Cervical Spine Pathologies and Special Tests
advertisement

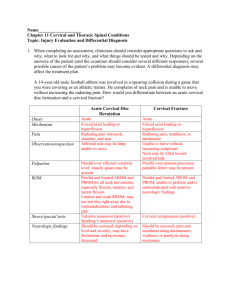
Cervical Spine Pathologies and Special Tests Orthopedic Assessment III – Head, Spine, and Trunk with Lab PET 5609C Pathologies Brachial Plexus Pathology: Brachial Plexus Neuropraxia: Common name: “Burner” or “Stinger” Definition: “Transient brachial plexopathy involving the upper trunk” “Temporary episode of unilateral upper extremity burning dysethesia with or without motor weakness” “Stinger” → tingling that occurs in upper extremity after injury Pathologies Brachial Plexus Pathology: Epidemiology: (specific studies) 50% of a Division I FB team had 1 or more burners/season (Robertson et al.) 65% of DIII FB players (201) during careers / 57% > 1 burner (Sallis et al.) 70% reported additional burners that they did NOT report ↑ occurrence with defensive players (DB’s) Pathologies Brachial Plexus: C5 – T1 7 cervical vertebrae 8 cervical nerves: 1st 7: exit above the corresponding vertebrae C8: exits below the 7th cervical vertebrae Pathologies Brachial Plexus Pathology: Mechanism of Injury: Stretch of the brachial plexus: Nerve root compression: Head forced laterally while opposite shoulder is depressed (common MOI – tackling) C5 and C6 (most commonly affected) Combination of neck hyperextension and ipsilateral lateral flexion Nerve roots impinged between vertebrae Spinal stenosis - ↑ risk Compression of brachial plexus: Direct blow to Erb’s point (shoulder pads compress plexus) Pathologies (A) Traction to the brachial plexus (ipsilateral shoulder depression and contralateral lateral neck flexion) (B) Direct blow to the supraclavicular fossa (Erb's point) (C) Compression of the cervical roots or brachial plexus (ipsilateral lateral flexion and hyperextension) Pathologies Pathologies Brachial Plexus Pathology: Signs and symptoms: Numbness and burning of the entire arm, hands, fingers Sensation loss over dermatomes Complete transient paralysis of affected nerves Tenderness over the brachial plexus Grading: Grade 1 (Neuropraxia): transient signs/sx. last from a few minutes → 2 weeks Grade 2 (Axonotmesis): significant sensory/motor deficits > 2 weeks and less than < 6 months Grade 3 (Neurotmesis): symptoms 6 months → 1 year Pathologies Brachial Plexus Pathology: Evaluation Inspection: Athlete shakes arm/hand in attempt to regain feeling Inspect cervical spine for abnormality (fracture/dislocation) Palpation: Cervical spine Clavicle, humerus, scapula, sternum, ribs SC, AC, GH joints Shoulder musculature Pathologies Brachial Plexus Pathology: Evaluation Functional Testing: Active and passive ROM (all neck and shoulder movements) RROM – can be performed in conjunction with myotome check Neurological Screening: Key muscles tested: deltoid, external rotators, biceps brachii Upper quarter sensory/motor testing Special Tests: Brachial plexus stretch test Cervical compression and distraction Spurling test Clinical Evaluation C1-C2 Neck flexion C3 Neck lateral flexion C4 Shoulder shrug C5 Shoulder abduction, ER C6 Elbow flexion, wrist extension C7 Elbow extension, wrist flexion C8 Thumb extension T1 Finger abduction and adduction Pathologies Brachial Plexus Pathology: Return to Play Criteria: Full, pain-free active and passive ROM in the cervical spine Full, pain-free neck strength against resistance Full strength of all shoulder and arm movements Normal sensation in all dermatomes Check shoulder pads/helmet to ensure proper fit Recheck in 3-5 minutes Protective Equipment: A: Neck Roll B: Lifter C: Cowboy Collar Pathologies Research Article #1: Effects of Football Collars on Cervical Hyperextension and Lateral Flexion Objective: Evaluate the effectiveness of 3 football collars in ↓ cervical ROM Why: MOI for stingers Do the collars ↓ movement? PREVENTION Pathologies Effects of FB Collars on Cervical Hyperextension and Lateral Flexion: Methods: Subjects: 15 D1 football players Force applied (hand-held dynamometer) Motion: 2-dimensional video analysis Movement: AROM and PROM Hyperextension Lateral flexion Hyperextension Findings: Lateral Flexion Findings: Can be limited by all 3 collars: (rankings) No collar ↓ passive lateral flexion better 1. Cowboy collar 2. A-Force 3. Neck roll than the shoulder pads alone Note: Passive overloading still resulted in additional 190 of hyperextension Standard neck roll ↓ active ROM Pathologies Research Article #2: Biomechanical Analysis of Football Neck Collars: Objective: Perform a biomechanical analysis of neck collars through dynamic testing Why: MOI for head and neck injuries Do the collars ↓ force transmission (upon impact)? Pathologies Biomechanical Analysis of FB Neck Collars: Methods: Collars (3) evaluated: Crash-test dummy: Cowboy collar (McDavid) Bullock collar Kerr collar Shoulder pads (raised and unraised), helmet, collar Accelerometers / load cells / angular rate sensors Impacts: Pneumatic linear impactor 5 m/s and 7 m/s Pathologies Biomechanical Analysis of FB Neck Collars: Results: Top of Head Impact: Front Impact: Most protection: Kerr collar (Bullock – 2nd) Why? Kerr collar contacts the base of the helmet during impact → redirects some load to shoulders Most protection: Kerr collar (all provided ↑ protection) ↓ head and neck movement ** Side Impact: Kerr – minimal protection Cowboy and Bullock – no protection Peak Values for Front Impact: Normal Shoulder Pad Configuration Pathologies Cervical Nerve Root Impingement: History: Onset: Acute of chronic Pain: Radiating symptoms into trapezius, scapula, shoulder, arm, wrist, and hand MOI: Compression or irritation of nerve Predisposing conditions: Disc pathology, narrowing of intervertebral foramina, facet degeneration Pathologies Cervical Nerve Root Impingement: Inspection: Palpation: Posture of head Point tenderness Functional Tests: Pain with extension, lateral bending toward same side, and rotation Neurological Tests: Upper quarter screen: AROM, PROM, RROM Muscle weakness, paresthesia, diminished reflexes Special Tests: Cervical compression test (↑ symptoms) Cervical distraction test (↓ symptoms) Spurling test / Vertebral artery test / Abduction test Special Tests Brachial Plexus Traction Test: Patient position: ATC position: Standing behind the patient Procedure: Seated One hand placed on side of the patient’s head; other hand over the AC joint (same side) Cervical spine is laterally bent and opposite shoulder depressed Positive test: Radiating pain on the side opposite the lateral bending Stretching of brachial plexus Radiating pain on the side toward the lateral bending Compression of cervical nerve roots between 2 vertebrae MOI is duplicated in attempt to replicate the athlete’s symptoms. Radiating pain down left shoulder – traction injury / Radiating pain down right shoulder – compression injury. Perform bilaterally and do NOT perform with suspected cervical spine fracture and/or dislocation. Special Tests: Cervical Compression Test: Patient position: ATC position: Standing behind the athlete with hands interlocked over the top of the patient’s head Procedure: Sitting Press down on the crown of patient’s head Positive test: Pain in upper cervical spine and/or upper extremity Implication; Compression of the facet joints and narrowing of the intervertebral foramen Special Tests Cervical Compression Test: Attempts to duplicate patient’s symptoms by ↑ pressure on cervical nerve roots. Do NOT perform test until cervical fracture, dislocation, or instability has been ruled out. Special Tests Spurling Test (Foraminal Compression): Patient position: ATC position: Standing behind the athlete with hands interlocked over crown of patient’s head Procedure: Seated Patient laterally flexes the head while a compressive force is placed along patient’s cervical spine Positive test: Radiating pain down patient’s arm Implication: Nerve root impingement Special Tests Spurling’s Test: Attempts to compress a cervical nerve root. Do NOT perform until a cervical fracture, dislocation, or instability has been ruled out. Special Tests Cervical Distraction Test: Patient position: ATC position: At head of patient with one hand under the occiput and the other on top of the forehead (stabilizing head) Procedure: Supine (relaxes the muscles acting on the cervical spine) Apply traction on patient’s head, causing distraction of cervical spine Positive test: Relief or reduction in symptoms Implications: Compression of the cervical facet joints and/or stenosis of neural foramina Cervical Distraction Test: Attempts to relieve patient’s symptoms by ↓ pressure on cervical nerve roots. Do NOT perform test until cervical fracture, dislocation, or instability has been ruled out. Special Tests Vertebral Artery Test: Patient position: ATC position: Seated at head of the patient with hands placed under the occiput to stabilize the head Procedure: Supine Passively extend and laterally flex the cervical spine (1) Head is rotated toward the laterally flexed side and held for 30 seconds (2) Positive test: Dizziness, confusion, nystagmus, unilateral pupil changes, nausea Implication: Occlusion of the cervical vertebral arteries Vertebral Artery Test: Used to assure the competency of the vertebral artery prior to initiating treatment or rehabilitation techniques that may compromise a partially occluded artery. Do NOT perform until the presence of a cervical fracture, dislocation, or instability has been ruled out. Positive Test: Refer to physician