- International Consortium for Evidence
advertisement

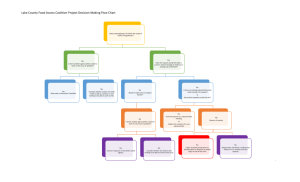
The International Consortium for Evidence-Based Perfusion: Moving from Concept to Reality Robert A. Baker1, 2, Timothy A Dickinson2, Donald S Likosky2, Kenneth G Shann2 1Flinders Medical Centre, Bedford Park, South Australia. 2Executive, International Consortium for Evidence Based Perfusion Potential Conflicts of Interest Research Support Terumo, National Heart Foundation, Somanetics, Lunar Innovations Travel and Conference Support Terumo, Medtronic, Cellplex, Bayer Perfusion Downunder Organisation Deputy Chair Chair of the PDU Collaboration Outline What is the ICEBP? Structure and Progress How and Why to get involved. What is the ICEBP? www.icebp.org Mission Statement The International Consortium for Evidence-Based Perfusion (ICEBP) partners and collaborates with perfusion societies, professional medical societies, and interested clinicians, to improve continuously the delivery of care and outcomes for our patients. Vision of the ICEBP To achieve this mission, we will • Evaluate current practice through a dedicated international perfusion registry. Mission Statement • Develop and publish evidence based guidelines, and support their integration The International Consortium for Evidence-Based Perfusion (ICEBP) partners and into clinical practice. collaborates with perfusion societies, professional medical societies, and interested clinicians, to improve continuously the delivery of care and outcomes for our patients. • Identify gaps in the medical literature and empower clinical teams to conduct Vision of the ICEBP research in areas where evidence is lacking. To achieve this mission, we will • Identify gaps between current and evidence-based clinical practice to promote •Evaluate current practice through a dedicated international perfusion registry. the improvement in patient care. •Develop and publish evidence based guidelines, and support their integration into clinical practice. •Identify gaps in the medical literature and empower clinical teams to conduct research in areas where evidence is lacking. International Consortium for Evidence-Based Perfusion Pediatric Process Improvement Subcommittee Clinically-Based Registry Subcommittee Communication Subcommittee Steering Committee Scientific Sessions Subcommittee Adult Process Improvement Subcommittee Evidence-Based Guideline Writing Subcommittee Educational Subcommittee Research Development Subcommittee Current practice Evidence-based practice Current practice Registry Guidelines Evidence-based practice Current practice CQI Registry Research Communications Education Scientific Sessions Evidence-based practice Guidelines Members Current practice Members CQI Registry Research Communications Education Guidelines Scientific Sessions Members Evidence-based practice Members Communications Subcommittee Website – www.icebp.org Website – Committee Pages Committee Sites Committee Sites Website – Meetings / Events Tools and Tips Newsletters www.icebp.org Scientific Sessions Planning Subcommittee Scientific Subcommittee Mission: Develop and organize an annual scientific meeting focused on meeting the goals of the ICEBP mission statement. The scientific meeting will cover topics related to all other subcommittees. In addition, the subcommittee will be charged with examining areas into which the meeting can grow to allow demonstration of sustained improvement in the care provided to patients. Scientific Subcommittee Mission: Develop and organize an annual scientific meeting focused on meeting the goals of the ICEBP mission statement. The scientific meeting will cover topics related to all other subcommittees. In addition, the subcommittee will be charged with examining areas into which the meeting can grow to allow demonstration of sustained improvement in the care provided to patients. Scientific Subcommittee Mission: Develop and organize an annual scientific meeting focused on meeting the goals of the ICEBP mission statement. The scientific meeting will cover topics related to all other subcommittees. In addition, the subcommittee will be charged with examining areas into which the meeting can grow to allow demonstration of sustained improvement in the care provided to patients. Scientific Subcommittee Mission: Develop and organize an annual scientific meeting focused on meeting the goals of the ICEBP mission statement. The scientific meeting will cover topics related to all other subcommittees. In addition, the subcommittee will be charged with examining areas into which the meeting can grow to allow demonstration of sustained improvement in the care provided to patients. Scientific Subcommittee Mission: Develop and organize an annual scientific meeting focused on meeting the goals of the ICEBP mission statement. The scientific meeting will cover topics related to all other subcommittees. In addition, the subcommittee will be charged with examining areas into which the meeting can grow to allow demonstration of sustained improvement in the care provided to patients. Best Practices in Perfusion Two Successful Meetings: 2006 Seattle, Washington (USA) 2007 Montreal, Quebec (CAN) Planning Committee - 2007 Dwayne Jones, CPC, CCP, RN (CAN) Christos Calaritis, BSc, CPC, CCP (CAN) Gordon R. DeFoe, CCP Timothy A. Dickinson, MS (Chair) (USA) Robert C. Groom, MS, CCP (USA) Deborah Hubble, CCP (USA) Donald S. Likosky, PhD (USA) Jeffrey B. Riley, MHPE, CCT (USA) Dirck A. Rilla, LP, CCP (USA) David J. Rosinski, CCP (USA) Kenneth G. Shann, CCP (USA) Alfred H. Stammers, MSA, CCP (USA) Robert Baker, PhD, CCP (Aus) Program Highlights - 2007 ICEBP guideline subcommittee update Quality improvement skills training The World Society for Pediatric and Congenital Heart Surgery –Dr. Tchervenkov Adult & pediatric registries Public reporting and transparency Credentialing of perfusionists as a best practice Abstracts on key aspects of best practice Audience Response System utilized International Attendees - 2007 Australia Pakistan Belgium Saudi Arabia Canada Spain Japan Sweden Germany United Kingdom Netherlands United States New Zealand Manufacturer Support - 2007 Bayer Pharmaceuticals Global Blood Resources The Medicines Company Luna Innovations Terumo Cardiovascular Medtronic, Inc. Maquet-Dynamed Inc. Quest Medical, Inc. Somanetics Corporations Rocky Mountain CAS Medical Systems Research Sorin Group Spectrum Medical Gish Biomedical, Inc. Best Practices – 2008 Date: Early October 2008 Location: Southern USA San Antonio Galverston Dallas Paediatric Subcommittee The Opportunity “The professions caring for patients with congenital heart disease have the unique opportunity to create the first comprehensive international database for a medical subspecialty.” Jacobs JP. International Congenital Heart Disease Nomenclature: Introduction to Mapping and Computer Based Mapping Solutions. Presented at The International Summit on Nomenclature for Congenital Heart Disease at The Third World Congress of Pediatric Cardiology and Cardiac Surgery, Toronto, Canada, May 27, 2001. Meaningful Multi-institutional Outcomes Analysis Requirements - Accomplishments Common Language = Nomenclature Mechanism of Data Collection (Database - Registry) Mechanism of Evaluating Case Complexity Mechanism to Verify Data Validity and Accuracy Collaboration Between Subspecialties Multi-Societal Database Committee for Pediatric and Congenital Heart Disease The STS Congenital Database Taskforce The EACTS/ECHSA Congenital Database Committee headed by Bohdan Maruszewski The STS Congenital Database Taskforce Core Users Group headed by Hal Walters The STS Congenital Database Data Verification Subcommittee headed by Dave Clarke The Aristotle Project headed by Francois Lacour Gayet The Multi-Center Panel of Experts for Cardiac Surgical Outcomes headed by Kathy Jenkins The Congenital Cardiac Anesthesia Society (CCAS) Database headed by David Vener The Joint Council of Congenital Heart Disease (JCCHD) headed by Gerard Martin, MD and representing the American Heart Association and the American College of Cardiology The Association of European Pediatric Cardiology Nomenclature Committee headed by Rodney Franklin Multi-Societal Database Committee for Pediatric and Congenital Heart Disease The Pediatric Cardiac Intensive Care Society (PCICS) The VPS (Virtual Pediatric Intensive Care Unit Database System) The International Consortium for Evidence Based Perfusion (ICEBP) The International Working Group for Mapping and Coding of Nomenclatures for Paediatric and Congenital Heart Disease (Nomenclature Working Group – NWG) headed by Christo Tchervenkov The World Society for Pediatric and Congenital Heart Disease headed by Christo Tchervenkov Center for Quality Improvement and Patient Safety of Agency for Healthcare Research and Quality (AHRQ) of the United States Department of Health and Human Services Birth Defect Branch of the Centers for Disease Control and Prevention (CDC) The National Association of Children's Hospitals and Related Institutions (NACHRI ) The National Quality Forum (NQF) Multi-Societal Database Committee for Pediatric and Congenital Heart Disease ICEBP Pediatric Committee is now a member Attend 3 meetings per year Involved with all projects Implementation of perfusion specific variables into STS Congenital heart surgery database Complications Project In congenital heart surgery, mortality in 2006 is 4%. In order to assess better quality of care involving the remaining 96% of patients, we must agree on universally accepted definitions of morbidity. Not all complications are caused by medical error and not all medical error results in complications. Not all complications are medical negligence or medical malpractice. Many subtypes of complications exist. Complications Project ICEBP Pediatric Committee responsible for CPB, ECLS, and VAD complication list Biweekly conference calls E-mail Multiple revisions Creation of manuscript to be submitted to Cardiology in the Young alongside other organ system complication lists (>1000) Ongoing Initiatives Collaborative Database initiatives with the: Congenital Cardiac Anesthesia Society (CCAS) Joint Council of Congenital Heart Disease (JCCHD), representing ACC and AHA Pediatric Cardiac Intensive Care Society (PCICS) STS Regional Congenital Database Reports Data Verification Site Visit Project Ongoing collaborative research to validate the Aristotle Basic Complexity Score with the developers of both the Aristotle Basic Complexity Score (ABC Score) and the Risk Adjustment for Congenital Heart Surgery (RACHS1) methodology with the goal of unifying these two systems. Complications Project Registry Subcommittee International Perfusion Registry Perfusion Fields in the STS Registry What Might Be Some Items on My Data Form? Traditional • Preoperative factors – Age, comorbid conditions • Intraoperative factors – Duration of cardiopulmonary bypass – Prime volume • Outcome Variables – Death x acuity, return to the OR for bleeding What Might Be Some Items on My Data Form? Traditional • Preoperative factors – Age, comorbid conditions • Intraoperative factors – Duration of cardiopulmonary bypass – Prime volume • Outcome Variables – Death x acuity, return to the OR for bleeding What you Can Vary • Process variables – Use of cell processing – Use and type of arterial line filter – Type of circuit – Prevention of air entrainment – Highest blood glucose level during bypass – Nadir Hct - by gender Guiding Principles Quality over quantity Definitions, definitions, definitions Validation of case count and status Smart registry Center Thumbprint Assist in submissions to other registries Software independent Cross match to STS and PDUCDB How We Can Learn from Each Other Lowest Hct on Pump Percent 30% 25% 20% Nov-06 Oct-06 Sep-06 Jul-06 Aug-06 Jun-06 May-06 Apr-06 Mar-06 Jan-06 Feb-06 Dec-05 Nov-05 15% Month -Yr OneOne center ’s experience center’s experience What is unique about these centers? TAKE HOME POINTS: The future depends on data collection, data feedback, and benchmarking Areas of Focus Patient demographics (to adjust for potential patient-level confounders) Compliance with perfusion guidelines that were published in JTCVS (amend the list as the ICEBP publishes guidelines) Cell processing and filtration Renal Management Factors influence low EF (among patients with normal EF) Guideline Writing Subcommittee The mission of the guideline writing subcommittee is to develop evidence-based clinical practice guidelines for cardiovascular perfusion. Methodology used by the American College of Cardiology/American Heart Association (ACC/AHA) Written and subsequently updated to remain concurrent with the medical literature. Adoption of these guidelines in practice would be tracked through the clinical registry subcommittee. Guideline Writing Subcommittee Guidelines Involvement of representatives from each of the participating perfusion organizations in the guideline writing subcommittee should reduce any un/anticipated hurdles for the endorsement of any given guideline. Submitted to the participating perfusion organizations for their review and endorsement Platelet Preservation: Do perfusion strategies really make a difference? Gordon R. DeFoe, BA, CCP Dartmouth-Hitchcock Medical Center Dartmouth Medical School Lebanon, NH, USA The Platelet Preservation Group Section Chairs Donny Likosky Kenny Shann Techniques Technology Monitoring Pharmacology Arno Nierich Kenny Shann Linda Shore Dirck Rilla Gordon DeFoe Jane Ottens Gordon DeFoe Tim Dickinson Arno Nierich Chris Mahoney Defining the problem Statement: We believe that platelets are good. Can we physically and qualitatively preserve platelets during cardiopulmonary bypass? Surface coatings or treatments Pump types Circuit components Cell salvage devices Are there holes in our knowledge? What are the steps? Evaluate the peer-reviewed medical literature in a rigorous and consistent fashion Focus expertise on specific topics Develop an informed opinion regarding effectiveness and assign levels of evidence Formulate a “finding” and a written summary for publication Search methodology NCBI - National Center For BioTechnology Information - MEDLINE search, ≥1996 Search parameters ((platelet OR platelets OR flow cytometry) AND (cardiac surgery OR ((("cardiopulmonary bypass"[TIAB] NOT Medline[SB]) OR "cardiopulmonary bypass"[MeSH Terms] OR ("coronary artery bypass"[TIAB] NOT Medline[SB]) OR "coronary artery bypass"[MeSH Terms]) OR (valve OR valves OR valvular) AND and surgery))) AND (biocompatible coated materials OR coated circuits) Evaluation of search results An automated Excel spreadsheet was automatically populated by NCBI search NCBI download includes abstract (if available) Reviewers can sift through references based upon abstract, or decide to review entire paper Almost all citations retrievable on-line Fate of all citations is tracked. Classification of Recommendations Class I - Conditions for which there is evidence, general agreement, or both that a given procedure or treatment is useful and effective Class II – Procedure or treatment should be performed or administered Class IIa – Additional studies with focused objectives are needed Class IIb – Additional studies with broad objectives are needed; additional registry data would be helpful Class III – Procedure or treatment should not be performed or administered because it is not helpful and might be harmful Levels of evidence Level A – Data is derived from multiple randomized clinical trials Level B – Data is derived from a single randomized trial or non-randomized studies Level C – Consensus opinion of experts Results of literature search 103 “hits” on MEDLINE All proved to be retrievable on-line 44 citations (inc. 2 review articles) were judged to be relevant to the topic of “technology for platelet preservation on bypass” In all, we evaluated studies on 4,234 adult patients in 41 distinct trials “Biocompatible” v “Standard” The clear preponderance of the evidence is that coated circuits better preserve platelet counts and reduce platelet deposition and activation, when used in either the “tip-totip” or “all but cannula” mode No clear benefit was observed when only the oxygenator was coated Comparison of technologies When different coatings were directly compared, there was no treatment that was clearly better than any other in terms of platelet preservation We did not find clear evidence that pump types or other component designs affected platelets directly Work still to be done Cochrane meta-analysis will be run Write discussion section for next publication There are holes in our knowledge Roller versus centrifugal Closed versus open Role of pump suction versus IRCR Is there a “best coating?” Proposed “Finding” When used in either the “tip to tip” or “all but cannula” configuration, biocompatible cardiopulmonary bypass circuits offer superior preservation and protection of platelets during and after cardiac surgery. (Class TBD, Level TBD) The Inflammatory Response: It’s not all about Pharmacological Intervention Rob Baker Flinders Medical Centre and Flinders University, Bedford Park Adelaide, AUSTRALIA Inflammation Section Chair: Clive and Rob Techniques Technology Pharmacology Richard*, Kimberle, David R, Joe S, Rob Bob G*, Andy C, Heinz, Nick M John M, Clive*, John M, Jeremiah, Hiliary G Cell Salvage Ischemia Temperature Embolism Ultrafiltration Pumps Coated Circuits Hemolysis Leukocyte Filtration * Sub group Leaders Do you think that cell salvage has an impact on inflammation in the Cardiac Surgical (on pump) patient? 82% 1. Yes 2. No 18% 3. Abstain ta in o A bs N Ye s 0% Cell Salvage Pubmed Searches 134 papers 4 + additional papers identified Emailed in Excel Format Abstract review identified 44 9 RCT’s I observational Recommendation Cell salvage is reasonable for the reduction of inflammatory markers in CS blood prior to its return to the patient. (Class TBD, Level TBD). Who is currently involved David Rosinski, Richard Newland, Kimberle McGill; Nicholas Mellas, Andrew Cleland, Bob Groom, Heinz Weitkemper, John Murkin, Jeremiah Brown, John Motley, Hiliary Grocott, Kenneth Shann, Tim Dickinson, Chris Brown Mahoney, Sander Spanjersberg, Arno Nierich, Donny Likosky, Linda Shore Brown, Gordon DeFoe, Dirck Rilla, Jane Ottens, Huong Pham, Rob Baker