Clinical Case-Infective Endocarditis
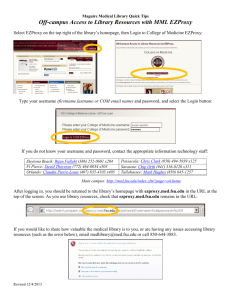
advertisement

Running head: HARRIS_CLINICAL CASE Clinical Case Study Brooke Harris RN, BSN, CCRN Wright State University College of Nursing and Health NUR 7201 1 CLINICAL CASE 2 History and Physical Chief Complaint Per patient’s friend statement “I think she overdosed on heroin” History of Present Illness J.K. is a 24y/o Caucasian female who was brought to the emergency department via EMS along with her friend after being found unresponsive at a party this evening. After EMS administered 0.04mg Narcan intravenously (IV) patient was oriented to person, place, and time however remains drowsy. She states that she only “shot up” one after a few shots of liquor. J.K. states “I got dizzy and just went to lay down for a bit” and has no recollection of being transported to the hospital. J.K. endorses complaints of 8/10 aching throbbing headache. Medical History J. K.’s medical history has included chickenpox as a child and is unsure of her vaccination status, however believes her family physician may have an updated record. She is unsure of her tetanus status, and is unsure of her last visit to her family physician as she is currently unemployed without insurance. She endorses treatment for syphilis three months ago. Social History J. K. is a single woman without children. She is currently unemployed and admits to occasionally prostitution. J.K. admits to use of 1ppd of cigarettes when she can afford them, and states she has used heroin before but only on one occasion. She admits to drinking alcohol, most commonly liquor, regularly at parties. Surgical History J.K. had incision and drainage of abscess in her right antecubital region a several weeks after use of heroin IV. She also had her tonsils and adenoids removed as a young child. CLINICAL CASE 3 Family History J.K’s mother is living at age 56 and suffers from coronary artery disease with history of cardiac stenting, hypertension, diabetes, and hyperlipidemia. J. K.’s father is estranged from the family and his history is unknown. J.K. has one younger sister who is healthy without document alteration in her health history. J.K. has no living grandparent. She has no history of her paternal grandparents. J.K’s maternal grandmother died at the age of 72 from a stroke, and had a history of hypertension and was a smoker. J.K’s maternal grandfather died at age 78 from lung cancer after smoking for 65 years, with only other history being finger amputations following a work related accident. Allergies No known medication allergies Medications She denies use of any medications prescription or over the counter Review of Systems General: Denies fever, c/o chills intermittently over the last month. Current weight is typical HEENT: C/O 8/10 aching throbbing headache at present. Denies any other pain. Denies diplopia, use of corrective lenses, changes in vision, loss of hearing, use of hearing aids. Neck: Denies irritation, stiffness, or pain, or difficulties with range of motion. Chest: Endorses occasional shortness of breath with activity, denies cough or difficulty breathing. Cardiovascular: Denies chest discomfort, palpitation, endorses intermittent leg swelling if she is on her feet for any length of time. CLINICAL CASE Gastrointestinal: Denies abdominal pain, nausea, vomiting, constipation, diarrhea, or indigestion. Denies any alteration in frequency, color, and/or consistency of stool. Genitourinary: Denies frequency, urgency, hematuria, burning, or dysuria. Musculoskeletal: Denies pain or swelling in joints. Denies any recent falls, alteration in mobility or broken bones. Skin: Endorses occasional dry skin, denies any rashes, irritation, or bruising. Neurological: Denies any alteration in level of consciousness, seizures, dizziness, tremors, disturbed thought, or hallucination. Psychosocial: Denies any anxiety or depression, suicidal ideations, homicidal thoughts. States she feels safe in her personal life. Physical Examination Vital Signs: T=100.9, HR=98, BP=119/86, RR=12, O2 saturation 96% on 3L Nasal Cannula. General: Looks older the chronologic age. Appears undernourished, thin, frail, 5’8” weighing 128lbs. HEENT: NC, PERRLA with 2mm pupils, EOMI, no nystagmus present, eyes with clear conjunctive, without drainage. Hearing without difficulties, nose appears midline, nares patent without drainage. Non-tender sinuses. Mouth dry, no lesions noted, missing multiple molars, no tonsils present. Neck: No masses or lesions present, trachea midline no tugging noted, non palpable thyroid, no carotid bruits, non-palpable and non-tender lymph nodes. Cardiovascular: Regular rate and rhythm with S1 and S2 noted. Holosystolic murmur that increases with inspiration appreciated. No gallops, rubs, or clicks noted. PMI non displaced. 4 CLINICAL CASE 5 Pulses 2 + in all areas: doralis pedis, posterior tibial, brachial, radial, femoral, and carotid. No JVD noted. Lower extremities with mild 1+ edema with pitting Chest: CTAB mildly decrease in bases, no wheezing, crackle, or ronchi noted. Equal chest expansion. Respirations even and unlabored. Abdomen: Soft, flat, and non tender, without masses, hepatomegaly noted, no splenomegaly present. Bowels sound present in each of the four quadrants. NO bruits, hums, or rubs noted. Genitourinary: Unable to assess Musculoskeletal: Moves all extremities equally to commands. 5/5 muscle strength in bilateral upper/lower extremities. ROM intact and equally in all extremities without clicking, or popping. Skin: Cool, pink, and dry. Neurological: Drowsy but awakens easily, oriented x3. Following commands appropriately. CN II-XII intact without deficit. Laboratory Data Diagnostic Lab Data NA(135-145 mEq/L) K (3.5-5.1 mEq/L) CL (96-108 mEq/L) CO2 (22-29 mEq/L) Glucose (70-115 mg/dL) BUN (6-23 mg/dL) Creatinine (0.4-1.1 mg/dL) WBC ( 3.8-10.8 k/mm³) RBC (4.4-5.8 g/dL) Hgb (12.2-14.7 g/dL) Hct (37.9-43.9 %) Plt (150-400 k/mm³) Urine Pregnancy Test Urine Drug Screen Differential Diagnosis 148 mEq/L 3.8 mEq/L 98 mEq/L 24 mEq/L 88 mg/dL 20 mg/dL 0.6 mg/dL 15.0k/mm³ 3.9 g/dL 11.7 g/dL 33.2 g/dL 180k/mm³ Negative Positive for opiates. CLINICAL CASE 6 In this case presentation the most concerning symptoms include: elevated temperature 100.9/ fever of unknown origin, holosystolic murmur, hepatomegaly, and lower extremity edema. Most likely causes for fever of unknown origin in this case include infectious processes and/or drug induced (Oxman, 2012). The holosystolic murmur that increases on inspiration or a murmur of tricuspid insufficiency/regurgitation (TR) may be caused by: endocarditis, pulmonary hypertension or right sided heart disease, carcinoid heart disease, rheumatic heart disease, and/or valvular abnormalities such as flail leaflet or prolapse (DeMaria, & Blanchard, 2011). The hepatomegaly could be cause by cirrhosis, cancer, hepatitis, right sided heart disease, venous congestion (Usatine, Smith, Chumley, & Mayeaux, 2013). Finally, in this case the lower extremity could be caused by inflammation, alteration in intravascular permeability, venous obstructions, elevated right heart pressures (Carman, 2012). In this case presentation, with consideration of symptoms including: fever, hepatomegaly, lower extremity edema, and tricuspid regurgitation; the most likely diagnosis is infective endocarditis (IE). (Rothman, Yang, & Marco, 2011). Differentials for IE include rheumatic heart disease, non-infective endocarditis, and valvular abnormality without endocarditis, pulmonary hypertension, and systemic lupus erythematosus (SLE). Rheumatic heart disease (RHD) commonly presents with disease in the mitral (70% of cases) and aortic valve (30-40% of cases) and less frequently with the tricuspid valve (<5% of cases). An echocardiogram would rule out a typical finding of RHD which is carditis or the presence of right/left heart failure. An electrocardiogram would reveal prolong PR segments in a patient with RHD and the patient would likely present with large joint pain/irritation and/or swelling related to the increase likelihood of polyarthritis (Bashore, Granger, Hranitzky, & Patel, 2014). With this case RHD is not CLINICAL CASE 7 completely unlikely and consideration for this process is necessary to for a relevant treatment plan. Non-infective endocarditis, valvular abnormalities without endocarditis would need to be considered as a possible diagnosis however less likely with consideration of an elevated temperature on admission. ECG would be beneficial for assessment of valvular abnormalities, and right/left heart failures finding secondary to abnormalities in the valve (Bashore, Granger, Hranitzky, & Patel, 2014). Assessment via echocardiogram would show the presence or lack of presence of vegetation on valve as well as dysfunction secondary to flail leaflet or prolapsed valve (DeMaria, & Blanchard, 2011). Often individuals with valvular disease have tricuspid regurgitation secondary to pulmonary hypertension or mitral disease leading to back flow of blood into the right-sided cardiac system (Shah, 2011). Pulmonary hypertension (PH) would also need to be ruled out as a possibility for this clinical case. Common findings in PH include: presence of loud pulmonic closure along with right ventricular hypertrophy, which may lead to TR overtime however, no loud closure sound was noted on physical examination. Further findings to rule out PH would include an ECG to assess for tall R waves in V1 and V2 along with an echocardiogram to look for elevated pulmonary pressures and potential right side ventricular enlargement (Barnett & De Marco, 2014). Individuals with PH could also have symptoms of hepatomegaly and lower extremity edema related to increase in venous return (Carman, 2012). Elevated temperature is unlikely with PH, however could be contributed to the use of heroin and would require further work up (Oxman, 2012). SLE often presents with cardiac symptoms, however they tend to differ from IE in the fact that they most commonly have pericarditis and a rub as opposed to a murmur on auscultation (Hahn, 2012). Blood work for SLE includes a test for antinuclear antibodies which are present 98% of the time. Other diagnostic symptoms for SLE not present in this case include arthritis or joint swelling/pain, skin rashes, oral ulcerations, neurologic changes often seizures. Further work-up is necessary; however SLE is considered unlikely (Hahn, 2012). CLINICAL CASE 8 Confirmation of IE according to Duke Criteria includes findings of two major criteria or one major and two minor. The major criteria can come from the following: positive blood cultures (positive for S. Bovis, S. Viridans, HACEK group, S. Aureus or S. Enterococci) drawn 12 hours apart, or (one positive culture with Coxiella burnetii). Other major criteria includes: echocardiography/ ECG suggestive of IE, presence of oscillating mass, abscess, or new/worsening valvular regurgitation. The minor criteria include predisposition of IV drug use, fever greater than 100.4F, vascular phenomena, septic hemorrhages, arterial emboli (Rothman, Yang & Marco, 2011; Nishimura, 2014). Diagnostic criteria will further assist with IE diagnosis (Nishimura, 2014). Relevant Diagnostic Data The most relevant diagnostic data for infective endocarditis includes blood cultures, echocardiography, and monitor of clinical symptoms (Rothman, Yang, & Marco, 2011). In this case first two sets of blood cultures are positive for Staphylococcus Aureus (S. Aureus) bacteria. S. Aureus bacteria in this presence of IV drug use is typically associated with right sided endocarditis (Lowy, 2012). Echocardiography is the mainstay diagnostic tool for IE and should be completed as soon as any cardiac abnormality is detected (Nishimura, 2014). Echocardiography for diagnosis of IE includes transthoracic echocardiogram (TTE) and transeshophageal echocardiogram (TEE), both of which have a 90-100% accuracy for diagnosis of IE. However, the TEE, which has higher sensitivity than the TTE, has shown to display more accurate diagnosis of any vegetation, masses or abscess associated with IE (Nishmura, 2014; DeMaria & Blanchard, 2011). In this case an initial TTE was performed following recognition suspected TR on physical assessment. TTE reveals left ventricular ejection fraction of 65%, along with moderate-severe tricuspid regurgitation and right atrial enlargement is noted as well. CLINICAL CASE 9 There is no presence of elevated pulmonary pressure or right ventricular enlargement showing signs of pulmonary hypertension. TTE show signs of suspected mass on tricuspid valve however further diagnostic testing is recommended (Mutlak, Lessick, Reisner, Aronson, Dabbah, & Agmom, 2007). TEE is performed which confirms the presence of multiple oscillating masses on the tricuspid valve and the right atrial enlargement. These diagnostics are pivotal for an IE diagnosis (Nishimura, 2014). Chest x-ray while not specific enough to display specific valve disease is helpful in displaying right sided heart enlargement (Shah, 2011). Chest CT may be performed in patient with suspected IE that visualization is difficult via TTE or TEE, however in this case is unnecessary (Nishimura, 2014). An electrocardiogram (ECG) shows tall p-waves in lead V1 significant for right atrial enlargement, and is lacking tall R waves in V1 and V2 which is helpful in ruling out specific disease processes. Tall R waves would be present in a patient with pulmonary hypertension (PH) and is helpful in eliminating PH as a cause for this patient TR (Hoit & Crawford, 2014). Plan The plan for individuals with infective endocarditis include initially begins with admission to hospital for further follow-up of blood cultures, symptoms, and echocardiography (Roth, Yang, & Marco, 2011). Secondary patient admitted with IE require a multi-disciplinary approach including cardiology, cardiothoracic surgery, and infectious disease to select appropriate treatment and therapy for the patient (Karchmer, 2012). Patient with IE require blood cultures every other to every third day to assess bacteremia and/or development of different bacterial (Baddour et al., 2005; Lowy, 2012). Antibiotic therapy for S. Aureus IE are Oxacillin 12g/24H IV for four-six weeks. Four week of oxacillin therapy is often sufficient for those with only right sided valvular involvement however assessment of blood culture is necessary to CLINICAL CASE 10 ensure cessation of bacterial growth prior to discontinuation of antibiotic therapy. In addition to oxacillin, an aminoglycoside gentamycin 3mg/kg per 24 hours for as few as a five to ten days (Baddour et al., 2005). Prior to initiation of an aminoglycoside renal function panel should be obtained to rule out renal dysfunction. Gentamicin has high potential for nephrotoxicity and neurotoxicity including ototoxicity and should be closely monitored throughout the administration period (Lexi-Comp, 2014). Weekly monitor of echocardiograms are often helpful in view resolution or worsening of valvular abnormalities (Nishimura, 2014). Routine laboratory monitoring including BMP, CBC is helpful for assessing renal function, electrolytes, trending leukocytosis, following hemoglobin and assessing for anemia (Nishimura, 2014). Important management for this patient includes smoking cessation and possible rehabilitation therapy for drug abuse (Barrow, 2014). This process will need to involve social services and integrative case management related to the patient’s current unemployment status. Long term rehabilitation is key to survival those suffering from drug abuse and/or addiction (Barrow, 2014). Smoking cessation is often helpful with local support groups and can be encouraged by the primary nurses and ACNP caring for the patient (Mahoney, & Cummings, 2011). Admission to inpatient rehabilitation facility may be beneficial for management of IV drug use/abuse (Barrow, 2014). Social services and case management should consider placement in care facility for long term antibiotic therapy related to risk of abuse of central line placed for medication therapy, providers must be aware of the risk of abuse with central line placement at discharge (Mahoney & Cummings, 2011; Barrow, 2014). Follow-up Short term follow-up involves the immediate care needed for improvement. Consideration of outpatient therapy importance lies with evaluating risk vs. benefit for long term CLINICAL CASE 11 antibiotic therapy and the patient safety. Not many IV drug users will qualify for outpatient management related to poor support system and high risk for further drug use. For those with effective support systems and agreement to contracts with physicians and family will often have positive outcomes with outpatient therapy (Baddour, 2005; Nishimura, 2014). A thorough dental evaluation should be completed to assess for areas of increase risk of further development of IE. Follow-up includes bi-weekly visits to the cardiologist for assessment of valvular dysfunction and completion of echocardiogram for evaluation of oscillating masses present during hospitalization while completing antibiotic therapy (Karchmer, 2012; Nishimura, 2014; Baddour, 2005). The patient will need to follow up at two weeks post discharge for assessment/discussion of need for valve repair/replacement. Follow-up with primary physician for laboratory data including blood cultures, BMP, CBC and assessment for worsening infection, or any renal dysfunction related to long term antibiotic and potential for septic emboli from the vegetation on the valve. The patient must be educated regarding signs and symptoms of worsening endocarditis including fever and chills (Nishimura, 2014; Baddour, 2005). Long term follow-up involves providers to stress the importance of daily dental hygiene and regular dental visits. Seek immediate medical attention for any fever related to increase risk for infection. Finally education regarding long term valvular dysfunction and need for supportive therapy. Surgical intervention is typically required for individuals with valvular dysfunction secondary to endocarditis and this should be in a long term plan for optimal outcomes (Baddour, 2005). CLINICAL CASE 12 References Baddour, L.M., Wilson, W. R., Bayer, A.S., Fowler, V.G., Bolger, A. F., Levison, M.E., …Taubert, K.A. (2005). Infective endocarditis: Diagnosis, antimicrobial therapy, and management of complications: A statement for healthcare professionals from the committee on rheumatic fever, endocarditis, and Kawasaki disease, council on cardiovascular disease in the young, and the council on clinical cardiology, stroke, and cardiovascular surgery, and anesthesia, american heart association: Endorsed by the infectious diseases society of america. (2005). Circulation 111,e394-e434. doi: 10.1161/CIRCULATIONAHA.105.165564. Barnett C.F., De Marco T (2014). Chapter 30. Pulmonary Hypertension. In Crawford M.H. (Eds), Current Diagnosis & Treatment: Cardiology, (4th ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=71 5&Sectionid=48214564. Barrows K (2014). Chapter e5. Integrative Medicine. In Papadakis M.A., McPhee S.J., Rabow M.W. (Eds), CURRENT Medical Diagnosis & Treatment 2014.Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=33 0&Sectionid=44291049. Bashore T.M., Granger C.B., Hranitzky P, Patel M.R. (2014). Chapter 10. Heart Disease. In Papadakis M.A., McPhee S.J., Rabow M.W. (Eds), CURRENT Medical Diagnosis & Treatment 2014. Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=33 0&Sectionid=44291012. Carman, T.L. (2012). Chapter 84. Edema. In McKean S.C., Ross J.J., Dressler D.D., Brotman D.J., Ginsberg J.S. (Eds), Principles and Practice of Hospital Medicine. Retrieved July from CLINICAL CASE 13 http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=49 6&Sectionid=41304056. DeMaria, A.N., Blanchard, D.G. (2011). Chapter 18. Echocardiography. In Fuster V, Walsh R.A., Harrington R.A. (Eds), Hurst's The Heart, (13th ed.). Retrieved July 20, 2014 fromhttp://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx? bookid=376&Sectionid=40279744. Hahn B (2012). Chapter 319. Systemic Lupus Erythematosus. In Longo D.L., Fauci A.S., Kasper D.L., Hauser S.L., Jameson J, Loscalzo J (Eds), Harrison's Principles of Internal Medicine, (18th ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=33 1&Sectionid=40727120. Hoit B.D., Crawford M.H. (2014). Chapter 21. Tricuspid & Pulmonic Valve Disease. In Crawford M.H. (Eds), Current Diagnosis & Treatment: Cardiology,(4th ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=71 5&Sectionid=48214554. Karchmer, A.W. (2012). Chapter 124. Infective Endocarditis. In Longo D.L., Fauci A.S., Kasper D.L., Hauser S.L., Jameson J, Loscalzo J (Eds), Harrison's Principles of Internal Medicine, (18th ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=33 1&Sectionid=40726868. Lexi-Comp, Inc. (2014). Retrieved from hhht://webstore.lexi.com/PDA-Software-for-Nurses Lowy, F.D. (2012). Chapter 135. Staphylococcal Infections. In Longo D.L., Fauci A.S., Kasper D.L., Hauser S.L., Jameson J, Loscalzo J (Eds), Harrison's Principles of Internal Medicine, (18th CLINICAL CASE 14 ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=33 1&Sectionid=40726884. Mahoney M.C., Cummings K (2011). Chapter 57. Tobacco Cessation. In South-Paul J.E., Matheny S.C., Lewis E.L. (Eds), CURRENT Diagnosis & Treatment in Family Medicine, (3rd ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=37 7&Sectionid=40349452. Nishimura, R.A., Otto, C. M., Bonow, R. O., Carabello, B. A., Erwin, J. P., Guyton, R. A.,…Thomas, J. D. (2014). 2014 AHA/ACC guideline for the management of patient with valvular heart disease. Journal of the American Cardiology 63(22), 57-185. Retrieved from https://www-clinicalkeycom.ezproxy.libraries.wright.edu:8443/#!/ContentPlayerCtrl/doPlayContent/1-s2.0S0735109714012790/ Mutlka, D., Lessick, J., Reisner, S. A., Aronson, D., Dabbah, S., & Agmom, Y. (2007). Echocardiography-based spectrum of severe tricuspid regurgitation: The frequency of apparently idiopathic tricuspid regurgitation. Journal of the American Society of Echocardiography 20(4), 405-408. Retrieved from https://www-clinicalkeycom.ezproxy.libraries.wright.edu:8443/#!/ContentPlayerCtrl/doPlayContent/1-s2.0S0894731706010005 Oxman, D.A. (2012). Chapter 191. Fever of Unknown Origin. In McKean S.C., Ross J.J., Dressler D.D., Brotman D.J., Ginsberg J.S. (Eds), Principles and Practice of Hospital Medicine. Retrieved fromhttp://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?booki d=496&Sectionid=41304178. CLINICAL CASE 15 Rothman R.E., Yang S, Marco C.A. (2011). Chapter 150. Infective Endocarditis.In Tintinalli J.E., Stapczynski J, Ma O, Cline D.M., Cydulka R.K., Meckler G.D., T(Eds), Tintinalli's Emergency Medicine: A Comprehensive Study Guide,(7th ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=34 8&Sectionid=40381627. Shah, P.M. (2011). Chapter 79. Tricuspid Valve, Pulmonary Valve, and Multivalvular Disease. In Fuster V, Walsh R.A., Harrington R.A. (Eds), Hurst's The Heart, (13th ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=37 6&Sectionid=40279813. Usatine, R.P., Smith, M.A., Chumley, H.S., & Mayeaux, E.J., (2013). Chapter 61. Liver Disease. In Usatine R.P., Smith M.A., Chumley H.S., Mayeaux E.J., Jr.(Eds), The Color Atlas of Family Medicine, (2nd ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bookid=68 5&Sectionid=45361106.