THE PREGNANT UTERUS 1st & 2nd Trimesters
advertisement

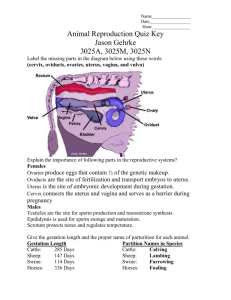
PREGNANCY: st nd 1 and 2 Trimesters (0 – 24 weeks) I. General A. Sonography used after 4-5 weeks B. Events prior to this time: 1. Ovulation 2. Fertilization 3. Implantation 4. Placentation 5. Embryonic Development II. OVULATION A. Definition: a cyclic event controlled by two hormones (FSH and LH) that occurs monthly 1. ~ 20 ova begin maturing 2. Only one completes the maturation process Phase?? 1st & 2nd Trimesters, Ovulation, con’t. 3. After ovulation, ovum moves into uterine tube 4. If fertilized, the zygote begins to divide 5. Implantation begins in ~6 days III. FERTILIZATION A. Definition: penetration of the ovum by one spermatozooan 1. Hyaluronidase (from acrosome): enzyme that allows penetration 2. Lack of acrosome/enzyme: infertility 3. Polyspermy: More than one sperm penetrates ovum 1st & 2nd Trimesters, Fertilization con’t. B. Sperm and ovum are haploid (N) C. Genetic material in nuclei fuses to form zygote (2N) D. Zygote begins cell division (mitosis!) immediately 1st & 2nd Trimesters, Fertilization con’t. E. Differentiation: prior to reaching uterus, zygote has developed into morula F. Cells continue to divide, form blastula or blastocyst 1. trophoblast 2. inner cell mass or blastoderm 1st & 2nd Trimesters, Fertilization, con’t. G. Trophoblast will give rise to placenta H. Inner cell mass will give rise to the embryo 1. Ectoderm (outer layer or “outer skin”) 2. Endoderm (inner layer or “inner skin”) 3. Mesoderm (middle layer or “middle skin”) Primary Germ Layers Trophoblast Cells Give rise to placenta Primary germ layers: Ecotderm Mesoderm Endoderm IV. Implantation A. Uterus composed of 3 layers 1. Perimetrium: external layer - peritoneum/broad ligament 2. Myometrium: middle layer 3. Endometrium: inner layer The Uterus Perimetrium Myometrium Endometrium 1st & 2nd Trimesters, Implantation, con’t. a. Epithelium forms numerous glands - may extend to myometrium b. Cyclic changes controlled by hormones - four phases c. If implantation occurs, endometrium is maintained in secretory phase Implantation Implantation begins ~ day 6 Trophoblast contacts endometrium Typically close to fallopian tube Trophoblast digests endometrium Enters “inner cell mass” first Completed by ~day 11 ** This concludes “period of the ovum” ** 1st & 2nd Trimesters, con’t. V. Placenta & Fetal Membranes A. Function of membranes: 1. house, protect, nourish 2. provide oxygen to 3. dispose of wastes for embryo 1st & 2nd Trimesters, con’t. B. Placenta 1. Decidua Capsularis: a. After implantation, embryo covered by endometrial layer b. Maternal tissue Placental formation Decidua capsularis Endometrial tissue Covers implanting embryo 1st & 2nd Trimesters, Placenta, con’t. 2. Decidua Basalis (Placentalis): a. Endometrial layer between embryo and myometrium b. Maternal tissue that will be meshed with fetal tissue Placental formation Decidua basalis Between embryo and mom Gives rise to maternal portion of placenta RNA virus DNA??? 1st & 2nd Trimesters, Placenta, con’t. 3. Trophoblast develops a second layer (chorion) during implantation a. Inner layer sprouts villi b. Villi penetrate decidua basalis c. Maternal blood seeps into spaces between villi d. Forms “Chorion Frondosum” Chorion Frondosum Chorion frondosum Chorionic villi Maternal blood 1st & 2nd Trimesters, Placenta, con’t. 4. Placenta has two origins: a. fetal portion: chorion frondosum b. maternal portion: decidua basalis 5. Blood in placental vessels: a. closely associated with maternal blood b. between chorionic villi Formation of Umbilical Vessels Placental vessels contain fetal blood Blood only communicates with mom’s blood via diffusion No direct mixing! 1st & 2nd Trimesters, con’t. C. Fetal structures 1. Amnion a. Inner fetal membrane b. Produces amniotic fluid c. Cushions embryo d. Contains enzymes for development Fetal membranes Amnion Outer fetal membrane Folds around embryo on all sides Forms amniotic fluid 1st & 2nd Trimesters, Fetal structures, con’t. 2. Yolk Sac a. Provides initial nourishment -connects to fetal gut b. develops from endoderm c. produces first blood cells d. forms part of primitive gut e. gives rise to allantois Fetal membranes Yolk Sac Formed from endoderm Minimal nourishment Provides umbilical vessels 1st & 2nd Trimesters, Fetal structures, con’t. 3. Umbilical Cord a. Point of fetal/maternal communication b. Formed from amnion, yolk sac, and body stalk c. Allantois: Contributes blood vessels to cord ** This concludes “period of embryo” (8 weeks) ** Umbilical Cord Vessels arise from yolk sac and forming placenta +O2 blood in umbilical veins - O2 blood in fetal veins +/- blood in fetal, umbilical arteries 1st & 2nd Trimesters, con’t. VI. Anomalies A. Meckel’s Diverticulum of the Ileum p. 137 1. Persistence of proximal end of yolk sac 2. Blind pouch a. usually <10 cm b. terminates at umbilicus c. occurs in 2% of population Meckel’s Diverticulum Meckel’s diverticulum of the Ileum May undergo torsion May form fistulas Sx mimic appendicitis 1st & 2nd Trimesters, Anomalies, con’t. B. Polyhydramnios 1. Volume of amniotic fluid > 2 liters 2. Associated with G.I. Tract obstruction or atresia 3. Causes: a. Diabetes Mellitus b. Viral infection in utero c. Rh incompatibility 1st & 2nd Trimesters, Anomalies, con’t. C. Oligohydramnios 1. Volume of amniotic fluid < 1/3 liter 2. May cause amniotic “band” syndrome 3. May be due to renal agenesis 1st & 2nd Trimesters, Anomalies, Oligohydramnios, con’t. 4. May indicate fetal demise, premature rupture of membranes 5. Causes: a. IUGR (Intrauterine Growth Restriction) b. Pulmonary Hypoplasia: lungs fail to develop properly 1st & 2nd Trimesters, con’t. A. Hydatidiform or Vesicular Mole 1. Occurs when embryo blights and chorion persists 2. Associated with Theca Lutein cysts in 1/3 of cases 3. Chorionic villi transform into vesicles 4. Benign tumor, may become huge (molar pregnancy) 1st & 2nd Trimesters, Anomalies, con’t. E. Omphalocele 1. Results when intestines fail to retract from umbilical cord 2. “Zipper” at linea alba fails to zip 3. External portion covered with skin of abdomen Omphalocele Associated with various trisomies and increased AFP levels Internal organs covered with peritoneum and amnion Normal till 10 weeks High fetal mortality rate 1st & 2nd Trimesters, Anomalies, con’t. F. Ectopic Pregnancy 1. Implantation of embryo outside uterus 2. Ampulla is most common site 3. May implant on mesentery, omentum, other sites 4. Rarely reach maturity Ectopic Pregnancy 99% are tubal pregnancies Other sites: Ovary Mesentery Cul-de-sac Spleen Liver 1st & 2nd Trimesters, Anomalies, con’t. G. Metastatic Carcinomas 1. Spread via lymph circulation a. Cervix: drains into internal and external nodes b. Body of uterus: drains into superficial inguinal nodes 1st & 2nd Trimesters, Anomalies, con’t. c. Fundus of uterus, fallopian tubes, and ovary: drain into para-aortic nodes at L-1 d. Vagina: drains into two directions 1st & 2nd Trimesters, Anomalies, con’t. 1. Lower 1/3 and vulva: drain into superficial inguinal nodes 2. Upper 2/3: drain to sacral, external & internal iliac nodes 2. Cancers may penetrate bladder or rectum wall 1st & 2nd Trimesters, Anomalies, con’t. H. Rectouterine Pouch (of Douglas) or cul-de-sac 1. Lowest point in abdominal cavity 2. Ectopic pregnancies, metastases often found here 1st & 2nd Trimesters, Anomalies, con’t. 2. Collects excess fluid in peritoneal cavity a. May be drained via posterior fornix b. Instruments may inadvertently penetrate 1. Enter peritoneal cavity 2. May cause peritonitis 1st & 2nd Trimesters, Anomalies, con’t. I. Hydrocephaly 1. Due to stenosis or blockage a. cerebral aqueduct b. foramina of Luschka or Magendie 2. CSF cannot circulate 3. Collects in and expands ventricles Hydrocephalus Means “water in the head” Usually due to a blockage in the CSF circulatory pattern May be corrected in utero 1st & 2nd Trimesters, Anomalies, Hydrocephalus, con’t. 4. Causes usually viral a. b. c. d. e. Toxoplasmosis (Valley Fever) Rubella (3-day measles) Treponema pallidum (syphilis) Herpes virus infection CMV infection (cytomegalovirus) 1st & 2nd Trimesters, con’t. Anomalies, continued … J. Anencephaly: 1. Lack of cerebral hemispheres 2. Brainstem is intact 3. Basic functions are present (breathing, heart beat) 1st & 2nd Trimesters, Anomalies, con’t. K. Porencephaly 1. Cysts or cavities in cerebral hemispheres 2. Cysts communicate with ventricles 1st & 2nd Trimesters, Anomalies, Porencephaly, con’t. 3. Hydranencepaly: a. an extreme form b. cerebral hemispheres nearly absent 4. Developmental anomaly, or ischemic infarction in utero Doppler U/S of the Circle of Willis in utero Circle of Willis Fetal circle of Willis: 3D U/S 1st & 2nd Trimesters, Anomalies, con’t. L. Spina Bifida 1. Defect of the spinal column 2. Due to failure of vertebral arches to close 3. Meninges, neural tissue exposed 4. May be associated with severe latex allergy Ultrasound-guided Prenatal Diagnosis Amniocentesis and CVS 1st & 2nd Trimesters, con’t. VII. First Trimester Bleeding A. Abortion (threatened or spontaneous) 1. Distorted irregular gestational sac 2. Common during first pregnancy a. Most women unaware b. Up to 50% may abort 1st & 2nd Trimesters, First trimester bleeds, con’t. B. Blighted ovum 1. embryonic membranes and chorion develop 2. no gestational sac C. Incomplete Abortion: embryo expelled, POC retained 1st & 2nd Trimesters, con’t. D. Molar gestation 1. Embryo blights 2. Chorionic villi become hydropic 3. Often accompanied by theca lutein cysts 1st & 2nd Trimesters, con’t. E. Ectopic pregnancy 1. Tubal implantation most common 2. Rupture results in bleeding F. Pelvic masses 1. Uterine leiomyoma (fibroid) 2. Corpus luteum cysts 1st & 2nd Trimesters, con’t. VIII. Uterine Anomalies: - usually result from fusion abnormalities of Mullerian ducts - embryonic tubular structures that give rise to fallopian tubes, uterus A. Arcuate uterus: saddle-shaped Uterine Anomalies 1st & 2nd Trimesters, Uterine anomalies, con’t. B. Capped uterus: muscle of fundus is contracted C. Couvelaire uterus: 1. blood in myometrium 2. indication of placental abruption D. Uterus acollis: uterus lacking a cervix 1st & 2nd Trimesters, Uterine anomalies, con’t. E. Uterus bicornis (duplex uterus, bifid uterus, uterus bifidis): uterus divided in two 1. Uterus bicornis unicollis: bifid uterus with one cervix 2. Uterus bicornis bicollis: bifid uterus with two cervices Uterine Anomalies, con’t… Uterine Anomalies, con’t… 1st & 2nd Trimesters, Uterine anomalies, con’t. F. Uterus biforis (uterus subseptus): 1. single uterine body 2. divided by short septum G. Uterus bilocularis (septate uterus, bipartite uterus, uterus septus): - uterus is divided by a complete anterior-to-posterior septum Uterine Anomalies, con’t… 1st & 2nd Trimesters, Uterine anomalies, con’t. H. Uterus didelphys: double uterus, each with own cervix I. Uterus incudiformis (uterus triangularis): uterus bicornis with broad, flat fundus J. Uterus parvicollis: normal uterus with abnormally small cervix K. Uterus unicornis: only one half of the uterus exists Uterine Anomalies, con’t… Uterus didelphys Uterus unicornis