Dangerous Critters?
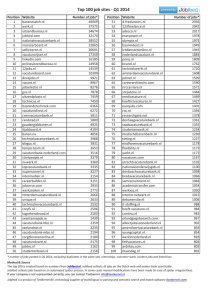
advertisement

Dangerous Critters? WY MSHA State Grant Program Gillette Campus of Sheridan College Western Wyoming Community College, Green River Center MICE? Are these “critters” REALLY dangerous? MOSQUITOES? SPIDERS? Dangerous Critters Venomous Spiders Mice & Rats Mosquitos Rice Rat Mosquito Hobo Spider (male) Hobo Spider (female) Yellow Sac spider Whitefooted mouse Black Widow Deer mouse Cotton Rat Brown Recluse DANGEROUSLY VENOMOUS SPIDERS DANGEROUSLY VENOMOUS SPIDERS Hobo Spider Widow Spider Recluse Spider Yellow Sac Spider Hobo/Brown Recluse Spider distribution Hobo Spider Male Female Pacific Northwest is normal range Enter homes July thru October Rarely found high on walls/ceilings Like mosquito bite, but turns into slow healing blister-like lesion – easily infected Female 8-11 mm, Male 11-16 mm Light to Med brown, 2 dark stripes on thorax, light strip on midline of abdomen broken by light chevron markings Hobo Spider poisoning Male venom may be more potent than female Subadults venom may be more potent than adults Red area immediately after bite Fades to “mosquitoe-like” bump Incorrectly referred to as an “aggressive” house spider…very fast spider…very poor eyesight Hobo Spider poisoning Within 24-48 hrs, blisters may occur Next 24 hrs, blisters may rupture, leaving open ulceration Next few days a scab forms, giving a “bulls-eye appearance Scab sloughs, leaving a scar in +/- 45 days Some instances, as with fatty tissue areas, lesions can become deep and extensive (2-3 yrs to heal) Hobo Spider poisoning Other long-term effects: Intractable burning pain… Damage to blood vessel valves… Cyst formation… Multiple lesions from gravitational drift… 15% of cases severe enough to require hospitalization In severe cases, bone marrow failure can develop, which causes death Black Widow Spider Female Throughout US Indoors year round, also outdoors Usually in seldom disturbed locations Web is approximately 12” in diameter Black color with red or orange hourglass marking on underside of abdomen (female only) Male 7-10mm, Female 12-13mm Black Widow Spider Bite Two tiny red dots, painful immediately Increased body temperature, sweating, nausea Some victims experience anxiety, profuse sweating, hair standing on end, increased blood pressure Black Widow Spider Bite No tissue necrosis Potent neurotoxin induces severe muscle cramping & spasms, beginning in large muscles of legs or abdomen Abdomen can exhibit board-like rigidity Severe cases include paralysis, stupor, and convulsions, death in small percentage of cases (small children, elderly) Brown Recluse Spider (Violin Spider) Midwest and southern US (may be some apparent reports in WY) Sticky webs under rocks, etc. Enter homes, cellars, barns Male & Female 6-12mm Tan to dark brown Fiddle shape markings on top of thorax Brown Recluse poisoning Day 2 Bite usually not felt, but produce immediate stinging like bee sting Tissue becomes swollen Flu-like symptoms Fever, nausea, chills, aches Brown Recluse poisoning Day 6 Painful ulceration develops Skin and musscle tissue dies, leaving a deep infected wound that enlarges, fails to heal or heals slowly (necrosis) Yellow Sac Spider Throughout US Indoors year round, mostly early autumn Build a silken sac in upper corners of ceilings Bite is slight burning sensation Some swelling Male 4-8mm, Female 5-10mm Pale yellow to green in color, legs and abdominal midline slightly darker Yellow Sac Spider bite Least known clinically significant spider Capable of causing a painful bite with necrotic lesion Not as severe as brown recluse or hobo Bites sometimes cause systemic effects Very prone to bite defensively (more than other significantly venomous spiders) Yellow Sac Spider bite Some bites in unusual areas (autos, swimming pools) Likely that many US cases of necrotic arachnidism ascribed to brown recluse are actually yellow sac spider bites HANTAVIRUS PULMONARY SYNDROME (HPS) HANTAVIRUS PULMONARY SYNDROME - SOME HISTORY First noted during an “outbreak” in the Four Corners area in May 1993 with several young & apparently otherwise healthy young people dying Researchers discovered a previously unknown type of hantavirus, carried primarily by the deer mouse Virus called Sin Nombre virus (SNV) and the disease it caused was named Hantavirus Pulmonary Syndrome (HPS) Further medical research revealed that HPS was not new and located the first case (through records and tissue analysis) in Utah in 1959 RODENTS KNOWN TO CARRY HANTAVIRUS PULMONARY SYNDROME Deer Mouse White-footed Mouse Rice Rat Cotton Rat Deer Mouse Head & body about 2-3 inches long-tail adds another 2-3 inches Gray to reddish brown Underbelly always white Tail has sharply defined white sides Found almost everywhere in North America Prefers woodlands, but found in desert areas also White-Footed Mouse Hard to distinguish from Deer Mouse Head & body about 4 inches-tail adds 2-4 inches Pale brown to reddish brown Underside and feet are white Found southern New England, Mid-Atlantic, southern, midwestern, western states & Mexico Prefers wooded & brushy areas Rice Rat Head & body 5-6 inches-plus a 5-7 inch tail Short, soft, grayish brown fur on top, gray or tawny underneath Feet are whitish Likes marshy areas and is semiaquatic Found in the southeastern US & Central America Cotton Rat Head & body 5-7 inches w/ tail 3-4 inches more Hair is longer and courser than deer mouse, grayish brown to grayish black Prefers overgrown areas w/ shrubs & tall grass Found in southeastern US, Central & South America SYMPTOMS OF HPS Early symptoms include: Fatigue, fever, muscle aches (especially large muscle groups – thighs, hips, back, shoulders) – universal symptoms May also have headaches, dizziness, chills, abdominal problems (nausea, vomiting, diarrhea, pain) – experienced by +/- ½ of victims Incubation time is unclear at this time Limited info indicates 1 to 5 weeks SYMPTOMS OF HPS Late symptoms include: Coughing, shortness of breath – universal symptoms Very uncommon symptoms: Earache, sore throat, and rash HANTAVIRUS PULMONARY SYNDROME Person to person contamination of HPS is unlikely Deer mice (cotton & rice rats-SE US, whitefooted mice-most of US) are the most common “carrier” of HPS Rodents “shed” the virus in their urine, droppings, and saliva Mainly transmitted to humans when we breathe air contaminated with the virus HANTAVIRUS PULMONARY SYNDROME Contamination happens when fresh rodent urine, droppings or nesting material is stirred up into the air we breathe – this process is called “aerosolization” Rodent bites are very rare mode of infection May be able to contract virus if you touch contaminated object, then touch your nose or mouth Suspected that you can be infected by eating food contaminated with rodent urine, droppings, or saliva HANTAVIRUS PULMONARY SYNDROME Disease transmission can happen any place rodents have infested such as: homes, barns, sheds, outbuildings, warehouses, summer homes, etc. Preventing rodents from infesting areas where you live and work is extremely important Disinfecting rodent-infested areas is very important to preventing the disease HOW TO PREVENT HPS Avoid contact with rodent infested areas Closed up rooms, cabins, warehouses Housecleaning activities in rodent infested areas Really stirring up the dust Large populations of rodents HOW TO PREVENT HPS Make your home, workplace, summer home or campsite unattractive to rodents If you don’t provide rodents with food and nesting material… You are much less likely to come into contact with them! HOW TO PREVENT HPS Recent research indicates that… Many people who became ill with HPS got the disease after frequent contact with rodents and/or their droppings around home or work Therefore…it makes sense to try to keep your home, vacation place, workplace, or campsite clean HOW TO PREVENT HPS Indoor Prevention Strategies… Keep your space clean… Keep tight lid on garbage… Set & keep spring loaded traps… Set EPA approved rodent bait… Use flea killer if bubonic plague is an area concern… Seal all entry holes ¼ inch and larger HOW TO PREVENT HPS Outdoor Prevention Strategies… Clear brush, grass, & junk from around buildings Use metal flashing around base of wooden, earthen, adobe (to 12” + above ground, 6” into ground) Elevate hay & woodpiles Trap rodents outside Encourage presence of natural preditors (snakes, owls, hawks, etc.) HOW TO PREVENT HPS Remember…getting rid of all rodents isn’t feasible…but with ongoing effort, you can keep populations very low… COMMON SIGNS OF RODENT INFESTATION You see rodent droppings… You see signs of rodent nesting… You find food containers that appear to be “nibbled” You find signs of “feeding stations” You find evidence of gnawing You notice an odd, stale smell You see a mouse in your area How to clean up infested areas Open buildings or closed areas and air them out before cleaning Wear personal protective equipment… Latex or nitrile gloves and P100 respirator Don’t stir up dust by sweeping or vacuuming Thoroughly wet contaminated areas…let stand 5 minutes Most general purpose disinfectants, household detergents are effective Hypochlorate solution (mix 1 ½ cups bleach in 1 gallon of water) may be used in place of commercial disinfectant How to clean up infested areas Once contaminated area is wet, take up contaminated materials with damp towel, then mop or sponge area with disinfectant Spray dead rodents with disinfectant…double bag with all cleaning materials and bury or burn Disinfect gloves before taking them off After taking off the gloves, thoroughly wash hands with soap and warm water WEST NILE VIRUS WEST NILE VIRUS No documented cases in Western Hemisphere until 1999 In 1999 & 2000 WNV encephalitis reported in New York City Metro area, New Jersey, and Connecticut – 83 cases, 9 deaths In 2001 WNV occurred in 10 states w/ 66 cases, 9 deaths In 2002 WNV spread to 44 states w/4,156 cases, 284 deaths Overview of West Nile Virus (WNV) WNV is a mosquito-borne disease that can cause encephalitis or meningitis Encephalitis is an inflammation of the brain tissue Meningitis is an inflammation of the membranes that envelop the brain or spinal cord WEST NILE VIRUS Transmitted to humans via mosquito bites Mosquitoes are infected by feeding on infected birds that have high level of WNV in their blood WNV is NOT transmitted from person to person No evidence that people get WNV from handling live or dead infected birds (use barriers as a precaution anyway) WEST NILE VIRUS Most WNV infected humans have no symptoms Small proportion develop mild symptoms including fever, headache, body aches, skin rash, swollen lymph glands – West Nile fever More serious infections include high fever, headache, neck stiffness, stupor, disorientation, coma, tremors, convulsions, paralysis – West Nile encephalitis WEST NILE VIRUS Less than 1% develop more severe symptoms including meningitis or encephalitis Estimated 1 in 1000 (0.1%) developing encephalitis die No specific treatment or vaccination WEST NILE VIRUS Prevention is your best course of action! Avoid mosquito bites-use “DEET” Clean out mosquitoes where you work and play WEST NILE VIRUS US Distribution (from USGS) West Nile was first isolated in 1937…known to cause infection and fever in humans in Africa, West Asia, and Middle East… Human Positive Avain (Bird) Deaths Negative WEST NILE VIRUS US Distribution (From CDC) WEST NILE VIRUS WY Distribution Avian (Bird) cases by county: WEST NILE VIRUS WY Distribution Animal cases by county WEST NILE VIRUS WY Distribution Human Cases By County: WEST NILE VIRUS Prevention When outdoors, wear clothing that covers the skin Apply effective insect repellent to clothing & exposed skin (DEET, etc.) Curb activity during dawn & dusk Apply screens to doors & windows & regularly maintain them Reduce the amount of standing water around home or work PLEASE REMEMBER! Safety and Health IS NOT just a “9 to 5” job! You should be safe AT HOME as well as AT WORK!