What is 'Diprifusor'? Target Controlled Infusion (TCI) of 'Diprivan'
advertisement

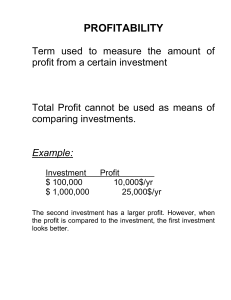
‘Diprifusor’ TCI system Tagged ‘Diprivan’ PFS loaded in syringe pump Full ‘Diprivan’ PFS is loaded correctly Finger grip Tag = PMR (Programmaable Magnetic Resonance*) Aerial ‘Diprifusor’ TCI Subsystem Recognition software/electronics ‘Diprifusor’ TCI Software/ 2 microprocessors Pump hardware Pump software Recognition tag in finger grip of ‘Diprivan’ PFS Important safety features Correct drug identification and usage l Operates in ‘Diprifusor’ TCI mode only with tagged ‘Diprivan’ PFS – no other drugs l Confirms ‘Diprivan’ concentration (1% or 2%) for correct infusion at requested target concentration l Erases tag when PFS is nearly empty and prevents refilling/reuse ‘Diprifusor’ TCI Subsystem Installed in syringe pumps that incorporate ‘Diprifusor’ Functions l Control unit for syringe pump l Recognition of tagged ‘Diprivan’ PFS 8 cm ‘Diprifusor’ TCI Software* Installed in ‘Diprifusor’ TCI Subsystem l Three-compartment pharmacokinetic model Specific set of pharmacokinetic parameters for ‘Diprivan’ (propofol) l Two independent algorithms for infusion control Fail-safe mechanism to enhance patient safety *© University of Glasgow ‘Diprifusor’ TCI System Main components Anaesthetist inputs patient data (age, body weight) Anaesthetist selects and inputs target blood concentration Patient ‘Diprifusor’ TCI Subsystem Microprocessor + pharmacokinetic program Infusion pump incorporating ‘Diprifusor’ Syringe pumps incorporating ‘Diprifusor’ Commercially-available infusion systems* l Graseby 3500 l Vial Médical Master TCI l ALARIS IVAC TIVA TCI * Contact manufacturer for details and availability Display panel of Graseby 3500 During ‘Diprifusor’ TCI Liquid Crystal Display (LCD) CALCULATED concentration TARGET concentration TCI status indicator TCI status indicator Access TOTAL amount of ‘Diprivan’ infused Small increment Small decrement Access INFO on effect site (brain) concentration, time to target... TCI status indicators , the word CALCULATED and symbol blink during infusion Consult Instruction Manual for details of display and operation Display panel of Vial Médical Master TCI During ‘Diprifusor’ TCI Graphical Liquid Crystal Display (LCD) Decrement time (to predict time of awakening) Target concentration Concentration µg/ml Effect-site concentration Calculated concentration Time (minutes/hours) Current infusion rate Consult Operator’s Guide for details of display and operation Main display of ALARIS IVAC TIVA TCI During ‘Diprifusor’ TCI Calculated concentration Target concentration Pump status Volume of ‘Diprivan’ infused Effect-site (brain) concentration and estimate time Chevron keys for Trend graph of calculated concentration increment/decrement Consult Directions for Use for details of display and operation Syringe pumps incorporating ‘Diprifusor’ Common features of commercially-available pumps Input/entry of patient details – age 16–100 years – body weight 30–150 kg Recognition of ‘Diprivan’ 1% or 2% Set and adjust target blood concentrations 0.1–15 µg/ml Display of target concentration Display of continuously changing calculated concentration Access/display calculated effect-site (brain) concentration Predict time to target and patient waking time Access/display infusion rate and volume of ‘Diprivan’ Consult pump manufacturer for detailed specification Target concentrations with ‘Diprifusor’ TCI Principles of setting and adjusting targets 1200 8 Calculated concentration (automatic calculation and display by system) Target concentration (selected by anaesthetist, displayed) 5 Infusion rate (ml/h) 2 3 4 100 4 50 2 1 0 0 0 5 10 15 Time (minutes) 20 25 30 35 Blood concentration (µg/ml) 6 Assessment of accuracy Measurement or predictive performance of a TCI system Bias This value represents the direction (over or under-prediction) of the performance error (median performance error,MDPE) No Bias Calculated concentration Measured concentration Significant Bias Assessment of accuracy Measurement or predictive performance of a TCI system Precision This is an indication of the size of the typical error from the predicted concentration (median absolute performance error,MDAPE) Small Scatter (No Bias) Calculated concentration Measured concentration Large Scatter (No Bias) Predictive performance of ‘Diprifusor’ TCI Median absolute performance error (MDAPE) General surgical patients * (median values) Overall 10% MDAPE 20% 40% 24.1% n = 46 Young (18 – 40 years) n = 10 Middle (41 – 55 years) n = 15 Older (56 years) 30% 22.6% 25.0% 24.2% n = 21 Cardiac patients (pre-bypass) † (mean value) n = 21 23% 20% 40% Proposed maximum acceptable range ‡, ¶ * Swinhoe CF et al. 1998 † Barvais L et al. 1996 ‡ Schüttler J et al. 1988 ¶ Glass PJA et al. 1990 -------UK Population Kinetics !! Individual Kinetics ? CAUSE OF PHARMACOKINETIC VARIATIONS drug concentration errors measurement errors in drug assay inadequate mixing at high infusion rates dose dependent pharmacokinetics technical errors in administration errors in delivery systems patient variability Target concentration and induction time Guidance based on results of ‘Diprifusor’ TCI clinical trial programme Titrate against the response of the patient in order to achieve the depth of anaesthesia required l In adults (under 55 years of age) – usually 4 to 8 µg/ml l In premedicated patients – initial target 4 µg/ml l In unpremedicated patients – initial target 6 µg/ml l Induction time with these targets is generally within the range of 60 to 120 seconds l A lower initial target should be used in patients: – over the age of about 55 years – ASA grades III or IV Consult full, local prescribing information Initial target concentration for induction UK study with prototype ‘Diprifusor’ TCI system----mean indiction time 103s in group 5 µg/ml. Target concentration Percentage of patients successfully induced 100% 5 µg/ml 4 µg/ml 75% 50% 90% 75% 3 µg/ml 40% 25% n = 20 n = 20 Failure of induction (patients not induced within 3 minutes of achieving the target concentration): target increased to 6 µg/ml n = 20 Chaudhri S et al. 1992 Induction time with ‘Diprifusor’ TCI UK study of mainly ASA grade I or II 106 patients Mean induction time (seconds) 20 ‘Diprifusor’ TCI 40 60 80 55 n = 79 (SD 10.6) p < 0.01 Manual control 75 n = 80 (SD 18.8) The initial infusion rate was higher with `Diprifusor´ TCI (1,200 ml/h) than with manual control (600ml/h). The mean dose of `Diprivan´ administered at the time of insertion of the laryngeal mask air way was significantly higher (p < 0.05) with `Diprifusor´ TCI (201 mg) than with manual control (160 mg) Russell D et al. 1995 Quality of induction with ‘Diprifusor’ TCI UK study of mainly ASA grade I or II patients Percentage of patients ‘Diprifusor’ TCI Manual control Poor 2.5% Adequate 22.8% Good 74.7% Poor 5.0% Adequate 22.5% Good 72.5% n = 79 The initial infusion rate was higher with `Diprifusor´ TCI (1,200 ml/h) than with manual control (600 ml/h). The mean dose of `Diprivan´ administered at the time of insertion of the laryngeal mask air way was significantly higher (p < 0.05) with `Diprifusor´ TCI (201 mg) than with manual control (160 mg) n = 80 Hutton P et al. 1995 Quality of maintenance with ‘Diprifusor’ TCI UK study of mainly ASA grade I or II patients Percentage of patients (assessed by observer) ‘Diprifusor’ TCI Manual control Poor 0% Poor 3.8% Adequate 22.4% Good 77.6% Adequate 27.5% Good 68.7% n = 76 The initial infusion rate was higher with `Diprifusor´ TCI (1,200 ml/h) than with manual control (600 ml/h). The mean dose of `Diprivan´ administered at the time of insertion of the laryngeal mask air way was significantly higher (p < 0.05) with `Diprifusor´ TCI (201 mg) than with manual control (160 mg) n = 80 Hutton P et al. 1995 Movement in response to initial surgical incision UK study of mainly ASA grade I or II patients NS p = 0.19 Percentage of patients 30% 28.8% 20% 19.7% 10% Manual control ‘Diprifusor’ TCI n = 80 n = 76 The mean overall infusion rate during maintenance was significantly greater (p = 0.001) in the ‘Diprifusor’ TCI group (13.2 mg/kg/h) than in the manual control group (8.2 mg/kg/h) Russell D et al. 1995 Movement during the remainder of maintenance period Excluding initial surgical incision in UK study p = 0.02 Percentage of patients 30% 26.2% 20% 10% 11.8% Manual control ‘Diprifusor’ TCI n = 80 n = 76 The mean overall infusion rate during maintenance was significantly greater (p = 0.001) in the ‘Diprifusor’ TCI group (13.2 mg/kg/h) than in the manual control group (8.2 mg/kg/h) Russell D et al. 1995 Need for supplementary manual bolus doses Maintenance: UK study of mainly ASA grade I or II patients Percentage of patients requiring supplementary manual bolus doses to deepen anaesthesia 50% 10% 3 – 5 doses 25% 40% 1 – 2 doses 0% Manual control ‘Diprifusor’ TCI n = 80 n = 75 The mean overall infusion rate during maintenance was significantly greater (p = 0.001) in the ‘Diprifusor’ TCI group (13.2 mg/kg/h) than in the manual control group (8.2 mg/kg/h). Setting a higher target concentration with ‘Diprifusor’ TCI results in automatic administration of a bolus Hutton P et al. 1995 Maintenance target concentrations Overall results from ‘Diprifusor’ TCI clinical trial programme Patient type Mean maintenance target concentration Healthy adult patients (ASA I or II) 3.5 to 5.3 µg/ml Cardiac patients (ASA II, III or IV) 2.8 to 3.4 µg/ml Age over 55 years 3.5 µg/ml Haemodynamic effects during ‘Diprifusor’ TCI Overall results from clinical trial programme Induction Maintenance Healthy adults Patients >55 years Cardiac patients systolic BP (mean 12 – 26%) diastolic BP (mean 16 – 28%) (comparable to manual administration) systolic and diastolic BP (similar pattern to younger age groups) Hypotensive effect exacerbated when opioid infusion was started before Diprifusor’ TCI ‘’ Usually little further change in BP from induction Changes in systolic BP >younger age groups Usually little further change in BP from induction Recovery after ‘Diprifusor’ TCI Overall results from clinical trial programme Consistent with rapid early-phase recovery profile of ‘Diprivan’ l Prompt, clear-headed recovery l After short procedures (up to 40 minutes), mean recovery time 5.0 – 10.3 minutes l After long procedures (up to 6 hours), mean recovery time 9.6 – 21.3 minutes l Waking (eyes open) usually occurs at calculated blood concentration 1 – 2 µg/ml Patient characteristics ‘Diprifusor’ TCI clinical trial programme Wide range of adult patients (induction and maintenance) l Age range 16 to 83 years (mean 45.4 years) l Male (n = 186) or female (n = 131) l ASA Class I, II, III and IV l Inpatients and outpatients/day cases l Spontaneous breathing and controlled ventilation n = 317 Types of surgery ‘Diprifusor’ TCI clinical trial programme Variety of procedures (duration of treatment 10 minutes to >8 hours) l l l l l l General Cardiac Gynaecological Orthopaedic Arthroscopic Neurosurgery n = 317 Other drug therapy ‘Diprifusor’ TCI clinical trial programme Wide range of premedicants and supplementary analgesics l Premedication – benzodiazepines (temazepam, diazepam, midazolam) – ranitidine l Pre-induction analgesia – opioids (alfentanil, fentanyl, sufentanil) – ketorolac l Supplementary analgesia – nitrous oxide – alfentanil – sufentanil – alfentanil + nitrous oxide/oxygen – fentanyl + nitrous oxide l Neuromuscular blocking drugs n = 317 Value of TCI in patients with anaesthetic problems Case reports with ‘Diprifusor’ TCI or prototypes l Bronchopleural fistula Donnelly JA & Webster RE, 1991 l Undrained pneumothorax Crofts SL & Hutchison GL, 1991 l Drained pneumothorax Millar FA et al. 1992 l Difficult airway due to fixed-flexion deformity of cervical spine MacKenzie RE & McFadzean WA, 1992 l Myotonic dystrophy Tzabar Y & Marshall R, 1995 Benefits l Maintain precise control of depth of anaesthesia with small incremental changes in target concentrations l Allow most patients to be anaesthetised without episodes of apnoea or exposure to nitrous oxide Tolerability profile of ‘Diprifusor’ TCI Clinical trial programme l Tolerability profile of ‘Diprivan’ (propofol) is unchanged when administered by TCI l Similar pattern of adverse events with ‘Diprifusor’ TCI and manually-controlled infusions of ‘Diprivan’ l Hypotension (1.58%) and sinus bradycardia (1.26%) were the only events with frequency > 1% l No unexpected adverse events revealed l No reports of awareness n = 317 TCI FOR HIGH RISK PATIENTS select a low target concentration of propofol such as 1µg/ml and WAIT to observe the effect time MUST be allowed for adequate equilibration of the effector site increase in steps of 0.5-1.0 µg/ml until the desired effect is achieved 10 8 6 4 2 0 0 10 20 30 10 8 6 4 2 0 0 10 20 30 User preferences on ease of use (convenience) Assessed by questionnaire in ‘Diprifusor’ TCI UK study Feature or variable Number of anaesthetists (n=8) expressing preference ‘Diprifusor’ TCIManual control No preference Ease of set-up Ease of setting target or infusion rate Ease of adjusting depth of anaesthesia Easier to use Preferred choice of infusion technique Statistical analysis was not performed Portability Reliability Russell D et al. 1995 User preferences for ‘Diprifusor’ TCI Assessed by questionnaire in European multicentre study Overall preference 93 7 p < 0.05 7 p < 0.05 25 p < 0.05 18 p < 0.05 0 Setting of initial target/ infusion rate 93 Overall ease of set-up 57 Adjustment of depth of anaesthesia 18 79 4 0% 25% 50% 75% 100% Percentage of anaesthetists (n = 28) expressing preference ‘Diprifusor’ TCI Manual control No difference Continued ... Servin F, 1997 User preferences for ‘Diprifusor’ TCI Assessed by questionnaire in European multicentre study continuation Overall preference 93 Management of depth of anaesthesia during syringe change 57 Management of depth of anaesthesia during unexpected syringe changes 50 11 25 Overall ease of use 89 0% 25% 50% 7 75% 7 p < 0.05 32 p < 0.05 25 NS 4 p < 0.05 100% Percentage of anaesthetists (n = 28) expressing preference ‘Diprifusor’ TCI Manual control No difference Servin F, 1997 Movement in response to surgical stimuli European multicentre study Percentage of non-paralysed patients p < 0.05 15% 14.6% 10% 5% 4.6% Manual control ‘Diprifusor’ TCI n = 144 n = 153 Mean overall infusion rate: 11.0 mg/kg/h in manual control group and 12.1mg/kg/h (p < 0.05) in TCI group. Servin FS, 1998 ‘Diprifusor’ TCI: conclusions European multicentre study l ‘Diprifusor’ TCI was easily learnt and well accepted by anaesthetists l For anaesthesia with ‘Diprivan’, the clinical profiles of ‘Diprifusor’ TCI and manual control are very similar l Overall user preference: of the two techniques, ‘Diprifusor’ TCI was preferred by most anaesthetists (93%) and they found it easier to use (89%). Servin FS, 1998 Main points about ‘Diprifusor’ TCI Induction and maintenance of anaesthesia in adult patients Clinical trial programme l Provides guidance on target concentrations in relation to age, ASA status, premedication and supplementary analgesia l Confirms that ‘Diprifusor’ TCI provides the major benefits of ‘Diprivan’: – smooth induction – good quality of maintenance – rapid, clear-headed recovery with low frequency of PONV l Shows that ‘Diprifusor’ TCI compared with manuallycontrolled infusion of ‘Diprivan’ offers additional advantages: – more convenient administration (easier to use) – improved control (more predictable and precise control of the depth of anaesthesia) Benefits to anaesthetist of ‘Diprifusor’ TCI Induction and maintenance of anaesthesia in adult patients Convenience and control l l l l More convenient than manually-controlled infusion Avoids the need for time-consuming calculation of infusion rates Continuous process for induction and maintenance – more convenient than intravenous induction/vaporizer for maintenance Allows wider appreciation and experience of the clinical benefits of ‘Diprivan’ 静脉麻醉的相对不足 RELATIVE DISADVATAGES OF INTRAVENOUS ANESTHESIA 1. 全凭静脉麻醉或靶控输注麻醉的价格昂贵, 特 别是长时 间手术的麻醉 TIVA OR TCI: MUCH MORE EXPENSIVE THAN INHALATION ANESTHESIA, ESPECIALLY IN LONG-TERM SURGERY 2. TCI 技术尚不普及 TCI: NOT POPULAR IN CLINICAL 3. 诱导期血压易波动 BLOOD PRESSURE: EASY BEING FLUCTUITED DURING INDUCTION 4. 给药后麻醉药必须在体内经过完整的药物代谢过程 INTRAVENOUS ANESTHETICS MUST BE METABOLIZED AFTER INJECTION THANK YOU!