Slide 1 - The 21st Cochrane Colloquium
advertisement

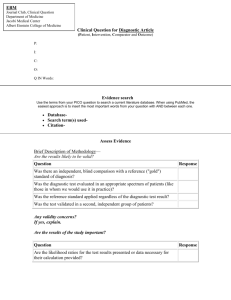
Challenges in conducting a systematic review of the diagnostic accuracy of genetic tests: an example of the genetic diagnosis of familial hypercholesterolaemia P Sharma1, G Mowatt1, F Stewart1, C Boachie1, Z Miedzybrodzka2, W Simpson4, D Boyers1,3, M Kilonzo3, P McNamee3 1. Health Services Research Unit, University of Aberdeen, 2. Clinical Genetics Centre, University of Aberdeen, 3. Health Economics Research Unit, University of Aberdeen, 4. Clinical Biochemistry Laboratory, NHS Grampian, Aberdeen. CONTACT: Pawana Sharma at p.sharma@abdn.ac.uk RESULTS - QUALITATIVE ANALYSIS BACKGROUND AND AIM The availability and uptake of genetic tests is increasing. In 2010 the Aberdeen HTA group were commissioned by the UK National Institute for Health Research Health Technology Assessment (NIHR HTA) Programme to undertake a systematic review of Elucigene FH20 and LIPOchip for the diagnosis of familial hypercholesterolaemia1 on behalf of the National Institute for Health and Care Excellence (NICE) Diagnostics Assessment Programme. Figure 1: Key methodological challenges in conducting a systematic review of the diagnostic accuracy of genetic tests Difficulty defining the reference standard AIM: To explore the methodological challenges involved in undertaking a systematic review of the diagnostic accuracy of genetic tests. Heterogeneity across studies Lack of valid diagnostic indices METHODS Inability to perform meta-analysis 1) Descriptive analysis of the issues encountered and measures undertaken to resolve these issues during the conduct of the systematic review1 (Table 1). 2) Comparative analysis to assess the extent to which the issues faced during this review were also encountered by other reviews. This comprised: • Overview of systematic reviews of the diagnostic accuracy of genetic tests • Qualitative analysis of the methodological aspects (for example, whether or not meta-analysis was performed, susceptibility to bias, quality of reporting etc.) Key methodological challenges in conducting a systematic review of the diagnostic accuracy of genetic tests Difficulty adhering to the strict inclusion criteria as defined a priori Evidence gap in terms of both quantity and quality • Quantitative assessment of clinical validity, (for example, by comparing the proportion of studies that reported diagnostic indices such as sensitivity, specificity, and the variability of these results) RESULTS - QUANTITATIVE ASSESSMENT OF CLINICAL VALIDITY RESULTS - DESCRIPTIVE ANALYSIS Table 1: Examples of issues encountered, measures undertaken to resolve the issues and suggested recommendations Issues encountered Description of the issue Decision made Dilemma in selection Applying the original of studies strict selection criteria would have resulted in only 3 studies being included. Selection criteria were relaxed, in consultation with the expert advisory panel. Comprehensiveness of the reference standard Studies using a reference standard that did not include coverage of PCSK9 were included as this was still considered to be sufficiently comprehensive in correctly classifying FH. The PCSK9 gene, a part of the recognised reference standard, is rare and was discovered in 2003, hence would not have been included in the reference standard prior to this date. Lack of false positive Only the index testdata negatives went on to receive further genetic tests, including the reference standard. Meta-analysis not conducted as planned Limited evidence base for economic modelling The lack of sufficient diagnostic indices and heterogeneity across studies (e.g., clinical criteria, version of tests used). It was not possible to provide pooled estimates. Recommendation suggested 100% 90% Sharma 2012 (our review) 80% Input from scientific experts versed in the technology should be sought from the design phase. While considering reference genetic tests, the evolution of gene discovery over time, reflecting developments in genetics, should also be taken into account. Gerhardus 2007 Bryant 2008 70% 60% 50% 40% 30% 20% Specificity was assumed to be 100% (no false positives). However, these studies were judged to be affected by partial and differential verification biases. 10% Diagnostic measures may not be adequately reported and metaanalysis may not be possible or appropriate. An alternative analysis plan should be Forest plots of considered in advance sensitivity and should this eventuality specificity were used to occur. visualise the heterogeneity amongst the included studies. Sensitivity was taken from a single study and 100% specificity was assumed. Figure 2: Diagnostic indices and variability of these results as reported by the studies included in three reviews Sensitivity analyses should explore the impact of study choices and assumptions on cost-effectiveness results. Decisions addressing these issues were made in consultation with our project expert advisory panel. 0% Sensitivity Specificity Positive predictive value Negative predictive value 95% Confidence interval CONCLUSIONS • Genetic tests are continuing to evolve, reviewers should obtain input from scientific/technical experts from the study design phase and undertake intensive scoping of the review question. • The paucity of well designed studies included in the three genetic test reviews made a valid assessment of the tests difficult. Study investigators should design studies to allow calculation of specificity as well as sensitivity where possible. REFERENCES 1. Sharma P et al. Elucigene FH20 and LIPOchip for the diagnosis of familial hypercholesterolaemia: a systematic review and economic evaluation. Health Technol Assess 2012;16(17). 2. Bryant J et al. A systematic review of the clinical validity and clinical utility of DNA testing for hereditary haemochromatosis type 1 in at-risk populations. J Med Genet 2008;45:513-518. 3. Gerhardus A et al. Diagnostic accuracy of methods for the detection of BRCA1 and BRCA2 mutations: a systematic review. European Journal of Human genetics, 2007;15:619-627. ACKNOWLEDGMENTS RESULTS - COMPARATIVE ANALYSIS Two additional systematic reviews2,3 of the diagnostic accuracy of genetic tests were selected for comparison. Six major methodological challenges were identified from the three reviews (Figure 1). A quantitative assessment of clinical validity is presented in Figure 2. The Health Services Research Unit is core funded by the Chief Scientist Office of the Scottish Government Health and Social Care Directorates. The systematic review of Elucigene FH20 and LIPOchip was funded by the HTA programme (project number 10/70/01) and published in Health Technol. Assess. 2012;16(17). Further information available at: http://www.hta.ac.uk/project/2450.asp. The views and opinions expressed are those of the authors and do not necessarily reflect those of the Chief Scientist Office, HTA programme, NIHR, NICE, NHS or the Department of Health. We thank the NICE assessment subgroup specialist members and Lara Kemp, Cynthia Fraser and Graeme MacLennan for their support. Website: http://www.abdn.ac.uk/hsru