Presentation1 NN
advertisement

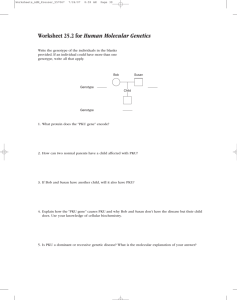
INBORN ERRORS OF METABOLISM Recognize IEM in a neonate with nonspecific signs and symptoms Make use of simple lab tests in the diagnosis of IEM Initial management of life threatening conditions associated with IEM An inherited enzyme deficiency leading to the disruption of normal body metabolism Accumulation of a toxic substrate (compound acted upon by an enzyme in a chemical reaction) Impaired formation of a product normally produced by the deficient enzyme 3 Affects amino acid & protein, carbohydrate, and lipid metabolism. Most disorders are autosomal recessive in transmission Most disorders are evident at or soon after birth. Early detection and treatment are essential to the prevention of irreversible cognitive impairment and early death 4 A B C product deficiency substrate excess D toxic metabolite 5 Disorders of: Amino acids Carbohydrates Fatty acid Lysosomal and peroxisomal function Mitochondrial Organic acids Metabolic Diseases Can Grouped as Defects of Carbohydrates-Glycogen storage disease(GSD), Galactosemia, Defects of amino acids-Phenylketonuria(PKU), Alkaptonuria,Urea cycle defects(UCDs). Organic acidemias-isovaleric acidemia, propoinic acidemia(PPA), methylmalonic acidemia(MMA), maple syrup urine disease(MSUD). Defects of lipids-Mitochondrial fatty acid oxidation defects, peroxisomal disorders ,lysosomal disorders ,mucopolysaccharidoses. Defects of purines and pyrimidines-Lesh-nyhan syndrome Miscellaneous –wilson disease,alpha-1-anti trypsin deficiency. Diagnosis/ Newborn Screening ◦ Nonselective screening – screening all newborns for a limited number of common inborn errors ◦ Selective – testing of an individual known to be at increased risk (e.g. sibling) ◦ Tandem mass spectroscopy – allows clinicians to screen for > 30 disorders Clinical manifestations ◦ Usually appear 24 hours or more after birth, attributed to ingestion of precursor substrate of defective enzyme ◦ CNS symptoms, poor growth, failure to thrive, developmental delays, specific neurological deficits ◦ May have blatant signs (i.e. unusual odor) Lens dislocation : Sulfite oxidase deficiency Skin changes : Biotinidase deficiency Peroxisomal disorders : Zellweger syndrome Large fontanelle prominent forehead flat nasal bridge epicanthal folds hypoplastic supraorbital ridges Pyruvate dehydrogenase deficiency Epicanthal folds flat nasal bridge small nose with anteverted flared alae nasi long philtrum Glutaric aciduria type II Macrocephaly high forehead flat nasal bridge short anteverted nose ear anomalies hypospadias rocker-bottom feet Cholesterol biosynthetic defects Smith-Lemli-Opitz syndrome: Epicanthal folds, flat nasal bridge, toe 2/3 syndactyly, genital abnormalities, cataracts Congenital disorders of glycosylation: Inverted nipples, lipodystrophy Lysosomal storage disorders: Hurler-like phenotype Clinical manifestations – diagnosis ◦ Laboratory studies ◦ Routine Hypoglycemia, acid-base balance, hyperammonemia, ketosis ◦ Specialized studies Require special lab Directed analysis for amino acids or organic acids © 2007 Thomson - Wadsworth Approaches to Treatment In most cases, treatment needs to be instituted empirically without a specific diagnosis. The metabolic screen helps to broadly categorize the patient’s IEM (e.g. urea cycle defect, organic academia, congenital lactic acidosis etc), on the basis of which, empirical treatment can be instituted Aims of treatment 1. To reduce the formation of toxic metabolites by decreasing substrate availability (by stopping feeds and preventing endogenous catabolism) 2. To provide adequate calories. 3. To enhance the excretion of toxic metabolites. 4. To institute co-factor therapy for specific disease and also empirically if diagnosis not established. 5. Supportive care-Treatment of seizures (avoid sodium valproate – may increase ammonia levels), -Maintain euglycemia and normothermia, -Fluid, electrolyte & acid-base balance, -Treatment of infection, -Mechanical ventilation if required. Management of hyperammonemia: 1) Discontinue all feeds. Provide adequate calories by intravenous glucose and lipids. Maintain glucose infusion rate 810mg/kg/min. Start intravenous lipid 0.5 g/kg/day (up to 3 g/kg/day). After stabilization gradually add protein 0.25 g/kg till 1.5 g/kg/day. 2) Dialysis is the only means for rapid removal of ammonia, and hemodialysis is more effective and faster than peritoneal dialysis. Exchange transfusion is not useful. 3) Alternative pathways for nitrogen excretion-: -Sodium benzoate. -Sodium phenylbutyrate -L-arginine (oral or IV) -L-carnitine (oral or IV) 4) Supportive care: Treatment of sepsis,seizures,ventilation. 1. 2. 3. 4. Determine if there is metabolic acidosis Is anion gap >16? Is there hypoglycemia? Is there hyperammonemia? ◦ Within 24 HOL? ◦ After 24 HOL? Copyright ©1998 American Academy of Pediatrics Organic acidemia Healthy NB rapidly ill, ◦ Ketoacidosis, poor feeding Vomiting, dehydration Hypotonia, lethargy Tachypnea, seizures Coma, unusual odors Labs: Urine organic acids Ketonuria (in the NB)- pathognomonic of IEM Neutropenia, thrombocytopenia +/- hyperammonemia Abnormal acylcarnitine Treatment: Stabilize Get rid of organic acid intermediates, and ammonia- hemodialysis Carnitine After stabilization, may resume oral feeds Consult dietitian, and metabolic specialist No acidosis (respiratory alkalosis) No ketones (unlike organic acidemia) No hypoglycemia But with hyperammonemia Treatment: Remove ammonia Hydration with D10 + electrolytes D/C all protein x 24 hours—calories from CHO and fat Na phenylacetate/Na benzoate Give arginine Protein restriction for life Prognosis: guarded Even with Treatment, many will die Definitive treatment: liver transplant An inborn error of carbohydrate metabolism in which the hepatic enzyme (galactose-1-phosphate uridyl transferase), GALK1 or GALE, which normally converts galactose into glucose is absent. Autosomal recessive pattern Incidence It occurs in approximately 1 out of every 60,000 Dietary Lactose Galactose Galactose 1-Phosphate BRAIN Mental retardation LIVER Jaundice Hetaptomegaly Cirrhosis Glucose EYES cataracts Galactose-1 phosphate uridyl transferase deficiency (classic galactosemia, the most common and most severe form)- (GALT) Type I Deficiency of galactose kinase – (GALK1)Type II Deficiency of galactose-6-phosphate –epimerase (GALE)-Type III Jaundice, vomiting poor feeding infections Failure to thrive hepatomegaly Speech disabilities, mental retardation Galactosemia clinical pictures Mild Cataract in the infant The only way to treat galactosemia is through dietary restrictions from the first days of life No brest feeding Soya- based formula • The newborn with questionable results on newborn screening should continue to be treated with soybased formula pending definitive results of confirmatory testing. Why? If unscreened and untreated, galactosemia is a life-threatening disorder. When? Neonatal period: 4th day How? Screening of every neonates, followed by confirming tests. Thereby, affected infants are treated before they become ill. Phenylketonuria is a genetic disorder where the body’s enzyme, phenylalanine hydroxylase ,is missing or malfunctioning so that it cannot properly break down the amino acid, phenylalanine . Mental Retardation Seizures Microcephaly (small head size) Skin rashes Stunted growth Hyperactivity “Musty or mousy” body odor from the excess phenylalanline Fair skin, hair, and eyes (phenylalanine is linked to melanin production) PKU is usually diagnosed after birth with a blood test taken from the infant’s heel or the crook of their arm. ◦ If there are abnormal amounts of phe, then further tests (blood and urine) are taken to ensure that the child has PKU. Another option of diagnosis is through the chorionic villus sampling (CVS) process. Treatment Once diagnosed, babies are fed diets containing protein without phenylalanine for the first 7-10 days. Special infant formula called Lofenalac Recently, there’s been a special medical (pill) formula discovered for PKU patients called Kuvan. It’s possible to have a wide range of PKU, from mild to severe, but it’s suggested to stick to a diet regiment for life. There’s usually a general list of foods that should not be consumed for PKU patients like: ◦ Dairy ◦ ◦ ◦ ◦ ◦ ◦ Milk, eggs, Cheese Nuts Beans Peas Meat (Poultry, beef, pork, duck etc.) Chocolate the sweetener aspartame can act as poisons for people with phenylketonuria Prevention: Unfortunately, if PKU is already diagnosed in an infant, there are no preventive measures one can take for their child to not have PKU. If a pregnant individual has PKU, then she’s able to prevent her child from PKU symptoms if she follows a diet low in protein. 50 Inherited as an autosomal recessive trait caused by mutations in the IDU Agene (4p16.3) Metabolic defect: inability ◦ The body's to make an enzyme: lysosomal alpha-L-iduronase 51 Approximately 1 in 150,000 infants are affected Newborn infants with this defect appear normal at birth By the end of the first year, signs of impending problems begin to develop 52 © 2007 Thomson - Wadsworth Coarse facial features (86.4%) Corneal clouding (70.9%) Heaptomegaly (70.0%) Kyphosis/gibbus (70.0%) Hernias (58.9%) Airway-related symptoms, such as sleep disturbances/snoring (51.6%) Splenomegaly (50.9%) Cardiac valve abnormalities (48.9%) Cognitive impairment (46.4%) Dystosis multiplex (43.6%) © 2007 Thomson - Wadsworth © 2007 Thomson - Wadsworth Hurler syndrome (type I) 56 Mucopolysaccharidosis I (MPS I) Disease (Hurler, Hurler-Scheie, Scheie Syndromes) Key Symptom Images Hernia Corneal clouding Coarse facial features Claw hand 57 58 59 X-linked Coarse, thick, facial features Progressive stiffness decreased mental development Hepatomegaly Splenomegaly Abnormal bone x-rays 60