Communicating Changes in Condition: Using the SBAR tool
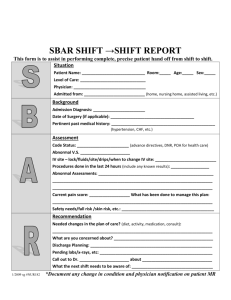
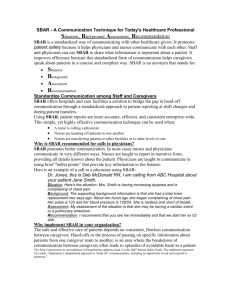
advertisement
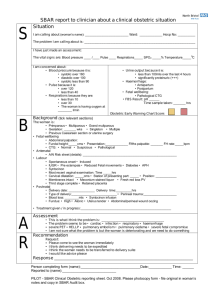
This transcript is intended to provide webinar content in an alternate format to aid accessibility. We apologize for any inaudible or unclear content as a result of audio quality. Communicating Changes in Condition: Using the SBAR tool Presented by: Kristi Wergin (30-minute Webinar) [9/24/2013] Candy Hanson: Hi everybody, this is Candy Hanson with Stratis Health, the Quality Improvement Organization in Minnesota and also the program manager. I want to welcome you to this educational session. This session is being recorded and will be available on the Stratis Health website at StratisHealth.org. Our featured guest speaker is Kristi Wergin, a program manager at Stratis Health. She provides quality improvement leadership for Minnesota Nursing Homes as part of the Centers for Medicare and Medicaid Services Quality Improvement Organization contract. Currently, she’s leading a team effort that is helping about 170 Minnesota Nursing homes in their quality improvement efforts, as part of the Acting Together to Improve Excellence. Kristi has over 30 years experience as a registered nurse with specific background in elder care, which includes direct resident care as a nursing assistant and staff nurse, as well as work in quality improvement, staff development, leadership, management and customer/employee satisfaction. She had the opportunity to receive the interact training at the INTERACT Institute in January of 2013, and has been providing training in the use of the INTERACT tools to nursing homes, participating in care transitions work with Stratis Health. Please welcome Kristi Wergin. Kristi Wergin: Thank you Candy. In your work to improve transitions of care, you’ve all learned about the importance of good communication within your homes, as well as between settings of care. SBAR, which stands for Situation Background Assessment & Recommendation, is a tool designed to improve communication. At the conclusion of this webinar… You should be able to describe the purpose of the SBAR communication form and change and condition progress note, Describe each section of the SBAR, and Be able to answer frequently asked questions that will help you implement the use of SBAR in your home We will be looking at the INTERACT SBAR tool, which I’m sure some of you are familiar with, so bear with us and maybe at the end you’ll have some things you can share with us about using this tool. The INTERACT SBAR tool was developed as part of the INTERACT program and INTERACT stands for Interventions to Reduce Acute Care Transfers and it is a quality improvement program that focuses on the management of acute change in resident conditions. It includes clinical and education tools and strategies for use in everyday practice in long-term care facilities. Stratis Health | 952–854-3306 | www.stratishealth.org Page 1 One in four patients admitted to a skilled nursing facility are readmitted to the hospital within 30 days. Such transfers can result in numerous consultations of hospitalization and billions of dollars in unnecessary healthcare expenditures. The goals of INTERACT are: To improve care, To improve the management of residents with a change in conditions, Reduce the frequency of potentially avoidable transfers to the acute hospital The INTERACT tools are free to use and can be accessed at http://INTERACT2.net/, which is on the slides. Nursing homes can safely reduce hospital transfers… By preventing conditions from becoming severe enough to require hospitalization through early identification and assessment of changes in resident condition, By managing some conditions in the nursing home without transfer when feasible and safe, or By improving advanced care planning and the use of palliative care plans when appropriate as an alternative to hospitalization for some residents. The INTERACT Program has four categories of tools to address these three points. 1. 2. 3. 4. Quality improvement tools Communication tools Decision support tools Advanced care planning tools SBAR is one of the communications tools. INTERACT tools are meant to be used together in your daily work in the nursing home. Here is an overview of INTERACT tools. The INTERACT tools are listed in the blue boxes in the first and third columns of the slide overview. The center column shows the steps that occur as the resident is admitted to the nursing home and has a change of condition. You can see where each tool comes into play as the change of condition is recognized and acted upon. The SBAR form and progress note is used to notify the physician or physician extender of a change in condition. I may say physician a lot, but whenever I say physician I’m referring to the physician, nurse practitioner, physicians assistant, any kind of position extender. It can also be used to share information about a resident during transition such as communicating with the hospital as part of the transfer process. As I mentioned before, SBAR stands for Situation Background Assessment & Recommendation. It is a communication tool whose purpose is: To improve communication with a change in resident condition, To guide the nurse to use consistent language when sharing information about a resident, Standardized criteria that’s important to share when a change of condition is noted, and To provide a framework that has clear guidelines about what information to share in an efficient and effective manner Stratis Health | 952–854-3306 | www.stratishealth.org Page 2 In addition to improving communication between nurses and physicians when there’s a change of condition, nurses that learn to communicate using SBAR guidelines will find the communication between staff, such as during shift reports, as well as across setting of care is also improved. To get you all familiar with this tool we will look at it one section at a time. Before completing the form and calling the physician, nurse practitioner or physicians assistant, it’s important that you gather information. At the top of the form there are items to check off to remind you of the information you should review and collect prior to making the call. You should collect information about: Vital signs Progress notes Recent labs and orders When assessing the resident before the call, you might want to use the INTERACT care plan or INTERACT acute changing condition file card, which if you aren’t already using might be something you want to check into. They are a great help in completing the assessment. Make sure you have all the relevant information prior to your call and don’t forget about advanced directives, allergies, and medications. The checkbox reminds you of what you should have available when you make your call. The first section of the SBAR form is the S, which stands for situation. When communicating information about a resident it is very important that you present a clear and concise explanation of what you are seeing. Let’s say for example that you notice one of your residents has had a change in mental status. Instead of waiting till the resident presents with further symptoms, it would be best to call the physician to inform them about the change of condition, when it was first noticed, if it has gotten worse, better or stayed the same since being noted. Also, don’t forget to share if there are things that make the symptom better or worse, and if the resident has had this symptom in the past. If this is a recurring problem, check to see what was done last time to treat the symptom. If something worked in the past then suggest that as a treatment. If it wasn’t helpful then it’s important to share that as well, in order for the resident to receive effective treatment as soon as possible. Next is B, which stands for background. This section allows you to provide context to the situation you find in the first section. Be sure to include whether the resident you’re calling about is at your home for post acute care or long-term care. Include the primary diagnosis, as well as other pertinent history. For example, if you’re calling about a resident that has acute methyl changes you may want to share that their primary diagnosis is dementia. Other pertinent history may include that they haven’t eaten or drank for the past day, maybe has increase confusion, and by that give specific examples of what you mean, and they have perhaps decreased urine output and foul smelling urine. Also include important medication information. For example, it’s important to indicate if the resident is on 9:18, if you’re getting an order for an antibiotic. It’s best to share this information now so you don’t have to call the doctor later for orders to check INRs while being treated for the antibiotic or worse, if you don’t want to have to call up an adverse drug event because INRs weren’t monitored while the resident was being treated with the antibiotic. Stratis Health | 952–854-3306 | www.stratishealth.org Page 3 It’s also important to have vital signs ready when you call. There’s nothing worse than being asked for this information and not having it. As I heard one physician comment, they’re called vital signs for a reason. Not having this basic information may make you lose your credibility and/or the physician may order a transfer due to his lacking confidence in you. Next and still part of the background section is a list of check off items. This section contributes to the length of the tool; however, it’s easy to complete and it helps you make sure you’ve given thought to all clinical issues before contacting a physician. This list includes information about: Change in a residents mental status Functional status Respiratory system GI system, and/or Urinary changes If there are no changes in some or all of these areas leave the section blank and go to the next section. It’s really designed to be a quick way to review the systems, make sure you’ve thought about it and that you share any changes with the physician relative to any of those different systems. The final question for the background part of the SBAR form directs you to check for recent lab results and any advanced care planning and/or resident family preference for care and information that may be pertinent. When completing this section you may find that you do not have recent advanced care planning information. This should prompt you to look at updating systems in your home to ensure these directions are always up to date. As I mentioned earlier there are several INTERACT tools that you may want to reference related to advanced care planning. The next section is A, which is for assessment or appearance. Here’s your change to share what you think is going on with the resident. Generally when making a call to a physician you have a pretty good idea of what might be going on. You may often know this resident very well and/or have seen the presenting symptoms many times in your work. Don’t be afraid to share what you’re thinking. That’s the only way you’ll get what you’re hoping for. Providing this assessment is certainly part of the recently updated Minnesota Nurse Practice Act, which calls for RNs to provide a comprehensive assessment of the health status of a patient through the collection, analysis and synthesis of data used to establish a health status baseline and plan of care, as well as address changes in a patient’s condition. This is right out of the nurse practice act. It’s also in the scope of practice for an LPN in Minnesota, whose called on to conduct ‘a focused assessment of a health status of an individual patient through the collection and comparison of data to normal findings and the individual patient’s current health status, and report changes and responses to interventions in an ongoing manner to a registered nurse or appropriate licensed healthcare provider for delegated or assigned tasks or activities.’ There are always questions about whether or not an LPN can make an assessment and as you read in the nurse practice act, it’s not only okay but it’s required. Don’t be afraid to. You’re simply giving your assessment from the information you’ve gathered. The next section is R, which is your chance to request what you want. Stratis Health | 952–854-3306 | www.stratishealth.org Page 4 If you feel you’re able to care for this resident in your facility let the physician know. Some examples of requests you might have might include: Perhaps the physician doesn’t know you can provide IVs at your home. This is an opportunity to let them know that, if that’s something that’s appropriate. Maybe you think it’s important to do some more evaluation before transferring the resident. Don’t be afraid to ask for x-rays, labs orders, Perhaps the resident has an O2 stat in the 70s, but the resident wants comfort care only. Let the physician know and ask the physician for a comfort care or hospice order. Maybe the resident has an O2 set in the 70s and they’re full code. In that case you want to ask for an order to transfer them to the hospital if it’s an emergency. So, if you have some direction in your head before making the call, and again gathering all the information on the SBAR helps lead you in that direction, it’s much more likely that you’ll be providing care that’s in the best interest of the resident. The SBAR tool is pretty straightforward, I think you’ll all agree, and many of you I’m sure if you did it will find out it’s not rocket science. As you’re teaching staff to use the SBAR and encouraging them to get on board and everybody to consistently use this tool, sometimes there are a lot of questions that come up about the tool, so I want to provide you with some answers to those questions in order to help you out as you’re trying to encourage the use of this tool. One is that it’s going to take so long. You look at it, it’s a lot of pages and it’s like oh my goodness, I know all this stuff why do I have to write it down. You might hear that and a way you can respond is to say try it out if you’ve never used it in your home before. Find a champion, someone who’s excited about using it, on one unit, one day, one nurse on one shift and time it to see how it works. You may have to make some changes based on the experiment or PDSA, but let the staff know then how long it really takes and it might avoid redundancy. It might take the place of other things you’re doing also. Remind the staff about the time it takes to make several calls to the physician if you don’t have all the information in the first place or what about the time it takes to complete an admission to the hospital, maybe you can avoid some of these time consuming admissions if you don’t send them to the hospital to begin with. Another question is… what about all the check boxes. These check boxes were added in INTERACT three, so I don’t think they were available on the INTERACT two SBAR form, so this is recently updated. The check boxes are helpful. They also make it longer which is why I think people ask about it. They are helpful to guide the nursing assessment. They structure the primary care clinician communications. They help reduce the potential for illegible notes and they are also important for electronic health records. If you have an electronic health record or if you’re working on that down the line, you can find if you have check boxes you can grab information much easier from that and use the DHR in your quality improvement efforts. They are also a quick way to get important information because it reminds you somewhat of what you should be looking at. What about the A section? That’s the assessment, there are always lots of questions about can we really do this? You’ll notice on the tool that the RNs and LPNs are a different line for assessment, and that’s because it’s kind of state specific. I think we’re ahead of the curve in Minnesota as far as spelling out what LPNs can do, but it’s not always clear. Sometimes there are more limitations in other states. Stratis Health | 952–854-3306 | www.stratishealth.org Page 5 As I said before, some nurses are uncomfortable making suggestions to physicians, but as I previously mentioned this is certainly within the scope of the Minnesota Nurse Practice Act for RNs and LPNs. We’re actually required to do it, and we’re good at it so we might as well share that information. Then there’s the question of… every single time I call the doctor do I have to use this, every time, for everything? No. Some seem all out of balance about the length of the form because they think you have to use it every time you call the physician, but it’s just designed to share a change in a resident’s condition. So if you’re just making a routine call to the physician for things like lab results, etc. that doesn’t require the use of an SBAR form. However, it’s a great format to consider as a guide to progress notes, regarding changes in a resident’s condition orders or in a care plan. Some people choose to make this part of the record, it’s just up to the individual nursing home, as to whether they want to make this a nursing note and put it in the record. I was hoping to share a video but it’s not working with the webinar setup. I wanted to share a link to a 10 steps SBAR video that’s good and short. It’s a link for those of you who might want to see a short video showing a good example of a nurse using an SBAR in a nursing home to report a change in a resident’s condition to a physician. It’s a good example and may be helpful to the staff. I encourage you to look at that and if you have a meeting and can bring that up to share with your staff to show them, sometimes it’s easier than talking about it. That’s it. Candy Hanson: This concludes our webinar and we have about five minutes for questions and I’ll start, I have two. In the background part of the INTERACT 3 tool where you have check boxes for what appears to me to be signs and symptoms and then underneath each one it says describe signs or symptoms. You’ve already checked them there so what does that mean? Kristi Wergin: I think if you want to be any more specific if it’s out of the norm you can make a note. Perhaps what you want to say isn’t in a check box this gives you a chance to add to that. It’s not required. Candy Hanson: I think it’s an important point, because as nurses we sometimes have difficulty because we try to say too much and this is meant to be a brief summary type tool to use. Kristi Wergin: An example might be like under mental status change, if you check increased confusion you might want to get a little more specific. What are you seeing? That might be helpful, if you say they’re more confused. You might want to say, you know, usually every other day when we go in there right away when the daughter comes he/she always recognizes the daughter and today they didn’t know who they were. Candy Hanson: My second question is this. How are the physicians assistants and NT made aware of the INTERACT? Is it common that most of them in the state of Minnesota are familiar with it? Kristi Wergin: That’s a good question but I can’t make that statement as to whether they’re familiar, I just know the communities we’ve worked with through the care transitions work, the physicians are not only aware of it but they appreciate it and usually give kudos if you call and use the SBAR. They’re usually thankful. Stratis Health | 952–854-3306 | www.stratishealth.org Page 6 Candy Hanson: That’s what we’ve seen in our project as well, so perhaps if there are any other questions or maybe you could share how you’re using the SBAR tool if you are currently and how your physicians respond to it. Are there any additional questions or comments? Kristi Wergin: Does anyone have it as part of their EHR, like it’s in your system? Natalie: In Nosh City we have SBAR in our electronic health. Candy Hanson: How does that work? Natalie: It’s working better now that we’ve done some more training on what we actually want in the spots, because it’s less directed here. It’s just the boxes. We had to do some training on what we want in those boxes. Candy Hanson: I think that’s an important point, to make that that’s a decision you might want to make for your facility. Do you want to guide your clinical staff on what type of data you want to use for communicating with your physicians. Natalie: We actually use an INTERACT SBAR tool, but we don’t make them fill out the paper forms, they just have to use that as a guide for, you should have this information when you call the doctors or whoever you need to call. Then they can use it as a guide for how to chart in the SBAR spot on the PCC. Kristi Wergin: So it’s like a template. Natalie: Yes. Candy Hanson: You use it as a template as you’re communicating verbally with your physicians? Natalie: Correct. Candy Hanson: Thanks that’s great. Does anyone else have anything to share? As I mentioned in the communication, this session is recorded and we’re hoping it will be useful to you as an ongoing training and orientation resource with your staff. We will also send you an evaluation link and would appreciate your feedback. We will now conclude the webinar. Thank you for joining us. This material was prepared by Stratis Health, the Quality Improvement Organization for Minnesota, under a contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the US Department of Health and Human Services. The contents presented do not necessarily reflect CMS policy. 10SOW-C7-13-132 102213 Stratis Health | 952–854-3306 | www.stratishealth.org Page 7