Luteal phase
advertisement

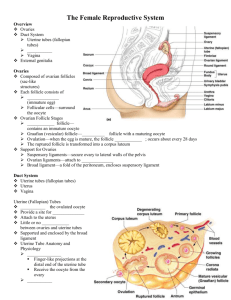
Female Reproductive System Suspensory ligament of ovary Peritoneum Uterosacral ligament Perimetrium Rectouterine pouch Rectum Posterior fornix Cervix Anterior fornix Vagina Anus Urogenital diaphragm Greater vestibular (Bartholin’s) gland Infundibulum Uterine tube Ovary Fimbriae Uterus Round ligament Vesicouterine pouch Urinary bladder Pubic symphysis Mons pubis Urethra Clitoris External urethral orifice Hymen Labium minus Labium majus Figure 27.10 Ovaries Held in place by several ligaments Ovarian ligament: anchors ovary medially to the uterus Suspensory ligament: anchors ovary laterally to the pelvic wall Mesovarium: suspends the ovary Broad ligament: supports the uterine tubes, uterus, and vagina; also contains the suspensory ligament and the mesovarium Suspensory ligament of ovary Ovarian blood vessels Uterine (fallopian) tube Mesosalpinx Mesovarium Broad ligament Mesometrium Ovarian ligament Body of uterus Ureter Uterine blood vessels Isthmus Uterosacral ligament Lateral cervical (cardinal) ligament Lateral fornix Cervix (a) Fundus of uterus Ovary Lumen (cavity) of uterus Uterine tube Ampulla Isthmus Infundibulum Fimbriae Round ligament of uterus Endometrium Wall of uterus Myometrium Perimetrium Internal os Cervical canal External os Vagina Figure 27.12a Ovaries Blood supply: ovarian arteries and the ovarian branch of the uterine artery Follicle Immature egg (oocyte) surrounded by Follicle cells (one cell layer thick) Several stages of development Primordial follicle: squamouslike follicle cells + oocyte Primary follicle: cuboidal or columnar follicle cells + oocyte Secondary follicle: two or more layers of granulosa cells + oocyte Late secondary follicle: contains fluid-filled space between granulosa cells; coalesces to form a central antrum Ovaries Vesicular (Graafian) follicle Fluid-filled antrum forms; follicle bulges from ovary surface Ovulation Ejection of the oocyte from the ripening follicle Corpus luteum develops from ruptured follicle after ovulation Tunica albuginea Degenerating corpus luteum (corpus albicans) Germinal epithelium Primary follicles Ovarian ligament Cortex Oocyte Granulosa cells Late secondary follicle Mesovarium and blood vessels Vesicular (Graafian) follicle Antrum Oocyte Zona pellucida Theca folliculi Ovulated oocyte Corpus luteum Corona Developing radiata corpus luteum (a) Diagrammatic view of an ovary sectioned to reveal the follicles in its interior Medulla Figure 27.11a Female Duct System Uterine (fallopian) tubes or oviducts Uterus Vagina Uterine Tubes Ampulla Distal expansion with infundibulum near ovary Usual site of fertilization Ciliated fibriae of infundibulum create currents to move oocyte into uterine tube Isthmus: constricted region where tube joins uterus Oocyte is carried along by peristalsis and ciliary action Suspensory ligament of ovary Ovarian blood vessels Uterine (fallopian) tube Mesosalpinx Mesovarium Broad ligament Mesometrium Ovarian ligament Body of uterus Ureter Uterine blood vessels Isthmus Uterosacral ligament Lateral cervical (cardinal) ligament Lateral fornix Cervix (a) Fundus of uterus Ovary Lumen (cavity) of uterus Uterine tube Ampulla Isthmus Infundibulum Fimbriae Round ligament of uterus Endometrium Wall of uterus Myometrium Perimetrium Internal os Cervical canal External os Vagina Figure 27.12a Uterus Body: major portion Fundus: rounded superior region Isthmus: narrowed inferior region Cervix: narrow neck, or outlet; projects into the vagina Cervical canal communicates with the Vagina via the external os Uterine body via the internal os Cervical glands secrete mucus that blocks sperm entry except during midcycle Uterine Wall Three layers 1. Perimetrium: serous layer (visceral peritoneum) 2. Myometrium: interlacing layers of smooth muscle 3. Endometrium: mucosal lining Endometrium Stratum functionalis (functional layer) Changes in response to ovarian hormone cycles Is shed during menstruation Spasms of spiral arteries leads to shedding of stratum functionalis Stratum basalis (basal layer) Forms new functionalis after menstruation Unresponsive to ovarian hormones Vagina Birth canal and organ of copulation Extends between the bladder and the rectum from the cervix to the exterior Urethra embedded in the anterior wall Vagina Layers of wall 1. Fibroelastic adventitia 2. Smooth muscle muscularis 3. Stratified squamous mucosa with rugae Mucosa near the vaginal orifice/opening forms an incomplete partition called the hymen Vaginal fornix: upper end of the vagina surrounding the cervix External Genitalia Mons pubis: fatty area overlying pubic symphysis Labia majora: hair-covered, fatty skin folds Labia minora: skin folds lying within labia majora Vestibule: recess between labia minora Greater vestibular glands Release mucus into the vestibule for lubrication Homologous to the bulbourethral glands External Genitalia Clitoris Erectile tissue hooded by a prepuce Glans clitoris: exposed portion Perineum Diamond-shaped region between the pubic arch and coccyx Bordered by the ischial tuberosities laterally Clitoris Labia minora Labia majora Inferior ramus of pubis Pubic symphysis Anus Body of clitoris, containing corpora cavernosa Clitoris (glans) Crus of clitoris Urethral orifice Vaginal orifice (b) Bulb of vestibule Fourchette Greater vestibular gland Figure 27.14b Mammary Glands Modified sweat glands consisting of 15–25 lobes Areola: pigmented skin surrounding the nipple Suspensory ligaments: attach the breast to underlying muscle Lobules within lobes contain glandular alveoli that produce milk Milk lactiferous ducts lactiferous sinuses open to the outside at the nipple First rib Skin (cut) Pectoralis major muscle Suspensory ligament Adipose tissue Lobe Areola Nipple Opening of lactiferous duct Lactiferous sinus (a) Lactiferous duct Lobule containing alveoli Hypodermis (superficial fascia) Intercostal muscles (b) Figure 27.15 Breast Cancer Usually arises from the epithelial cells of small ducts Risk factors include: Early onset of menstruation and late menopause No pregnancies or first pregnancy late in life Family history of breast cancer 10% are due to hereditary defects, including mutations to the genes BRCA1 and BRCA2 Breast Cancer: Detection and Treatment 70% of women with breast cancer have no known risk factors Early detection via self-examination and mammography Treatment depends upon the characteristics of the lesion: Radiation, chemotherapy, and surgery followed by irradiation and chemotherapy (a) Mammogram procedure Malignancy (b) Film of normal breast (c) Film of breast with tumor Figure 27.16 Oogenesis Production of female gametes Begins in the fetal period Oogonia (2n ovarian stem cells) multiply by mitosis and store nutrients Primary oocytes develop in primordial follicles Primary oocytes begin meiosis but stall in prophase I Oogenesis Each month after puberty, a few primary oocytes are activated One is selected each month to resume meiosis I Result is two haploid cells Secondary oocyte First polar body (benign…reabsorbed) The secondary oocyte arrests/stops in metaphase II and is ovulated If penetrated by sperm the second oocyte completes meiosis II, yielding Ovum (the functional gamete) Second polar body Follicle development in ovary Meiotic events Before birth Oogonium (stem cell) Follicle cells Oocyte Mitosis Primary oocyte Primordial follicle Primary oocyte (arrested in prophase I; present at birth) Primordial follicle Growth Infancy and childhood (ovary inactive) Each month from puberty to menopause Primary follicle Primary oocyte (still arrested in prophase I) Secondary follicle Spindle Meiosis I (completed by one primary oocyte each month in response to LH surge) First polar body Meiosis II of polar body (may or may not occur) Polar bodies (all polar bodies degenerate) Vesicular (Graafian) follicle Secondary oocyte (arrested in metaphase II) Ovulation Sperm Second Ovum polar body Meiosis II completed (only if sperm penetration occurs) Degenating Ovulated secondary oocyte In absence of fertilization, ruptured follicle becomes a corpus luteum and ultimately degenerates. corpus luteum Figure 27.17 Ovarian Cycle Monthly series of events associated with the maturation of an egg Two consecutive phases (in a 28-day cycle) Follicular phase: period of follicle growth (days 1–14) Ovulation occurs midcycle Luteal phase: period of corpus luteum activity (days 14– 28) Theca folliculi 3 2 4 1 5 6 8 7 Primary oocyte Zona pellucida Antrum Secondary oocyte Secondary oocyte Corona radiata 1 Primordial follicles Figure 27.18 (1 of 7) Theca folliculi 3 2 4 1 5 6 8 7 Primary oocyte Zona pellucida Antrum Secondary oocyte Secondary oocyte Corona radiata 2 Primary follicle Figure 27.18 (2 of 7) Theca folliculi 3 2 4 1 5 6 8 7 Primary oocyte Zona pellucida Antrum Secondary oocyte Secondary oocyte Corona radiata 3 Secondary follicle Figure 27.18 (3 of 7) Theca folliculi 3 2 4 1 5 6 8 7 Primary oocyte Zona pellucida Antrum Secondary oocyte Secondary oocyte Corona radiata 4 Late secondary follicle Figure 27.18 (4 of 7) Theca folliculi 3 2 4 1 5 6 8 7 Primary oocyte Zona pellucida Antrum Secondary oocyte Secondary oocyte Corona radiata 5 Mature vesicular follicle carries out meiosis I; ready to be ovulated Figure 27.18 (5 of 7) Theca folliculi 3 2 4 1 6 8 7 Primary oocyte Zona pellucida Antrum Secondary 5 oocyte 6 Follicle ruptures; secondary oocyte Secondary oocyte Corona radiata ovulated Figure 27.18 (6 of 7) Luteal Phase Ruptured follicle collapses Granulosa cells and internal thecal cells form corpus luteum Corpus luteum secretes progesterone and estrogen Luteal Phase If no pregnancy, the corpus luteum degenerates into a corpus albicans in 10 days If pregnancy occurs, corpus luteum produces hormones until the placenta takes over at about 3 months Theca folliculi 3 2 4 1 6 8 7 Primary oocyte Zona pellucida Antrum Secondary 5 oocyte 7 Corpus luteum (forms from Secondary oocyte ruptured follicle) Corona radiata Figure 27.18 (7 of 7) Establishing the Ovarian Cycle During childhood, ovaries grow and secrete small amounts of estrogens that inhibit the hypothalamic release of GnRH As puberty nears, GnRH is released; FSH and LH are released by the pituitary, and act on the ovaries These events continue until an adult cyclic pattern is achieved and menarche occurs During childhood, until puberty Ovaries secrete small amounts of estrogens Estrogen inhibits release of GnRH Establishing the Ovarian Cycle At puberty Leptin from adipose tissue decreases the estrogen inhibition GnRH, FSH, and LH are released In about four years, an adult cyclic pattern is achieved and menarche occurs Hormonal Interactions During a 28-Day Ovarian Cycle Day 1: GnRH release of FSH and LH FSH and LH growth of several follicles, and estrogen release estrogen levels Inhibit the release of FSH and LH Stimulate synthesis and storage of FSH and LH Enhance further estrogen output Hormonal Interactions During a 28-Day Ovarian Cycle Estrogen output by the vesicular follicle increases High estrogen levels have a positive feedback effect on the pituitary at midcycle Sudden LH surge at day 14 Hormonal Interactions During a 28-Day Ovarian Cycle Effects of LH surge Completion of meiosis I (secondary oocyte continues on to metaphase II) Triggers ovulation Transforms ruptured follicle into corpus luteum Hormonal Interactions During a 28-Day Ovarian Cycle Functions of corpus luteum Produces inhibin, progesterone, and estrogen These hormones inhibit FSH and LH release Declining LH and FSH ends luteal activity and inhibits follicle development Hormonal Interactions During a 28-Day Ovarian Cycle Days 26–28: corpus luteum degenerates and ovarian hormone levels drop sharply Ends the blockade of FSH and LH The cycle starts anew LH FSH (a) Fluctuation of gonadotropin levels: Fluctuating levels of pituitary gonadotropins (follicle-stimulating hormone and luteinizing hormone) in the blood regulate the events of the ovarian cycle. Figure 27.20a Primary Vesicular Corpus follicle follicle luteum Degenerating Secondary Ovulation corpus luteum follicle Follicular phase Ovulation (Day 14) Luteal phase (b) Ovarian cycle: Structural changes in the ovarian follicles during the ovarian cycle are correlated with (d) changes in the endometrium of the uterus during the uterine cycle. Figure 27.20b Uterine (Menstrual) Cycle Cyclic changes in endometrium in response to ovarian hormones Three phases 1. Days 1–5: menstrual phase 2. Days 6–14: proliferative (preovulatory) phase 3. Days 15–28: secretory (postovulatory) phase (constant 14- day length) Uterine Cycle Menstrual phase Ovarian hormones are at their lowest levels Gonadotropins are beginning to rise Stratum functionalis is shed and the menstrual flow occurs Uterine Cycle Proliferative phase Estrogen levels prompt generation of new functional layer and increased synthesis of progesterone receptors in endometrium Glands enlarge and spiral arteries increase in number Uterine Cycle Secretory phase Progesterone levels prompt Further development of endometrium Glandular secretion of glycogen Formation of the cervical mucus plug Estrogens Progesterone (c) Fluctuation of ovarian hormone levels: Fluctuating levels of ovarian hormones (estrogens and progesterone) cause the endometrial changes of the uterine cycle. The high estrogen levels are also responsible for the LH/FSH surge in (a). Figure 27.20c Endometrial glands Blood vessels Menstrual flow Functional layer Basal layer Days Menstrual phase Proliferative phase Secretory phase (d) The three phases of the uterine cycle: • Menstrual: Shedding of the functional layer of the endometrium. • Proliferative: Rebuilding of the functional layer of the endometrium. • Secretory: Begins immediately after ovulation. Enrichment of the blood supply and glandular secretion of nutrients prepare the endometrium to receive an embryo. Both the menstrual and proliferative phases occur before ovulation, and together they correspond to the follicular phase of the ovarian cycle. The secretory phase corresponds in time to the luteal phase of the ovarian cycle. Figure 27.20d Uterine Cycle If fertilization does not occur Corpus luteum degenerates Progesterone levels fall Spiral arteries kink and spasm Endometrial cells begin to die Spiral arteries constrict again, then relax and open wide Rush of blood fragments weakened capillary beds and the functional layer sloughs Menopause Has occurred when menses have ceased for an entire year There is no equivalent to menopause in males Menopause Declining estrogen levels Atrophy of reproductive organs and breasts Irritability and depression in some Hot flashes as skin blood vessels undergo intense vasodilation Gradual thinning of the skin and bone loss Increased total blood cholesterol levels and falling HDL Effects of Estrogens Promote oogenesis and follicle growth in the ovary Exert anabolic effects on the female reproductive tract Support the rapid but short-lived growth spurt at puberty Effects of Estrogens Induce secondary sex characteristics Growth of the breasts Increased deposit of subcutaneous fat (hips and breasts) Widening and lightening of the pelvis Effects of Estrogens Metabolic effects Maintain low total blood cholesterol and high HDL levels Facilitates calcium uptake Effects of Progesterone Progesterone works with estrogen to establish and regulate the uterine cycle Effects of placental progesterone during pregnancy Inhibits uterine motility Helps prepare the breasts for lactation Female Sexual Response Initiated by touch and psychological stimuli The clitoris, vaginal mucosa, and breasts engorge with blood Vestibular gland secretions lubricate the vestibule Orgasm is accompanied by muscle tension, increase in pulse rate and blood pressure, and rhythmic contractions of the uterus Female Sexual Response Females do not have a refractory period after orgasm and can experience multiple orgasms in a single sexual experience Orgasm is not essential for conception Sexually Transmitted Infections (STIs) Also called sexually transmitted diseases (STDs) or venereal diseases (VDs) The single most important cause of reproductive disorders Gonorrhea Bacterial infection of mucosae of reproductive and urinary tracts Spread by contact with genital, anal, and pharyngeal mucosae Gonorrhea Signs and symptoms Males Urethritis, painful urination, discharge of pus Females 20% display no signs or symptoms Abdominal discomfort, vaginal discharge, or abnormal uterine bleeding Can result in pelvic inflammatory disease and sterility Treatment: antibiotics, but resistant strains are becoming prevalent Syphilis Bacterial infection transmitted sexually or contracted congenitally Infected fetuses are stillborn or die shortly after birth Infection is asymptomatic for 2–3 weeks A painless chancre appears at the site of infection and disappears in a few weeks Syphilis If untreated, secondary signs appear several weeks later for 3–12 weeks, and then disappear: pink skin rash, fever, and joint pain The latent period may or may not progress to tertiary syphilis, characterized by gummas (lesions of the CNS, blood vessels, bones, and skin) Treatment: penicillin Chlamydia Most common bacterial STI in the United States Responsible for 25–50% of all diagnosed cases of pelvic inflammatory disease Symptoms: urethritis; penile and vaginal discharges; abdominal, rectal, or testicular pain; painful intercourse; irregular menses Can cause arthritis and urinary tract infections in men, and sterility in women Treatment: tetracycline Viral Infections Genital warts Caused by human papillomavirus (HPV) Second most common STI in the United States Increase the risk of cancers in infected body regions Viral Infections Genital herpes Caused by human herpes virus type 2 Characterized by latent periods and flare-ups Congenital herpes can cause malformations of a fetus Treatment: acyclovir and other antiviral drugs