Endocrine System - My Anatomy Mentor
advertisement

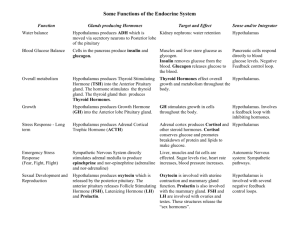
The Endocrine System Endocrine System Function: Regulates Coordinates Integrates Works cooperatively with the nervous system No ducts: Reactions not immediate -last longer than N.S. responses Hormones Substances secreted by cells that regulate the activity of another tissue or organ Most produced by glands Some produced by clusters of cells Some produced by neurons (neurohormones) Hormones Types of Hormones Amino Acid Derivatives Simple amines, thyroxin, peptides and proteins Examples: Thyroid hormones, epinephrine and NE, insulin, glucagon Most hormones this type Hormones Types of hormones Steroid hormones Derived from cholesterol Includes gonadal hormones (sex hormones) and adrenal hormones (cortex only) Examples: Progesterone, testosterone, cortisol, aldosterone Hormones Types of hormones Eicosanoids Are paracrine hormones (local hormone = produced by cells and released to effect cells in the same area) Examples: Prostaglandins, leukotrines Intracellular Receptors Receptors On the target cell -bind hormone Determine the effect the hormone will have on the target cell Binding may cause: Change in membrane permeability or potential Synthesis of substances such as proteins or enzymes Activation or deactivation of enzymes Secretion of substances Stimulation of mitosis Hormone Actions Alter the activity of target cells Decrease or increase cellular activity in target cells Only affect cells with receptors for that hormone Hormone action: What happens when a hormone binds with a receptor? 1. Channels 2. 2nd messenger 3. Genes HORMONE ACTION Where are the receptors? 1. On the cell membrane (AA hormones) intracellular second messenger 2. In the nucleus (steroid hormones & thyroxine) direct gene activation HORMONE ACTION- Second Messenger Intracellular second messenger Hormone Receptor G protein Adenylate cyclase system Cyclic AMP Protein kinases Hormone Mechanisms Second Messengers Hormone binds to a receptor on plasma membrane Series of reactions initiated within the cell Example: Cyclic AMP Second Messengers Cyclic AMP (cAMP) Formed from ATP when a hormone binds to receptor Hormone/receptor binding ‘G’ protein activates or inhibits adenyl cyclase ATP converted to cAMP May activate protein kinases Initiates cascade of enzymes within the cell Effect depends upon target cell Second Messenger System Second Messengers PIP Mechanism PIP2 split into diacylglycerol and IP3 Both act as second messengers IP3 triggers the release of calcium from the ER Ca2+ acts as a third messenger Diacylglycerol may activate protein kinases Second messenger system Direct Activation of Genes Steroid hormones can pass through the plasma membrane Bind to receptors inside cell Hormone/receptor binding stimulates genes on the DNA to begin protein production Gene Activation Hormone Regulation Nervous System Ultimate control of hormone mechanisms belongs to the nervous system Mainly hypothalamus and sympathetic nervous system Endocrine Gland Stimuli Hormone Regulation Stimulation or inhibition of endocrine glands comes from THREE sources: Other hormones Humoral stimuli Neural stimuli Hormone Regulation Hormonal Regulation (by other Hormones) Hormones may stimulate or inhibit the release of other hormones Hypothalamus Regulates anterior pituitary gland Pituitary hormones Stimulate release of hormones from other glands Hormone Regulation Regulation by Humoral Stimuli Changing ion or nutrient levels in the blood may inhibit or stimulate the release of hormones Example: Low blood calcium (Ca2+) PTH released from the parathyroid glands Ca2+ released from bone Increase in blood Ca2+ Hormone Regulation Regulation by Neural Stimuli Nerve impulses may stimulate the release of hormones Example: Sympathetic neurons stimulate release of epinephrine and norepinephrine from the adrenal medulla Feedback Mechanisms Negative Feedback System Rising hormone or ion levels inhibit further hormone release from the gland Positive Feedback System Rising hormone levels cause an increase in the hormone being secreted Hypo or Hypersecretion May result in a disorder Examples: Diabetes Grave’s disease Addison’s disease Cushing’s disease Major Endocrine Glands Pituitary Gland (Hypophysis) Posterior lobe (Neurohypophysis) Releases 2 hormones produced in the hypothalamus posterior lobe anterior lobe Posterior Pituitary Gland Posterior Lobe Derived from hypothalamus Posterior lobe + infundibulum = neurohypophysis Neuron axons to pituitary = hypothalamic hypophyseal tract hypothalamic hypophyseal tract Posterior Pituitary Gland Two hormones released here Both produced in nuclei of the hypothalamus Both secreted into capillaries in posterior pituitary for distribution to the body Oxytocin & ADH Hypothalamus SON/PVN – produce ADH & oxytocin Released from posterior pituitary Pituitary Posterior lobe: • Pituicytes ADH Oxytocin Posterior Pituitary Gland Supraoptic Nucleus ADH (Vasopressin) Paraventricular nuclei Stimulates increased reabsorption of water by kidney tubules Decreases urine volume Increases blood volume Supraoptic nuclei React to Osmoreceptors Paraventricular Nucleus Oxytocin Uterine contractions Milk release (Contraction of mammary gland smooth muscle ADH & oxytocin Ventral Hypothalamus Releasing and inhibiting hormones Thru portal system Target = anterior pituitary Anterior Pituitary Gland Hypophyseal Portal System neurons in ventral hypothalamus primary capillary plexus hypophyseal portal veins secondary capillary plexus secretory cells Anterior Pituitary Gland Ventral hypothalamus Anterior Lobe = Adenohypophysis Derived from roof of mouth Produces hormones Release of hormones is controlled by hormones from neurons of the ventral hypothalamus = releasing or inhibiting hormones anterior lobe Pituitary (Hypophysis) Location and relationships Densely packed cells (anterior) Anterior lobe: TSH ACTH FSH LH GnRH Growth h. Prolactin MSH Anterior Pituitary Gland The following four anterior pituitary hormones are tropic hormones Tropic Hormones: TSH ACTH FSH LH Tropic Hormones Hormones Secreted Thyroid Stimulating Hormone (TSH) Stimulates production and release of thyroid hormones by the thyroid gland Release stimulated by TRH Inhibited by rising blood levels of thyroid hormone Tropic Hormones Hormones Secreted Adrenocorticotropic Hormone (ACTH or Corticotropin) Stimulates secretion of corticosteroid hormones (esp. cortisol) from the adrenal cortex Release stimulated by CRH, fever, hypoglycemia and stress Inhibited by rising cortisol levels Tropic Hormones Hormones Secreted Follicle Stimulating Hormone (FSH) Not present until puberty Stimulates gamete production and maturation in both males and females Release stimulated by GnRH Inhibited by rising gonadal hormones Anterior Pituitary Gland Hormones Secreted Luteinizing Hormone (LH) Promotes production of gonadal hormones Controlled by the same hormones as FSH Triggers ovulation in females Non-tropic Hormones Hormones Secreted Growth Hormone (GH) or Somatotropin Produced in response to growth hormone releasing hormone (GHRH from hypothalamus) Also secreted in response to hypoglycemia or decreased blood GH or Increased amino acid levels Inhibited by GHIH (somatostatin from hypothalamus) Stimulates cell growth and division in most cells (esp. bone and muscle) Mobilizes fat to conserve glucose Hyposecretion results in pituitary dwarfism Hypersecretion results in gigantism or acromegaly Non-tropic Hormones Hormones Secreted Prolactin (PRL) Release stimulated by PRH Inhibited Both by PIH (dopamine) are influenced by estrogen Stimulates milk production by breasts Thyroid Gland - Anatomy The Thyroid Gland Two lateral lobes Composed of follicles Cuboidal follicle cells produce thyroglobulin Thyroglobulin stored in lumen of follicle Iodine attaches Molecule is split into T3 and T4 (mostly T4) Hormones enter circulation, more T3 formed thyroid gland Thyroid Gland - histology Follicular cells follicles colloid thyroglobulin T3 – triiodothyronine T4 – thyroxine Parafollicular cells Calcitonin Thyroid Gland - hormones Follicular cells thyroglobulin T3 – triiodothyronine T4 – thyroxine • • • + BMR (glucose oxidation) maintains bp tissue growth & development Parafollicular cells Calcitonin • • decreases blood calcium + osteoblasts Thyroid Gland – T3/T4 production Follicles – colloid, follicular cells Cells make thyroglobulin Thyroglobulin moves into follicle Iodine pumped into follicle Iodine used to make subunits • 1 OR 2 IODINE Subunits moved into follicle cells Subunits join to make T3 or T4 T3/T4 released from follicle cells Thyroid Hormone Production Thyroid Hormone T4 converted to T3 once in tissues Secreted in response to TSH Inhibited by rising blood thyroid hormone levels Effects: Increases metabolic rate Increases heat production Promotes protein synthesis and enhances the affect of GH Promotes uptake of glucose by cells Promotes lipid metabolism Speeds up actions of nervous system Thyroid Hormone Hyposecretion Can result in cretinism in children Myxedema in adults Hypersecretion Grave’s Disease Thyroglobulin Thyroid Gland - pathology Myxedema – adult hypothyroid Goiter – enlarged thyroid due to lack of iodine Cretinism – infantile hypothyroid Grave’s disease – hyperthyroid exophthalmos Calcitonin parafollicular cells Secreted by parafollicular or C cells by the thyroid Released in response high blood calcium Stimulates uptake of calcium by bone Parathyroid Glands 4 to 8 on posterior thyroid gland Secrete Parathyroid Hormone (PTH) Secreted in response to low blood calcium Stimulates bone resorption Released calcium enters blood Increases absorption of calcium by intestines and reabsorption by kidneys parathyroid glands Parathyroid Hormone Hypersecretion Depletes calcium from bones Depresses nervous system activity Skeletal muscle weakness Hyposecretion Over excitability of neurons Muscle spasms Convulsions Chief cells Adrenal (Suprarenal) Glands Two glands--one on top of each kidney Outer cortex, inner medulla adrenal gland Cortex Produces over 2 dozen corticosteroids from cholesterol Increased hormone output in response to ACTH or stress cortex medulla Adrenal Cortex Three Regions: Zona Glomerulosa Outer region Production of mineralocorticoids (aldosterone) Regulation of electrolyte & fluid balance Aldosterone 95% of mineralocorticoids Sodium reabsorption (and water) by kidney tubules Increases blood volume and pressure Stimulated by angiotensin Renin secreted by kidneys Activates angiotensin hormones in blood Stimulates release of aldosterone Inhibited by Atrial Natriuretic Factor (ANF) Secreted by heart cells when B.P. rises Blocks secretion of renin and aldosterone Adrenal Cortex Zona Fasciculata Middle region Secretes glucocorticoids (cortisol) Cortisol Released in response to ACTH Inhibited by increased cortisol Promotes gluconeogenesis (production of glucose from non-carbohydrate sources) Causes a rise in B.P. Anti-inflammatory if given in higher doses Cortisol Hypersecretion Cushing’s Syndrome Depressed bone and cartilage formation Depressed inflammatory response and immune system Edema, hypertension, loss of muscle and bone, ‘moon face’ Hyposecretion Addison’s disease Drop in blood plasma volume Inability to cope with stress or regulate blood sugar levels Increased skin pigmentation Adrenal Cortex Zona Reticularis Inner region Produces glucocorticoids & gonadocorticoids (androgens and estrogen) ADRENAL MEDULLA Chromaffin Cells Secrete epinephrine and norepinephrine (Catecholamines) Release stimulated by sympathetic neurons Prolongs the fight or flight response The Pancreas Mixed endocrine and exocrine function Acinar Cells Secrete digestive enzymes into small intestine Islets of Langerhans Contain alpha cells Glucagon Contain beta cells Insulin Pancreas endocrine and exocrine Islets of Langerhans Cell Types: Alpha Beta Delta Glucagon Insulin Somatostatin Increases blood sugar PP Pancreatic Polypeptide Regulates exocrine function Inhibits bile release Decreases blood sugar Inhibit glucagon/insulin release Inhibit digestive tract activity Insulin Stimulated by high blood sugar Inhibited by decrease in blood sugar or somatostatin (GHIH) Lowers blood sugar Enhances glucose transport into cells (esp. muscle) Stimulates glycogen formation Promotes conversion of glucose to fat Stimulates protein synthesis in muscle Islet of Langerhans Glucagon Released in response to low blood sugar Mobilizes fatty acids, glucose and amino acids from storage Promotes release of fat from adipose tissue Promotes: Gluconeogenesis (production of glucose from non-carb. sources) Glycogenolysis (breakdown of glycogen into glucose) Raises blood sugar levels Diabetes Diabetes Insipidus Caused by ADH deficiency Large quantities of urine Dehydration No blood sugar accumulation Diabetes Mellitus Results from Hyposecretion of insulin or hypoactivity of insulin Diabetes Diabetes Mellitus Two types: Type 1 (Juvenile Onset) Usually before age 20 Decreased amount of beta cells in pancreas Possibly autoimmune cause Long term vascular and neural problems Type 2 (Adult Onset) Insulin is produced but receptors are resistant to it Family tendencies Influenced by weight, diet and exercise Diabetes Lack of insulin or response to it Inability of glucose to enter body cells High blood sugar Fat stores are mobilized for fuel Blood sugar and fatty acid levels rise higher Ketone bodies build up from breakdown of fatty acids Ketosis or acidosis results (lowered blood pH) Crisis, coma or death Diabetes Symptoms Polyuria Large urine output Polydipsia Excessive thirst Polyphagia Excessive hunger caused by the inability to use glucose as an energy source The Pineal Gland Secretes melatonin May affect responses to light cycles May inhibit gonad activity in humans until puberty “brain sand” The Thymus Gland Shrinks with age Produces thymopoietin and thymosin Aids in development of the immune response (development of Tlymphocytes) THE GONADS Produce gametes and reproductive hormones Testosterone in males Maturation of reproductive organs Secondary sex characteristics Sex drive Estrogens and progesterone in females Estrogens cause maturation of reproductive organs and appearance of secondary sex characteristics With progesterone, promote breast development and cyclic changes in uterine lining