Skin
advertisement
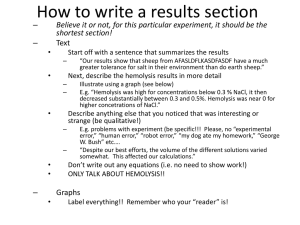
Occam's razor need not apply! ID Case Conference Wednesday March 28, 2007 David Fitzgerald, MD HPI ► ► ► ► 25 yo male immigrated from Guatemala 3 months ago now with complaints of fever, rash, abdominal pain and diarrhea for the last 3 months since arriving in the US. These sxs have worsened over the last 2 weeks prompting his presentation to the ER. Describes abd pain as diffuse and crampy. Diarrhea is currently watery but had been bloody initially. Three months ago he walked across the desert border in Arizona and spent 8 days in the desert short of water and food. After a few days he began to have bloody BM's. No prior episodes of bloody BM's. He saw a doctor recently and was given Aciphex for reflux and a Medrol dose pack for the rash. He was also given an unknown injection. In ER pt had temp to 39.1, was tachycardiac and hypotensive. S/p 8 L of fluid in ER and remained with tachycardia and borderline BP. Increasing O2 requirement as well. Admitted to MICU. ► PMH Reports history of eye surgery as a child ► SH Recent immigrant from Guatamala as above. Married, wife and 15 month old son in Guatamala. Both are well. Lives with his wife’s cousin and several other friends Works at McDonalds Denies ETOH, tobacco or illicit drugs Travel history across desert southwest. ► FH NC ► Meds Acidphex ROS ► ► ► ► ► ► ► ► Gen – fevers, chills, mild NS. 15 Lb wt loss over last 3 months Neuro- No HA, neck stiffness, visual changes, focal weakness or confusion. Friends with him confirm no change in mental status HEENT – denies oral lesions, dysphagia/odynophagia, visual disturbances CV – no cp/palps Pulm – mild cough, non productive. No SOB GI- as above with diarrhea, abd pain. No vomiting, mild nausea. Gu- no ulcers, discharge or dysuria Skin – nonpruritic pink rash that started on his face, moved to his trunk and stomach and then to his arms and legs. Physical exam ► ► ► ► Temp : 39.1 Pulse:115 RR:20 BP 115/70, Sat: 95-98% 2 L General: Pleasant interactive, thin, Hispanic male, in mild distress HEENT – PERRLA, EOMI, Anicteric, mild conj injection bilaterally, ► ► ► ► Confluent, non-tender, blanchable macular erythema on the face and upper trunk. Maculopapular, non-tender, blanchable erythema, proximal>distal extremities. MM dry. No oral lesions or thrush ► ► ► ► Neck – supple Lymph – no cervical, supraclavicular, axillary or inguinal LAN noted CV -Tachy, regular, no mrg Lung – bronchial BS at bases bilaterally. Mild crackles above Abd – soft, mild ttp in R UQ and RLQ, + BS, nondistended. No RB/Guarding. GU- no lesions or discharge Ext – no c/c/e Skin ► Neuro: A+O x 3, non focal strength and sensation grossly, CN2-12 intact Data WBC 14.0 ANC 12.2 ALC 0.4 ► HGB 10.2 (decreased to 8.0 then to 7.3 over 12 hours) MCV 78 RDW 16 Retic count - 0.5% (low) Spherocytes noted Howell Jolly bodies noted ► PLT 395 ► ► ► ► ► ► PT 19.4 INR 1.6 PTT 44 D dimer – 56,000 LDH – 20,000 Fibrinogen 303 AT III 82% low ► Direct Coombs Anti IgG - positive Anti-complement negative ► ► ► ► ► ► ► ► Na 132 K 4.7 Cl 98 HCO3 20 BUN/Cr 18/1.1 Ca 6.0 Mg 1.9 PO4 4.4 ► ► ► ► ► ► LFTS Tbili 0.6 AST 580 ALT 106 Alk Phos 622 GGT 339 DATA ► CRP 17.6 ► UA LE and Nit Neg, 2+ protein, WBC 6, RBC 7 ► Tox screen – negative ► CK 95 ► CSF TNC 2 ► 38% PMNS ► 25% Lymphs RBC <1 Protein 32 Glucose 59 Radiology ► CT chest and abdomen 1. Patchy nodular parenchymal opacifications are concerning for infectious pneumonitis. 2. Inflammatory change of the ascending colon with adjacent free fluid suggests infectious colitis. ► RUQ US – negative for cholecystitis. Nml liver, spleen and kidneys Peripheral smear Diagnoses ► Fungal – Histo Peripheral blood smear – intracellular and extracellular yeast noted CSF cell count – intracellular yeast noted Urine histo ag + ► Bacteremia Blood cx – ► 1. ► 2. Strep Pneumonia E coli ► Viral – HIV, EBV, CMV HIV Elisa + EBV VL - 32,308 CMV VL – 3876 ► Parasitic Fecal cx – 4+ PMNs Fecal O+P –Entamoeba histolytica ► Negative studies Hepatitis serologies negative Bronch – PCP DFA negative CSF – ► HSV PCR neg ► Crypto ag neg Final diagnosis ► Disseminated histoplasmosis with meningitis ► HIV (CD4<10) ► CMV viremia (? Colitis) ► EBV viremia (? Underlying lymphoma) ► Entamoeba histolytica ► Strep Pna and E coli bacteremia ► Hemolytic anemia Warm antibody autoimmune hemolytic anemia (AIHA) ► ► Autoimmune hemolytic anemia (AIHA) due to the presence of warm agglutinins is due to IgG antibodies that react with protein antigens on the red blood cell (RBC) surface at body temperature. For this reason, they are called "warm agglutinins" even though they seldom directly agglutinate the RBCs. ► Various etiologies – Drugs (penicillin, methyldopa, huge list) Infectious agents – usually viral ► Neoplasms (NHL and CLL) ► autoimmune disease (esp SLE) ► Idiopathic (majority) ► AIHA – extravascular hemolysis ► Results in extravascular hemolysis in spleen as deformed RBC (spherocytes) are unable to fit through the slits in the walls of the blind channels in the cords of Billroth Diagnosis ► ► ► ► ► ► ► Hemoglobin usually in the range of 7 to 10 g/dL Positive Direct Coombs test – detects the presence of IgG or complement bound to erythrocyte mebranes Retic count usually elevated above 4 to 5 percent LDH elevated Indirect Bilirubin elevated Haptoglobin decreased Peripheral blood smear usually shows the presence of spherocytosis ► ► The combination of an increased serum LDH and reduced haptoglobin is 90 percent specific for diagnosing hemolysis, while the combination of a normal serum LDH and a serum haptoglobin greater than 25 mg/dL is 92 percent sensitive for ruling out hemolysis Diff dx is that of hemolytic anemia due to drugs and AIHA due to the presence of cold agglutinins (IgM) Complications ► Lymphoproliferative disorder In one series of 108 patients (not HIV) 18% developed a lymphoproliferative disorder after a median time of 2 years ► Venous thromboembolism Reported in both NonHIV and HIV patients AIHA in HIV/AIDS ► ► ► Direct Coombs test is positive in 20-40% of AIDS patients but overt hemolysis is rare Not well studied area due to small numbers of cases reported Pathophysiology of AIHA in AIDS may be related to Hypergammaglobulinemia related to B-Cell dysregulation Direct activation of B cells by HIV Coinfection with EBV or CMV Other infectious agents associated with AIDS may also be associated with production of auto-antibodies ► MAI, CMV, EBV, PCP, M TB, Histoplasma capsulatium AIDS related malignancies Reticulocytopenia ► Reticulocytopenia in AIHA is more common in HIV patients than in the general population ► May lead to underdiagnosis of AIHA in HIV patients ► Theories May be due to antibodies that preferentially destroy reticulocyte precursors May be related to abnormal microenvironment in bone marrow caused by other infections (MAI, Histo, CMV), lymphoma or drugs (ZDV) Treatment ► ► ► ► No great data on the efficacy of various modalities Patients with + Coombs, stable HGB and only mild hemolysis can be monitored Transfusions – may be difficult to cross match Corticosteroids – mainstay of treatment. Prednisone 1 mg/kg daily Quickly slows or stops hemolysis in up to 2/3 of patients and results in increase in HGB within one week Once stabilized can start taper ► IVIG – best used with steroids. Used in severe cases when a rapid response is desired 1 g/kg per day for 2 days May decrease infectious complications of steroids Treatment ► Splenectomy 75% success rate in HIV patients with AIHA Removes the major site of RBC destruction Recommended in patients who do not respond to steroids or cannot be tapered off them Can increase the number of circulating CD4 cells, but not alter the ratio ► Immunosuppressives Not universally accepted, even in those who fail to respond to above treatments Can lead to worsening of anemia by BM suppression ► Plasmapheresis Controversial Due to the large extravascular distribution of IgG and continued AB production Search PubMed ► Autoimmune Hemolytic Anemia (AHIA) Case Reports Reviews Differential Diagnosis Drug Therapy