reproduction-a&p
advertisement

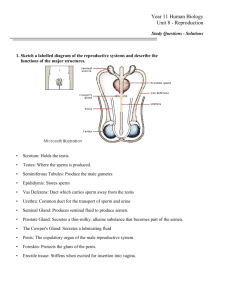
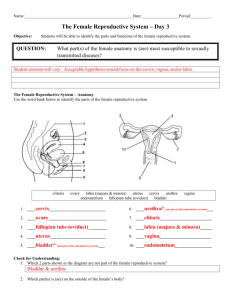
ANATOMY AND PHYSIOLOGY The REPRODUCTIVE SYSTEM MALE & FEMALE Female Reproductive system – organs and function Menstrual cycle Secondary sexual charecteristics Male Reproductive system – organs and function Contraception THE FEMALE REPRODUCTIVE ORGANS Vagina Cervix uteri - "neck of uterus" External orifice of the uterus Canal of the cervix Internal orifice of the uterus corpus uteri - "Body of uterus" Cavity of the body of the uterus Fundus (uterus) THE LAYERS & LIGAMENTS OF THE UTERUS Endometrium Myometrium Perimetrium Peritoneum broad ligament of the uterus (mesometrium) round ligament of uterus ovarian ligament (or "proper ovarian ligament") OVARY Ovaries are oval shaped and, in the human, measure approximately 3 cm x 1.5 cm x 1.5 cm. The ovary is located in the lateral wall of the pelvis in a region called the ovarian fossa. The fossa usually lies beneath the external iliac artery and in front of the ureter and the internal iliac artery. STRUCTURE OF THE OVARY The outermost layer is the germinal epithelium. The tunica albuginea covers the cortex. The ovarian cortex consists of ovarian follicles and stroma in between them. Included in the follicles are the cumulus oophorus, membrana granulosa, corona radiata, zona pellucida, and primary oocyte. The zona pellucida, theca of follicle, antrum and liquor folliculi are also contained in the follicle. Also in the cortex is the corpus luteum derived from the follicles. The innermost layer is the ovarian medulla. It can be hard to distinguish between the cortex and medulla, but follicles are usually not found in the medulla. OVARY OVARIAN HORMONES – OESTROGEN & PROGESTERONE They induce and maintain the physical changes of puberty and the secondary sex characteristics. They support maturation of the uterine endometrium in preparation of implantation of a fertilized egg. They provide signals to the hypothalamus and pituitary that help maintain the menstrual cycle. Oestrogen plays an important role in maintaining subcutaneous fat, bone strength, and some aspects of brain function. THE COMPETITIVE GIRLS OESTROGEN PROGESTERONE 3 – oestrone, oestrdial, oestriol Secreted by ovary + corpus luteum Produced by ovary Peaks 5-7 days after ovulation Peak before ovulation Together with FSH & LH – puberty changes Balancing & protecting from oestrogen dominance Increases libido Decreases libido Maintains the lining of uterus Increases uterine lining Stimulates new bone growth Slows down resorption of bones More effects on pregnancy Maturation and release of egg Encourages fat burning Fat storage Natural diuretic Salt & water retention Precursor to stress hormones CHOLESTEROL HORMONES Cholesterol Pregnenolone Progesterone PROGESTERONE – THE PRECURSOR Cortisol Aldosterone Progesterone Oestrogen Testosterone MENSTRUAL CYCLE The menstrual cycle is a recurring cycle of physiological changes in the females that is associated with reproductive fertility. The length of a woman's menstrual cycle will typically vary, with some shorter cycles and some longer cycles. A woman who experiences variations of less than 8 days between her longest cycles and shortest cycles is considered to have regular menstrual cycles. The PHASES Menstrual phase – discharge of endometrial lining Follicular phase (also known as proliferative phase) Ovulation (not a phase, but an event dividing phases) Luteal phase (also known as secretory phase) Ischemic phase (some sources group this with secretory phase) THE GONADOTROPHICS FSH – FOLLICLE STIMULATING Maturation of ovarian follicles Regulated by GnRH – hypothalamus Negative feedback loop LH – LUTEINISING Growth and maturation of follicle Stimulates ovary to produce T, O & P To form the corpus luteum from ovarian follicles MENARCHE & MENOPAUSE The menstrual cycle is under the control of the reproductive hormone system and is necessary for reproduction. A woman's first menstruation is termed menarche, and is one of the later stages of puberty in girls. The average age of menarche in humans is 12 years, but is normal anywhere between ages 8 and 16. Factors such as heredity, diet and overall health can accelerate or delay menarche. The cessation of menstrual cycles at the end of a woman's reproductive life is termed menopause. The average age of menopause in humans is 51 years, with anywhere between 40 and 58 being common. Menopause before age 35 is considered premature. The age of menopause is largely a result of genetics; however, illness, certain surgeries, or medical treatments may cause menopause to occur earlier. SECONDARY SEXUAL CHARACTERISTICS Growth of pubic hair and development of breast are the most noticeable, others being change in skin tone- smoother, finer crown hair, widens the pelvis and hips increases the amount of body fat in hips, thighs, buttocks, and breasts. Oestrogen also induces growth of the uterus, proliferation of the endometrium, and menses. increase of subcutaneous fat with decrease in facial hair. FALLOPIAN TUBES In humans, the Fallopian tubes are about 7–14 cm long. There are four regions of the fallopian tube from the ovary to the uterus: Infundibulum - contains Fimbria Ampulla - usual site of fertilization Isthmus Intramural oviduct - inside wall of uterus VAGINA The human vagina is an elastic muscular canal that extends from the cervix to the vulva. Although there is wide anatomical variation the average vagina is 6 to 7 inches (15.24 to 17.78 cm) in length; its elasticity allows it to stretch during sexual intercourse and during birth to offspring. The vaginal opening is at the back (caudal) end of the vulva, behind the opening of the urethra. The vagina, along with the inside of the vulva, is reddish pink in colour, as with most healthy internal mucous membranes in mammals. Length, width and shape of the vagina may vary. Vaginal lubrication is provided by the Bartholin's glands near the vaginal opening and the cervix and also seeps through the vaginal wall (which does not contain any glands). FERTILIZATION When an ovum is developing in an ovary, it is encapsulated in a sac known as an ovarian follicle. On maturity of the ovum, the follicle and the ovary's wall rupture, allowing the ovum to escape and enter the Fallopian tube. There it travels toward the uterus, pushed along by movements of cilia on the inner lining of the tubes. This trip takes hours or days. If the ovum is fertilized while in the Fallopian tube, then it normally implants in the endometrium when it reaches the uterus, which signals the beginning of pregnancy. Occasionally the embryo implants into the Fallopian tube instead of the uterus, creating an ectopic pregnancy, commonly known as a "tubal pregnancy". THE BREAST The breasts of a female’s body contain the mammary glands, which secrete milk used to feed infants. The breasts are modified sudoriferous (sweat) glands, producing milk. Each breast has one nipple surrounded by the areola. The areola is coloured from pink to dark brown and has several sebaceous glands. The larger mammary glands within the breast produce the milk. They are distributed throughout the breast, with two-thirds of the tissue found within 30 mm of the base of the nipple. These are drained to the nipple by between 4 and 18 lactiferous ducts, where each duct has its own opening. The remainder of the breast is composed of connective tissue (collagen and elastin), adipose tissue (fat), and Cooper’s ligaments. THE PENIS The penis is an external male sexual & reproductive organ and for mammals additionally serves as the external organ of urination. The human penis is made up of 3 columns of erectile tissue the two corpora cavernosa (singular: corpus cavernosum) and one corpus spongiosum The corpus spongiosum lies on the underside (known also as the ventral side) of the penis; the two corpora cavernosa lie next to each other on the upper side (dorsal side). The end of the corpus spongiosum is enlarged and bulbousshaped and forms the glans penis. The glans supports the foreskin or prepuce, a loose fold of skin that in adults can retract to expose the glans. The area on the underside of the penis, where the foreskin is attached, is called the fraenum (or fraenulum). BLOOD AND NERVE SUPPLY Artery -Dorsal artery of the penis, Deep artery of the penis, Artery of the urethral bulb Vein -Dorsal veins of the penis Nerve -Dorsal nerve of the penis Lymph -Superficial inguinal lymph nodes Precursor -Genital tubercle, Urogenital folds TESTES Like the ovaries, testicles are components of both the reproductive system (gonads) and the endocrine system (endocrine glands). The functions of the testicles are: producing sperm (spermatozoa) producing male sex hormones-testosterone Both functions of the testicle, sperm-forming and endocrine, are under control of gonadotropic hormones produced by the anterior pituitary: luteinizing hormone (LH) follicle-stimulating hormone (FSH) THE DUCTS OF THE TESTES Under a tough membranous shell- tunica albugina, the testis contains very fine coiled tubes called the seminiferous tubules. The tubes are lined with a layer of cells that, from puberty into old-age, produce sperm cells. The sperm travel from the seminiferous tubules to the rete testis- to the efferent ducts, and then to the epididymis where newly-created sperm cells mature. The sperm move into the vas deferens, and are eventually expelled through the urethra and out of the urethral orifice through muscular contractions. Between the seminiferous tubules are special cells called Leydig cells (interstitial cells) where testosterone and other androgens are formed. SECONDARY SEXUAL CHARACTERISTICS Testosterone directly increases size and mass of muscles, enhancing strength prominent Adam’s apple with larger vocal cords, deepening the voice, changing the shape of the face and skeleton. Testosterone converted into DHT in the skin, it accelerates growth of androgen-responsive facial and body hair. Taller stature is largely a result of later puberty and slower epiphyseal fusion. Broadening of shoulders, chest, hands and feet; heavier bone structure; fat deposits around abdomen and waist. COMPOSITION OF SEMEN The components of semen come from two sources: sperm, and "seminal plasma". Seminal plasma, in turn, is produced by contributions from the seminal vesicle, prostate, and bulbourethral glands. The seminal plasma provides a nutritive and protective medium for the spermatozoa during their journey through the female reproductive tract. The normal environment of the vagina is a hostile one for sperm cells, as it’s very acidic (from the native microflora producing lactic acid), viscous, and patrolled by immune cells. The components in the seminal plasma contain basic amines such as putrescine, spermine, spermidine and cadaverine - are responsible for the smell and flavour of semen. These alkaline bases counteract the acidic environment of the vaginal canal, and protect DNA inside the sperm from acidic denaturation. THE SPERM The sperm cell consists of a head 5 µm by 3 µm and a tail 50 µm long. The head- The acrosome contains lytic enzymes which are released when the sperm reaches an ovum. These enzymes digest the outer membrane of the egg, allowing penetration of the sperm. The head also contains a single set of chromosomes derived from the male. This will include either an 'X' or 'Y' chromosome, because of the way the XY separate during meiosis. The middle - contains numerous mitochondria. These provide the energy for movement of the tail. Spermatozoan stream lines are straight and parallel. The tail flagellates, which propels the sperm cell (at about 1-3 mm/minute in humans) by whipping in an elliptical cone. CONTRACEPTION This can be divided into these categories: External / Barrier– Male condoms, Female condoms, Diaphragm, cervical cap, sponges, IUCD - copper T loop, other loops, Hormonal - contraceptive pill- the combined, the morning after pill, progesterone only mini pills, hormonal injections, subcutaneous implants, Vaginal spermicidal creams/jellies Cycle/ periodic awareness Withdrawal – coitus interruptus Sterilization – male (vasectomy), female(tubal ligation)