EARLY ACS - Clinical Trial Results
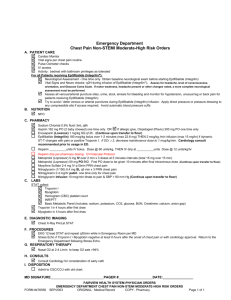
advertisement

Early Glycoprotein IIb/IIIa Inhibition in Non-ST-segment Elevation Acute Coronary Syndrome: A Randomized, Double-blind, Placebo-Controlled Trial Evaluating the Clinical Benefits of Early Front-loaded Eptifibatide in the Treatment of Patients with Non-ST-segment Elevation Acute Coronary Syndromes Disclosures Funded by Millennium Pharmaceuticals and Schering Plough All authors disclose research grant funding and/or consulting and speaking honoraria from Schering Plough Full Relationships with Industry disclosures for all authors are listed in detail in the ACC.09 Presenter Disclosure Digest Study Structure Study Chairman: E. Braunwald Study Co-Chairmen: R. Califf, F. Van de Werf 35 Investigators 24 Countries represented Cardiology and Emergency Medicine DCRI: K. Newby, L. Berdan, R. Harrington TIMI: R. Giugliano CVC: P. Armstrong, C. Sorochuk Helpline: P. Tricoci, P. Sinnaeve Chairman: D. Weaver Members: J. Alpert, E. Cohen, D. Faxon, L. Fisher, F. Verheugt Schering Plough Physician Lead: J. Strony Ops leaders: A. Kilian, L. Layton 440 sites 29 countries Physician Lead: M. Roe Lead Coordinator: D. Montgomery Angio Core: M. Gibson Primary Goal To compare the effect of 2 strategies for eptifibatide administration in high-risk NSTE ACS patients managed with an invasive diagnostic assessment: A strategy of routine, early administration of eptifibatide to all patients shortly after presentation A strategy of delayed, provisional eptifibatide administration at the physician’s discretion after coronary angiography and prior to PCI Study Design 2 of 3 high-risk criteria: 1. Age > 60 years 2. + CKMB or TnT/I 3. ST or transient ST (Or age 50-59, h/o CVD and + CKMB or TnT/I) High-risk NSTE ACS n = 10,500 Routine, early eptifibatide (180/2/180) Placebo / delayed provisional eptifibatide pre-PCI Randomize within 12 hours of presentation Invasive strategy: 12 to 96 hours after randomization Primary Endpoint: 96-hr Death, MI, Recurrent ischemia Safety Endpoints at 120 hrs: Bleeding (GUSTO and TIMI requiring urgent revascularization, or Thrombotic bailout scales), Transfusions, Stroke, Non-hemorrhagic SAEs Key Secondary Endpoint: 30-d Death or MI Key Exclusion Criteria Increased bleeding risk active bleeding or recent bleed Recent surgery or trauma Prior ICH or recent ischemic stroke Serious concomitant illness or pregnancy ESRD with dialysis < 30 days Recent or planned use of direct thrombin inhibitor, fXa inhibitor, abciximab/tirofiban amendment 1: allowed bivalirudin at PCI amendment 2: allowed acute fondaparinux or bivalirudin Blinded Study Drug Administration Investigational double bolus and infusion regimen 180 ug/Kg / 2 ug/kg/min / 180 ug/Kg IV eptifibatide (or matching placebo) • Infusion decreased to 1 ug/Kg/min if CrCl <50 mL/min) Provisional, blinded cross over to open label eptifibatide at time of PCI using blinded bolus kit Bolus kit = Provisional use Eptifibatide Placebo Coronary Angio PCI Bolus Kit = Bailout use Open label Eptifibatide Eptifibatide Placebo Open label Eptifibatide Statistical Methods Power at original sample size (10,500 patients) Primary quadruple composite at 96 hours •85% Power for RRR 22.5% at alpha = 0.048 Death or MI at 30 days •85% Power for RRR 15% at alpha = 0.048 Sample size reduced to 9500 patients when pooled primary event rate greater than expected late in trial 98% power for primary endpoint, 81% power for secondary endpoint * Adjusted for single interim efficacy analysis Enrollment (N = 9492) N = 6595 N = 2897 160 136 625 2272 12 1342 11 374 103 472 128 155 175 50 447 260 96 510 23 178 837 192 51 452 118 57 23 177 47 Follow-up 99.9% complete worldwide Enrollment Top 20 Enrolling Sites 1/ Austria Franz Leisch (304) 11/ Germany Michael Gross (138) 2/ Netherlands A W J van ‘t Hof (301) 12/ Germany Uwe Zeymer (133) 3/ USA Kristin Newby (231) 13/ USA Yale Cohen (119) 4/ India Keyur Parikh (224) 14/ Portugal Luis Providencia (112) 5/ USA Amir Malik (209) 15/ Israel Uri Rosenshein (107) 6/ Israel Basil Lewis (198) 16/ Poland Piotr Ponikowski (95) 7/ Israel Arie Roth (174) 17/ France Khalife Khalife (94) 8/ Germany Peter Schuster (156) 18/ Israel Eugenia Nikolsky (92) 9/ Germany Martin Desaga (151) 19/ Switzerland Michael Pieper (90) 10/ Poland Maria Trusz-Gluza (138) 20/ Canada Manohara Senaratne (88) Baseline Characteristics Routine Early Eptifibatide (n=4722) Age (yrs) 67 (60, 75) Female (%) 32 Diabetes mellitus (%) 30 Hypertension (%) 71 Dyslipidemia (%) 58 Prior MI (%) 27 Creatinine Clearance <50 mL/min (%) 18 Troponin positive (%) 84 ST-segment shifts (%) 62 Symptoms to presentation (hrs) 3.3 (1.4, 8.0) Presentation to randomization (hrs) 5.4 (3.3, 8.8) Delayed Provisional Eptifibatide (n=4684) 68 (60, 75) 31 31 72 58 28 18 84 62 3.2 (1.5, 7.8) 5.7 (3.4, 8.8) In-hospital Management Cardiac Catheterization (%) Randomization to cath (hrs) In-hospital Management (%) CABG Medically Treated only PCI Provisional (before wire) Bailout (after wire) Use of Established Rx (%) Beta-blocker Statin ACEI / ARB Clopidogrel (intended early) Routine Early Eptifibatide Delayed Provisional Eptifibatide (n=4722) (n=4684) 98 98 21.4 (16.9, 34.2) 21.4 (16.7, 31.0) 13 30 13 31 59 25 11 60 27 12 88 86 78 75 88 87 79 75 96-Hour Primary Efficacy Results Routine Delayed Early Provisional Eptifibatide Eptifibatide OR P (95% CI) (n=4722) (n=4684) Death, MI, RIUR, TBO 9.3% 10.0% 0.92 0.23 (0.80-1.06) Death 0.8% 0.9% 0.96 0.87 (0.62-1.50) Death or MI 7.5% 8.3% 0.89 0.13 (0.77-1.04) Death, MI, RIUR 8.4% 9.4% 0.89 0.11 (0.77-1.03) MI, myocardial infarction; RIUR, recurrent ischemia requiring urgent revascularization; TBO, thrombotic bailout Kaplan-Meier Curves for Primary Endpoint Death, MI, RIUR or TBO (%) 15 10.0% 10 Delayed provisional eptifibatide 9.3% P = 0.23 (stratified for intended early clopidogrel use) 5 Routine early eptifibatide 0 0 8 16 24 32 40 48 56 64 72 80 Time Since Randomization (Hours) 88 96 30-Day Secondary Efficacy Results Routine Early Eptifibatide Delayed Provisional Eptifibatide OR (n=4722) (n=4684) (95% CI) P Death or MI 11.2% 12.3% Death 2.8% 2.6% 1.10 (0.86-1.41) 0.46 13.8% 0.89 (0.79-1.01) 0.065 Death, MI, RIUR 12.5% 0.89 0.079 (0.79-1.01) MI, myocardial infarction; RIUR, recurrent ischemia requiring urgent revascularization Kaplan-Meier Curves for 30-day Death or MI Death or MI (%) 15 12.4% Delayed provisional eptifibatide 10 11.2% Routine early eptifibatide 5 P = 0.079 (stratified for intended early clopidogrel use) 0 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 Time Since Randomization (Days) 96-hour Primary Efficacy Results Prespecified Subgroups Odds Ratio for Upstream Routine Early Eptifibatide (95% CI) Eptifibatide, % Baseline Characteristic Delayed Provisional Eptifibatide, % Overall 9.3 10.0 Men Women 9.1 9.8 9.7 10.4 Age < 75 yr Age > 75 yr 8.6 11.4 9.5 11.4 Troponin positive Troponin negative 9.5 7.7 10.6 6.8 Diabetes 8.9 10.6 No Diabetes 9.5 9.8 Early clopidogrel intended No early clopidogrel intended 8.8 10.8 9.5 11.5 0.5 0.6 0.7 0.8 0.9 1 Early Eptifibatide Better 2 Delayed Provisional Eptifibatide Better 30-day Death or MI Prespecified Subgroups Odds Ratio for Upstream Eptifibatide (95% CI) Baseline Characteristic Routine Early Eptifibatide, % Delayed Provisional Eptifibatide, % Overall 11.2 12.3 Men 11.4 12.0 Women 10.7 13.0 Age < 75 yr Age > 75 yr 10.2 11.6 14.0 14.6 Troponin positive 11.6 13.0 Troponin negative 8.1 8.4 Diabetes 11.7 13.8 No Diabetes 10.9 11.7 Early clopidogrel intended No early clopidogrel intended 10.3 13.7 12.0 13.4 0.5 0.6 0.7 0.8 0.9 1 Early Eptifibatide Better 2 Delayed Provisional Eptifibatide Better Safety Results (through 120 hours) Routine Delayed Early Provisional Eptifibatide Eptifibatide (n=4686) Bleeding (all patients, %) TIMI major 2.6 TIMI major or minor 5.8 GUSTO severe 0.8 GUSTO moderate or severe 7.6 PRBC transfusion 8.6 Bleeding (CABG) Re-operation for bleeding (%) 6.0 Chest tube output (mL/24 H) 720 Thrombocytopenia (<100K, %) 3.3 Stroke (total, %) 0.6 (n=4643) OR P (95% CI) 1.8 3.4 0.9 5.1 6.7 1.42 (1.07-1.89) 0.015 1.75 (1.43-2.14) <0.001 0.99 (0.64-1.55) 0.97 1.52 (1.28-1.80) <0.001 1.31 (1.12-1.53) 0.001 8.4 770 2.8 0.8 0.70 (0.39-1.27) -1.19 (0.93-1.51) 0.79 (0.48-1.30) 0.24 0.41 0.17 0.36 Small Molecule GP IIb/IIIa Inhibition in NSTE ACS PURSUIT PRISM PRISM PLUS Theroux PARAGON B PARAGON A COMBINED 1998 (n = 23,967) 0.88 (0.79-0.97) ACUITY Timing EARLY ACS 0.25 0.92 (0.82-1.01) EARLY ACS + ACUITY 0.89 (0.84-0.95) COMBINED 2009 (n = 42,666) 0.50 1.0 2.0 Odds Ratio for 30-day Death or MI Relative to Control 4.0 Conclusions Among high-risk NSTE ACS patients, a strategy of routine, early eptifibatide compared with delayed, provisional eptifibatide at PCI did not significantly reduce the primary composite of death, MI, RIUR, or TBO at 96h resulted in a trend toward reduction in death or MI at 30 days, but no difference in 30-day mortality resulted in higher rates of non-life-threatening bleeding and transfusions Implications The results of EARLY ACS do not support a strategy of routine early eptifibatide use in high-risk NSTE ACS patients managed with an invasive strategy If subgroups of patients with high likelihood of benefit and low bleeding risk could be identified, it might be reasonable to consider early eptifibatide use in selected high-risk NSTE ACS patients who are intended to undergo angiography Available Today at www.nejm.org EARLY ACS Steering Committee Australia P. Aylward New Zealand H. White Austria K. Huber Norway D. Atar Canada M. Labinaz, A. Langer, J-F. Tanguay Poland W. Ruzyllo Czech Rep P. Widimsky Portugal M. Carrageta Denmark P. Grande Russia V. Sulimov France G. Steg Spain A. Betriu Germany C. Bode, U. Zeymer South Africa A. Dalby Hungary M. Keltai Switzerland F. Mach India D. Prabhakaran United Kingdom K. Fox, K Karsch Israel B. Lewis United States B. Gibler, N. Kleiman, H. Herrmann, J. Hochman, J. Hoekstra, M. Ohman, W. O’Neill, C. Pollack, M. Schweiger Italy D. Ardissino Netherlands A. van ‘t Hof Back-up slides Strategy During First 96 Hours CABG (N=268) Pre-CABG Events = 33 Post-CABG Events = 52 PCI (N=2723) Pre-PCI Events = 87 Post-PCI Events = 243 Total Events on Medical Treatment = 71 + 82 +33 Events Risk Medical 186 4718 Post PCI 201 52 Post CABG CABG (N=251) Pre-CABG Events = 22 Post CABG Events = 46 Medical Only (N=1706) Total Events = 71 PCI (N=2666) Pre-PCI Events = 82 Post-PCI Events = 201 Group N=3490 N=5389 N=519 Delayed Provisional Eptifibatide (N=4680) Total Events = 469 Early Eptifibatide (N=4718) Total Events = 439 Medical Only (N=1784) Total Events = 71 Medical Only PCI CABG Randomization N=9406 Rate Total Events on Medical Treatment = 71 + 87 + 22 Group Events Risk 4.1% Medical 180 4680 4.0% 2584 8.0% Post PCI 243 2636 10.5% 235 23.4% 46 229 20.6% Post CABG Rate Primary and Key Secondary Efficacy Results By Clopidogrel Strata at Randomization Routine Early Eptifibatide Delayed Provisional Eptifibatide OR (95% CI) 96-hr Death, MI, RIUR, TBO Clopidogrel intended 8.8 No Clopidogrel intended 10.8 9.5 11.5 0.92 (0.78-1.08) 0.93 (0.72-1.20) 30-day Death / MI Clopidogrel intended No Clopidogrel intended 12.0 13.4 0.85 (0.73-0.91) 1.03 (0.81-1.31) 10.3 13.7