the mother and neonate and promoting maternal-neonatal bonding. 117 Pain Management in Labor Nonpharmacologic – Lamaze Pharmacologic Analgesics Anesthetics Epidural or Spinal Local 118 Fetal Monitoring Fetal Heart Rate (FHR) FHR Variability FHR Accelerations FHR Decelerations Variable Early Late 119 Fetal Distress Assessment Ominous FHR pattern Fetal acidosis Meconium-stained amniotic fluid Decrease or cessation of fetal movement Nurse's role in fetal distress 120 Causes of Fetal Distress Utero-placental insufficiency Congenital malformation Maternal complications such as diabetes, heart disease or preeclampsia Maternal hypotension Infections Prolonged labor Postmaturity Oxytocin infusion Vaginal bleeding 121 Key Nursing Interventions for Fetal Distress Monitor FHR, fetal activity and fetal heart variability Identify and correct the cause if possible Position patient on the side to enhance utero-placental blood flow Administer oxygen via face mask as ordered (usually 8 – 10 liters/minute) Increase nonadditive IV fluids 122 Key Nursing Interventions for Fetal Distress Discontinue Oxytocin infusion if in use Assist with AROM (artificial rupture of membranes) and placement of internal fetal electrode Notify MD immediately if no improvement Prepare for cesarean birth Preoperative education and informed consent Treatment depends on the underlying cause 123 Common Complications of Labor and Delivery Common Complications Prolapsed Umbilical Cord Premature Rupture of Membranes (PROM) Preterm Labor 124 Prolapsed Cord Key interventions Relieve pressure on cord Trendelberg or knee chest position Oxygen to increase maternal oxygen saturation Pressure on the presenting part Call for help, but do not leave mother Expedite delivery 125 Premature Rupture of Membrane (PROM) Spontaneous break in the amniotic sac before onset of regular contractions Mother at risk for chorioamnionitis, especially if the time between Rupture of Membranes (ROM) and birth is longer than 24 hours Risk of fetal infection, sepsis and perinatal mortality increase with prolonged ROM. Vaginal examinations or other invasive procedure increase risk of infection for mother and fetus. 126 PROM Signs of Infection Maternal fever Fetal tachycardia Foul-smelling vaginal discharge 127 PROM Detecting Amniotic Fluid Nitrazine Ferning: Place a smear of fluid on a slide and allow to dry. Check results. If fluid takes on a fernlike pattern, it is amniotic fluid. Speculum exam 128 PROM Treatment Depends on fetal age and risk of infection In a near-term pregnancy, induction within 12-24 hours of membrane rupture In a preterm pregnancy (28 -34 weeks), the woman is hospitalized and observed for signs of infection. If an infection is detected, labor is induced and an antibiotic is administered 129 PROM Nursing Interventions Explain all diagnostic tests Assist with examination and specimen collection Administer IV Fluids Observe for initiation of labor Offer emotional support Teach the patient with a history of PROM how to recognize it and to report it immediately 130 Signs of Preterm Labor Rhythmic uterine contraction producing cervical changes before fetal maturity Onset of labor 20 – 37 weeks gestation. Increases risk of neonatal morbidity or mortality from excessive maturational deficiencies. There is no known prevention except for treatment of conditions that might lead to preterm labor. 131 Treatment of Preterm Labor Used if tests show premature fetal lung development, cervical dilation is less than 4 cm, & there are no that contraindications to continuation of pregnancy. Bed rest, drug therapy (if indicated) with a tocolytic 132 Preterm Labor Pharmacotherapies Terbutaline (Brethine), a beta-adrenergic blocker, is the most commonly used tocolytic Side effects: maternal & fetal tachycardia, maternal pulmonary edema, tremors, hyperglycemia or chest pain, and hypoglycemia in the infant after birth Ritodrine (Yutopar) is less commonly used. 133 Preterm Labor Pharmacotherapies Magnesium Sulfate Acts as a smooth muscle relaxant and leads to decreased blood pressure Many side effects including flushing, nausea, vomiting and respiratory depression Depression of CNS and DTRs Should not be used in women with cardiac or renal impairment Excreted by the kidneys 134 Perterm Labor Pharmacotherapies Corticosteroids Help mature fetal lungs Betamethasone or dexamethasone Most effective if 24 hours has elapsed before delivery 135 Nursing Interventions with Preterm Labor Nursing Intervention in Premature labor Observe for signs of fetal or maternal distress Administer medications as ordered Monitor the status of contractions, and notify the physician if they occur more than 4 times per hour. 136 Nursing Interventions with Preterm Labor Nursing Intervention in Premature labor Encourage patient to lie on her side Bed rest encouraged but not proven effective Provide guidance about hospital stay, potential for delivery of premature infant and possible need for neonatal intensive care 137 Nursing Interventions with Preterm Labor Discharge teaching for home care: Avoid sex in any form Take medications on time Teach to recognize the signs of preterm labor and what to do 138 Induction and Augmentation of Labor When continuing the pregnancy may be harmful to the fetus induction with Oxytocin may be indicate Hypotonic labor may need augmentation Nursing responsibilities with Oxytocin administration include: Ensuring proper set up of intravenous lines Slowly increase Oxytocin dose (titrate) Observe for maternal or fetal problems 139 The Postpartum Period Uterus The fundus descends 1 cm/day and is not palpable after 10 postpartum days. The organs return to a pre-pregnant state. Urinary tract May become edematous and lose tone and sensation. Anesthesia may cause urine retention. Bladder retention may cause the fundus to rise above the umbilicus. 140 The Postpartum Period Immediate nursing interventions: Assess fundal height and tone. Assess lochia amount and character - Heavy clots or spurts of bleeding indicate uterine hemorrhage or cervical tear. Assess perineum for swelling, discoloration, and state of episiotomy (if performed). 141 The Postpartum Period Renal system Cardiovascular system Fluid & electrolytes Hematopoetic system Gastrointestinal system Musculoskeletal system 142 The Postpartum Period Continued nursing interventions: Monitor for infection and hemorrhage Manage pain Assess mother-infant bonding Assess emotional status Teach for discharge Administer Rh immune globulin (RhoGam) or rubella as indicated 143 Nursing Interventions after Cesarean Birth Pain relief via patient-controlled analgesia (PCA) or morphine sulfate into the epidural Early ambulation Foley out first 12-24 hours Incision care - “REEDA” (redness, ecchymoses, edema, drainage, approximation) Watch for and treat abdominal distention which is often gas 144 Postpartum Complications Postpartum Hemorrhage (PPH) Early PPH occurs during the first hour after birth due to uterine atony, lacerations and hematoma. Treat with fundal massage and medications to cause uterine contractions. Late PPH is 1-2 weeks due to retained placental fragments, subinvolution. Treat with D&C, and medications including antibiotics. 145 Postpartum Infections Endometritis – malodorous lochia, fever (100.6), chills, abdominal pain, uterine tenderness, tachycardia and subinvolution The infection may spread to cause peritonitis and septic pelvic thrombophlebitis Treat with IV antibiotics Emotional support 146 Postpartum Infections Mastitis - A breast infection occurring 1-2 weeks after childbirth Engorgement and blocked mild duct increases risk Fever, localized breast pain, redness,warmth and inflammation Breastfeeding should continue Antibiotics Nurse's role is to support, educate and refer 147 Postpartum Adjustments Nursing management of the new family Families in crisis and the role of the nurse Nursing management of families that have suffered a loss, or other unfavorable outcome Relinquishing a newborn (adoption) 148 Postpartum Complications Postpartum Depression (PPD) Assess the presence and severity in all post partum women Depression lasts at least 2 weeks Lack of interest, guilt instead of pleasure, but able to care for infant Psychotherapy, antidepressants 149 Postpartum Complications Postpartum psychosis Rare, bipolar history common Risk to self and/or newborn Unable to properly care for newborn Hospitalization necessary Antidepressants, antipsychotics 150 Nursing Assessment of the Normal Newborn Initial Assessment immediately following birth Need for resuscitation APGAR scoring Heart rate Respiratory effort Muscle tone Reflex response Color Cry – strong and lusty 151 Nursing Assessment of the Normal Newborn Initial assessment (continued) Newborn responses to birth Assessment and care of the newborn Check for congenital anomalies especially cardiovascular, pulmonary and neurologic If stable, place with parents for initial bonding and early breastfeeding 152 Nursing Assessment of the Normal Newborn Second physical assessment – within first 4 hours of life General appearance Measurements: weight, length, head & chest circumference Temperature (axillary not rectal) Respiration: Normal 30 – 60 (average 40s) Heart: Normal 120 – 160. Temporary murmur from open ductus arteriosus common. Brachial and femoral pulses strong and equal. Blood Pressure not routinely assessed 153 Nursing Assessment of the Normal Newborn Skin characteristics Acrocyanosis Mottling Harlequin Jaundice Erythema toxicum – “Newborn rash” Milia Skin turgor 154 Nursing Assessment of the Normal Newborn Skin Characteristics (continued) Vernix caseosa Ruddy color Cracked and peeling skin Lanugo Forceps or vacuum marks Birthmarks Café-au-lait 155 Nursing Assessment of the Normal Newborn General appearance of the head Cephalhematoma – bleeding between the periosteum and the cranial bone Caput succedaneum – localized edema from pressure Molding – movement of the cranial bones during birth Fontanels 156 Nursing Assessment of the Normal Newborn Face Symmetry Eyes Nose Mouth Ears 157 Nursing Assessment of the Normal Newborn Neck Chest Cardiac Peripheral vascular Abdomen 158 Nursing Assessment of the Normal Newborn Umbilical cord Examined for 2 arteries, 1 vein. Will dry up and detach in 10 to 14 days Cord Care: alcohol, soap & water 159 Nursing Assessment of the Normal Newborn Genitals Female may have thick white mucousy vaginal discharge Male evaluate for the position of the urinary meatus, scrotum, testicles 160 Nursing Assessment of the Normal Newborn Anus – verify patency Arms and hands- count fingers, evaluate palmar creases and position of the arms Legs and feet – count toes, legs of equal length and check for hip dislocation (hip click) Back – Spine straight, no spina bifida 161 Nursing Assessment of the Normal Newborn Neurologic Status Alertness Resting posture Cry Muscle tone and activity 162 Nursing Assessment -Normal Newborn Reflexes Tonic neck Grasp Moro Rooting Sucking Babinski Plantar 163 Nursing Assessment of the Normal Newborn Estimation of gestational age through physical assessment Physical maturity characteristics – skin, lanugo, plantar creases, breasts, ear/eye, genitals characteristics Neuromuscular characteristics: resting posture, arm recoil, popliteal angle, scarf sign, heel to ear and square window signs 164 Nursing Care of the Normal Newborn Identification Medications Vitamin K Erythromycin Thermoregulation Feedings 165 Nursing Care of the Normal Newborn Infant protection Parent teaching Positioning Cord care Circumcision Car seat safety Screening tests, immunizations and other procedures Assessing and supporting bonding 166 Newborn Complications Identifying complications Hyperbilirubinemia (Jaundice) Physiologic janudice Pathologic jaundice Jaundice associated with breastfeeding 167 Nursing Interventions with Newborn Complications Hyperbilirubinemia (Jaundice) Phototherapy Changes bilirubin to water soluble easily excretable form Eye patch covering Frequent feedings to encourage frequent stools Bonding Parent Teaching 168 Newborn Complications Preterm Birth Respiratory problems Thermoregulation Fluid and electrolytes with parenteral feedings Watch for and treat infection Skin care Pain management 169 Newborn Complications Complications of preterm birth Respiratory distress syndrome Bronchpulmonary dysplasia Retinopathy of prematurity Necrotizing enterocolitis Periventricular-intraventricular hemorrhage 170 Newborn Complications Postterm infants and postmaturity syndrome Large-for-Gestational-Age Infants Small-for-Gestational-Age Infants Hypoglycemia Sepsis Congenital Anomalies 171 Case Study This case addresses complications seen in labor and in the postpartum period. Read the case study over carefully. Answer the questions at the end of the case study using the information provided. You may work individually or in a small group. Come to class prepared to discuss the case and share your answers. 172 NCLEX-RN Questions There are 40 multiple choice questions on a wide range of childbearing family topics. Attempt to answer them in 45 minutes. Do not look at the answers at the end of the study guide. Write down questions that gave you trouble so that they can be discussed in class at the appropriate time. 173 Photo Acknowledgement: Unless noted otherwise, all photos and clip art contained in this module were obtained from the 2003 Microsoft Office Clip Art Gallery.