Approach to the Patient with Liver Disease
advertisement

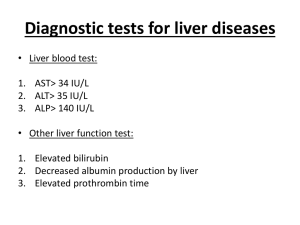
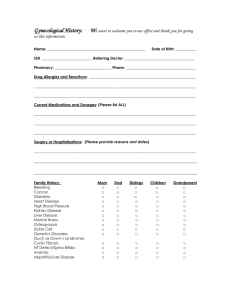
Approach to the Patient with Liver Disease Chapter 301 Harrison 2012 Baghbanian M. Gasteroentrologist Sadughi hospital 1390/7/27 Diagnosis of liver disease is made by : Careful history Physical examination Laboratory tests Radiologic examinations Liver biopsy – less for diagnosis than for grading and staging Liver Structure and Function • largest organ of the body • 1–1.5 kg • 1.5–2.5% of lean body mass. • size and shape of the liver vary and match the general body shape The liver is located in ? RUQ under the right lower rib cage against the diaphragm and projects into the LUQ The liver is held by ? Ligamentous attachments to the diaphragm Peritoneum Great vessels Upper gastrointestinal organs Liver blood supply? Dual blood supply: 20% : hepatic artery(oxygen-rich) from celiac artery 80% : portal vein (nutrient-rich ) from stomach, intestines, pancreas, and spleen Liver cells? The majority of cells : – hepatocytes (2/3 of the mass of the liver) The remaining cell are: – – – – Kupffer cells (reticuloendothelial system) stellate (Ito or fat-storing) cells endothelial cells and blood vessels bile ductular cells Liver structure? In light microscopy: Lobules with portal areas at the periphery and central veins in the center of each lobule. Portal areas? Consist of : small veins Arteries bile ducts lymphatics organized in a loose stroma of matrix and collagen. Acini? physiologic unit of the liver : helps to explain the morphologic patterns and zonality of many vascular and biliary diseases not explained by the lobular arrangement. Acini fenestrae in sinusoids→ free flow of plasma but not cellular elements. plasma is in direct contact with hepatocytes in the subendothelial space of Disse. Acini Blood flowing: – zone 1 → zone 3 of the acinus – portal veins → hepatic (central ) veins Bile flowing: zone 3 → zone 1 of the acinus Hepatocytes function? 1-synthesis of most proteins – (albumin, coagulation factors) 2-production of bile – (bile acids, cholesterol, phospholipids) 3-regulation of nutrients – (glucose, glycogen, lipids, amino acids) 4-metabolism and conjugation of compounds for excretion in bile or urine – (bilirubin, drugs) most commonly liver "function" tests Serum bilirubin – is a measure of hepatic conjugation and excretion Albumin and prothrombin time – are measures of protein synthesis. hepatic dysfunction: Abnormalities of bilirubin, albumin, and prothrombin time liver disease patterns? Hepatocellular diseases : inflammation and necrosis – (viral hepatitis or alcoholic liver disease) Cholestatic diseases: inhibition of bile flow – (gallstone or malignancy , primary biliary cirrhosis) Mixed pattern: hepatocellular + cholestatic – ( cholestatic forms of viral hepatitis and many drug-induced liver diseases). Liver disease patterns is important? pattern of onset + prominence of symptoms can rapidly suggest a diagnosis symptoms of liver disease? Fatigue Itching RUQ pain Nausea Poor appetite Abdominal distention GI bleeding liver disease with no symptoms? Many patients with liver disease are no symptomatic Manifestaion : abnormalities in liver tests – As a part of a routine physical examination – Or screening for blood donation – Or for insurance or employment. Diagnosis : HOW? 1- PATTERN of disease? – (hepatocellular, cholestatic, or mixed injury) 2- Specific ETIOLOGIC ? 3- Grading ? – (severity or activity of disease—active or inactive, and mild, moderate, or severe) 4-Staging ? – (whether acute or chronic; early or late; precirrhotic, cirrhotic, or end-stage) Clinical history should focus on symptoms of liver disease: – their nature – patterns of onset – patterns of progression — potential risk factors for liver disease. Clinical history Symptoms can also suggest the presence of: cirrhosis and end-stage liver disease complications of cirrhosis such as portal hypertension. Fatigue The most common and most characteristic symptom of liver disease. Typically after activity or exercise Rarely present or severe in the morning after adequate rest afternoon versus morning Nausea Vomiting Nausea occurs with more severe liver disease May be provoked by odors of food or eating fatty foods. Vomiting can occur but is rarely persistent or prominent. Poor appetite with weight loss Poor appetite with weight loss occurs commonly in acute liver diseases but is rare in chronic disease Except advanced cirrhosis Diarrhea Diarrhea is uncommon in liver disease Except with severe jaundice – lack of bile acids can lead to steatorrhea RUQ pain RUQ pain occurs in many liver diseases and is usually marked tenderness The pain arises from stretching or irritation of Glisson's capsule, which is rich in nerve endings. Severe RUQ pain Is most typical of: – Gallbladder disease – Liver abscess – Severe venoocclusive disease Occasional accompaniment of acute hepatitis. Itching acute liver disease – early in obstructive jaundice – later in hepatocellular disease (acute hepatitis). chronic liver diseases – cholestatic disease (PSC and PBC) occur before the onset of jaundice – Itching can occur in any liver disease, particularly cirrhosis Jaundice hallmark symptom of liver disease and perhaps the most reliable marker of severity. Patients usually report darkening of the urine before scleral icterus. Jaundice is rarely detectable in bilirubin level <2.5 mg/dL. severe Jaundice With severe cholestasis : lightening of the color of the stools steatorrhea Jaundice without dark urine Usually indicates indirect hyperbilirubinemia : Hemolytic anemia Genetic disorders of bilirubin conjugation – Gilbert's syndrome : common and benign – Crigler-Najjar syndrome:rare and severe – Gilbert's syndrome affects 5% of the population; jaundice is more : after fasting and stress. Risk factors for liver disease • • • • • • • • • Personal habits ( Alcohol use , Injection drug use) Medications ( herbal , OCP, and over-the-counter) Sexual activity Exposure to jaundiced or other high-risk persons Recent surgery Remote or recent blood products transfusion Occupation Accidental exposure to blood or needlestick Familial history of liver disease. assessing the risk of viral hepatitis Careful history of sexual activity include: – the number of sexual partners – for men, a history of sex with men. Sexual exposure is : common mode of spread of hepatitis B rare for hepatitis C Assessing the risk of viral hepatitis A family history of hepatitis, liver disease, and liver cancer is also important. Maternal-infant transmission occurs with both hepatitis B and C Vertical spread of HBV can now be prevented by passive and active immunization of the infant at birth Vertical spread of hepatitis C Is uncommon There are no reliable means of prevention Transmission is more common in : – HIV-co-infected mothers – Prolonged and difficult delivery – Early rupture of membranes – Internal fetal monitoring History of injection drug use Even in the remote past, is important for hepatitis B and C. Injection drug use is now the single most common risk factor for hepatitis C Blood transfusion Transfusion with blood products is no longer an important risk factor for acute viral hepatitis Before : 1992 is important risk factor for hepatitis C. – HCV Ab didn’t checked 1986 is a risk factor for hepatitis B. – anti-HBc didn’t checked Risk factors for hepatitis A Travel to an underdeveloped area of the world Exposure to persons with jaundice Exposure to young children in day-care centers Eating shellfish(rare) Risk factors for Hepatitis E Is more common in Asia and Africa Eating raw or undercooked pork or game (deer and wild boars) Tattooing and body piercing? For hepatitis B and C are frequently mentioned but are actually quite rare types of exposure Alcohol In the United States,70% of adults drink alcohol , but significant alcohol intake is less common more than 2 drinks (22–30 g) per day in women 3 drinks (33–45 g) in men a A Alcoholic liver disease drunk for 10 years Family history Familial causes of liver disease include: – Wilson's disease – Hemochromatosis – Alfa 1 antitrypsin deficiency – Familial intrahepatic cholestasis – Benign recurrent intrahepatic cholestasis – Alagille syndrome. Wilson's disease Severe liver disease in childhood or adolescence with a family history of liver disease or neuropsychiatric disturbance investigation for Wilson's disease Hemochromatosis Liver disease in adulthood WITH: – Family history of cirrhosis – Diabetes – Endocrine failure investigation of iron status Hemochromatosis Adult patients with abnormal iron studies genotyping of the HFE gene for the C282Y and H63D mutations Alfa1 ATD A family history of emphysema + liver disease investigation of 1AT levels if low →Pi genotype Physical examination Complements rather than replaces the need for other diagnostic approaches. Is normal In many patients unless the disease is acute or severe and advanced. Can reveal signs that point to a specific diagnosis, either in risk factors or diseases . Physical examination Typical physical findings in liver disease are: Icterus Hepatomegaly Hepatic tenderness Splenomegaly Spider angiomata Palmar erythema Excoriations Signs of advanced liver disease? Muscle wasting Ascites and edema Dilated abdominal veins Hepatic fetor Asterixis Mental confusion Stupor and coma. Bruising Males with cirrhosis Particularly when related to alcohol signs of hyperestrogenemia (gynecomastia, testicular atrophy, and loss of male-pattern hair distribution ) Physical examination - Icterus Sclera under natural light. fair-skinned individuals : yellow skin may be obvious dark-skinned individuals, the mucous membranes below the tongue demonstrate jaundice. Jaundice is rarely detectable if the serum bilirubin level is < (2.5 mg/dL) but may remain detectable below this level during recovery from jaundice (protein and tissue binding of bilirubin). Spider angiomata and palmar erythema occur in: Acute liver disease Chronic liver disease Especially prominent in cirrhosis Occur in normal individuals and are frequently during pregnancy Spider angiomata? Superficial, tortuous arterioles fill from the center outward. only on the arms, face, upper torso Pulsatile and difficult to detect in dark-skinned individuals Hepatomegaly Is not a very reliable sign of liver disease (variability of the size and shape) Marked hepatomegaly is typical : – Cirrhosis – Venoocclusive disease – Infiltrative disorders (amyloidosis, metastatic or primary cancers of the liver,alcoholic hepatitis.) Hepatomegaly Careful assessment of the liver edge may also demonstrate unusual: – Firmness – Irregularity of the surface – Frank nodules Splenomegaly occurs in many medical conditions but can be a significant physical finding in liver disease. The availability of ultrasound (US) assessment of the spleen allows for confirmation of the physical finding. Ascites Ascites is best appreciated by attempts to detect shifting dullness by careful percussion. US examination will confirm the finding of ascites in equivocal cases. Edema ; causes? Hypoalbuminemia Venous insufficiency Heart failure Medications(NSAID) Hepatic failure? signs or symptoms of hepatic encephalopathy in a person with severe acute or chronic liver disease. . first signs of hepatic encephalopathy ? change in sleep patterns and personality irritability mental dullness In acute liver failure: mania may be present Physical findings Hepatic failure? asterixis and flapping tremors of the body and tongue. Fetor hepaticus : • slightly sweet, ammoniacal odor • in patients with liver failure • particularly portal-venous shunting of blood Other causes of coma Electrolyte imbalances Sedative use Renal failure Respiratory failure should be excluded in liver disease Hepatic encephalopathy in acute hepatitis Is major criterion for: • Diagnosis of fulminant hepatitis • Indicates a poor prognosis. Hepatic encephalopathy In chronic liver disease usually triggered by a medical complication : – GIB – Over diuresis – Uremia and electrolyte imbalance – Dehydration – Infection – Constipation – Narcotic analgesics. Hepatic encephalopathy examination? Connect a series of 25 numbered circles rapidly using a pencil. – The normal range is 15–30 seconds – delayed in patients with early encephalopathy. drawing abstract objects comparison of signature to previous. Other signs of advanced liver disease Umbilical hernia from ascites Hydrothorax Prominent veins over the abdomen Caput medusa • resulting from the recanulation of the umbilical vein. hyperdynamic circulation • Widened pulse pressure Hyperdynamic circulation cirrhosis fluid and sodium retention increased cardiac output reduced peripheral resistance hyperdynamic circulation Widened pulse pressure Hepatopulmonary syndrome? In patients with long-standing cirrhosis and portal hypertension Defined by triad : – liver disease – hypoxemia – pulmonary arteriovenous shunting. Hepatopulmonary syndrome examination? Characterized by: platypnea orthodeoxia – shortness of breath and oxygen desaturation that occur paradoxically in upright position pulse oximetry is reliable screening test Skin disorders in liver disease Hyperpigmentation in: chronic cholestatic diseases (PBCand PSC) Xanthelasma and tendon xanthomata as result of retention of lipids and cholesterol. Gray pigmentation occurs with hemochromatosis Mucocutaneous vasculitis with palpable purpura :typical of cryoglobulinemia of HCV but also occur in HBV. Specific physical signs in liver disease Kayser-Fleischer ring • in Wilson's disease • golden-brown copper in Descemet's membrane at periphery of the cornea • best seen by slit-lamp examination. Dupuytren contracture , parotid enlargement – suggestive of alcoholic liver disease Laboratory Testing Tests of liver injury: – ALT , AST – AlkP – Bilirubin Tests of liver function: – Albumin – Prothrombin time. Further testing may be necessary: Gama glutamyl transpeptidase (gGT) – ALP elevations is due to liver disease? Viral hepatitis serology Markers of PBC (AMA) Markers of sclerosing cholangitis (P-ANCA) Markers of AIH(antinuclear, smooth-muscle, liver-kidney microsomal Ab). Diagnostic Imaging US and CT: – Have a high sensitivity for detecting biliary duct dilatation – First-line options in patient with obstructive jaundice. Imaging in Fatty liver All three modalities can detect a fatty liver, which appears bright CT and MRI in fatty liver : quantify liver fat monitoring therapy visualization of the biliary tree MRCP offers several advantages over ERCP no need for contrast media or radiation images can be acquired faster less operator dependent no risk of pancreatitis. MRCP: is superior to US and CT for choledocholithias It is useful in congenital biliary abnormalities. visualization of the biliary tree ERCP: is more valuable in ampullary lesions and PSC allows for biopsy , direct visualization of the ampulla and CBD, intraductal SONO. provides several therapeutic options in obstructive jaundice (sphincterotomy, stone extraction, and placement of nasobiliary catheters and biliary stents.) Hepatic vasculature imaging Doppler US and MRI are used to assess: – hepatic vasculature and hemodynamics – monitor surgically or radiologically placed vascular shunts such as transjugular intrahepatic portosystemic shunts. Diagnostic Imaging in hepatic masses CT and MRI are indicated for the evaluation of : – hepatic masses – staging of liver tumors – preoperative assessment sensitivity is high specificity remains a problem two and sometimes three studies are needed Diagnostic Imaging -elastography Measure hepatic stiffness as a means of assessing hepatic fibrosis US and MR elastrography – Detect hepatic fibrosis – Obviate the need for liver biopsy Elastography may be an appropriate means of monitoring fibrosis and disease progression Interventional radiologic techniques -Biopsy of lesions radiofrequency ablation Chemoembolization of cancer Insertion of drains into hepatic abscesses Measurement of portal pressure vascular shunts Liver Biopsy The criterion standard in the evaluation of liver disease, particularly chronic liver diseases. Is necessary for diagnosis sometimes Is more useful in: – Assessing the severity (grade and stage) – Predicting prognosis – Monitoring response to treatment Liver Biopsy The size of the liver biopsy length of 1.5–2 cm is necessary for accurate assessment of fibrosis. noninvasive means of assessing disease activity ( blood tests) and fibrosis (elastography ) may replace liver biopsy in assessing stage and grade of disease. Liver Biopsy Usually not needed in the diagnosis and management of acute liver disease exceptions that diagnosis remains unclear despite thorough clinical and laboratory investigation. Is helpful in the diagnosis of: – Drug-induced liver disease – acute alcoholic hepatitis. Liver Biopsy liver biopsy plays an important role in the diagnosis of: – – – – – Autoimmune hepatitis Primary biliary cirrhosis Nonalcoholic steatohepatitis Alcoholic steatohepatitis Wilson's disease (quantitative hepatic copper ) Strict diagnostic criteria have not been developed for most liver diseases Liver Biopsy liver biopsy is an invasive procedure and not without complications → should be used only when contribute to management and therapeutic decisions For patients with suspected liver disease 1- initial testing for routine liver tests such as bilirubin, albumin, ALT, AST, AlkP 2-These results will establish whether the pattern of abnormalities is hepatic, cholestatic, or mixed. For patients with suspected liver disease whether the disease is acute or chronic? – If the disease is acute and if history, laboratory tests, and imaging studies do not reveal a diagnosis liver biopsy establish the diagnosis. – If the disease is chronic liver biopsy can be helpful not only for diagnosis but also to grade the activity and stage the progression of disease. liver disease evaluation in Immunocompromized patients In patients with HIV infection or after bone marrow or solid organ transplantation, 1- evaluation of opportunistic infections (adenovirus, cytomegalovirus, coccidioidomycosis) 2- vascular and immunologic conditions (venoocclusive disease, graft-versus-host disease). Causes of chronic liver disease? The most common Causes are : – – – – – – – – – Chronic hepatitis C Alcoholic liver disease Nonalcoholic steatohepatitis Chronic hepatitis B Autoimmune hepatitis Sclerosing cholangitis Primary biliary cirrhosis Hemochromatosis Wilson's disease. Grading • Grading refers to an assessment of the severity or activity of liver disease, whether acute or chronic; active or inactive; and mild, moderate, or severe. • Liver biopsy is the most accurate means of assessing severity, particularly in chronic liver disease. Serum aminotransferase levels Noninvasive means to follow disease activity, But not always reliable in reflecting disease severity. Normal aminotransferase levels in HBsAg(+) patients Indicate: – Inactive HBsAg carrier state or – Mild chronic hepatitis B or – Fluctuating disease activity Serum testing for: Hbe antigen HBV DNA (can help resolve these different patterns) but these markers can also fluctuate and change over time. Serum aminotransferase levels in chronic hepatitis C Similar to hepatitis B , serum aminotransferase levels can be normal despite moderate activity of hepatitis C disease. • Serum aminotransferase levels in steatohepatitis In alcoholic and nonalcoholic steatohepatitis: – aminotransferase levels are quite unreliable in reflecting severity. In these conditions, liver biopsy is helpful in guiding and recommending therapy scales for grading activity in chronic liver disease The most common are: – Histology activity index – Ishak histology scale. The amount of fibrosis is generally staged on: – 0 to 4+ in Metavir scale – 0 to 6+ scale in Ishak scale Staging in chronic liver diseases staging=amount of fibrosis the most accurate method :Liver biopsy Early stage staging precirrhotic Cirrhotic Mild to moderate stages of hepatic fibrosis are detectable only by liver biopsy. importance of staging? Prognosis Guiding management of complications Cirrhotic Patients are candidates for : – Screening and surveillance for: Esophageal varices Hepatocellular carcinoma Cirrhosis can be staged clinically? Child-Pugh classification is reliable staging system : (from 5–15) 5 and 6 → class A (compensated cirrhosis) 7–9 → indicating class B 10–15 → indicating class C . This scoring system was initially devised to stratify patients into risk groups prior to undergoing portal decompressive surgery. Child-Turcotte-Pugh Scoring of Liver Disease Severity Parameter 1 point 2 points 3 points Bilirubin (uM) <35 35-50 >50 Albumin (g/l) >35 30-35 <30 Prothrombin (%) >76 76-63 <63 Encephalopathy none mild (gr. 1-2) severe (gr. 3-4) Ascites none moderate severe, refractory Class A = 1-6; Class B = 7-9; Class C = 10-15 points importance of Child-Pugh score Reliable predictor of survival in liver diseases Predicts the likelihood of major complications of cirrhosis such as bleeding from varices and spontaneous bacterial peritonitis. Assess prognosis in cirrhosis Provide the standard criteria for listing liver transplantation Child-Pugh score of >7 (class B) Decompensation of cirrhosis listing liver transplantation. M×odel for end-stage liver disease (MELD score) Assessing for liver transplantation: MELD score Child-Pugh system Less center-to-center variation More objective Three noninvasive variables: – INR – serum bilirubin – serum creatinine PELD (pediatric end-stage liver disease ) Children below the age of 12 years Using : – Bilirubin – INR – Serum albumin – Age – Nutritional status Nonspecific Issues in Management of Patients with Liver Disease Alcohol use Medications Vaccination Surveillance for complications of liver disease Management of Alcohol use Patients with Liver Disease Alcohol use: – Alcohol should be used sparingly, by patients with liver disease. – Abstinence should be encouraged for: • all alcohol-related liver disease • cirrhosis • receiving interferon-based therapy for hepatitis B or C. Vaccinations in Patients with Liver Disease All patients with liver disease should receive: – HAV vaccine Those with risk factors should receive; – HBV vaccine should also be encouraged: – Influenza vaccine – pneumococcal vaccine Medications in Patients with Liver Disease Patients with liver disease should be careful using any medications, other than the most necessary. Drug-induced hepatotoxicity can: – Mimic many forms of liver disease – Exacerbate of chronic hepatitis and cirrhosis Drugs should be suspected in which the cause of exacerbation is unknown surveillance for complications of chronic liver disease Variceal hemorrhage upper endoscopy Patients with cirrhosis: endoscopic obliteration beta blocker Hepatocellular carcinoma: – Patients with cirrhosis – US of the liver at 6- to 12-month intervals. Healthy Liver Hepatic Fibrosis Cirrhosis Liver Cancer THE END Macronodular cirrhosis Micronodular cirrhosis Visible signs of advanced liver cirrhosis Gynecomastia Ascites Caput Medusae Umbilical hernia