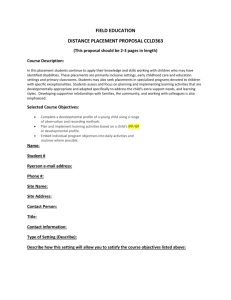
practice education physiotherapy programme
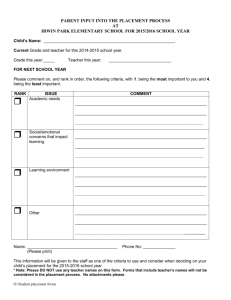
advertisement

School of Rehabilitation Sciences BSc (Hons) and MSc Physiotherapy (pre-registration) Practice Education Programme Physiotherapy Practice Educator and Student Handbook Academic Year 2015-16 Mary Jane Cole Senior Lecturer Physiotherapy Practice Education Practice Placement Co-ordinator Tel: +44 (0) 20 8725 2250 Mob: 07900525054 Email: m.cole@sgul.kingston.ac.uk Alison Jones Senior Lecturer Physiotherapy Practice Education Practice Placement Co-ordinator Tel: +44 (0) 20 8725 0819 Email: a.jones@sgul.kingston.ac.uk Faye McGill Programme Administrator Tel: +44 (0) 20 8725 0124 Email: placementteam@sgul.kingston.ac.uk Table of Contents: Sections highlighted in green are recommended to Practice Educators if pressed for time. Welcome.......................................................................................................................... 3 BSc (Hons) Physiotherapy............................................................................................... 5 Course Philosophy ....................................................................................................... 5 Course Aims ................................................................................................................ 5 Overall Course Learning Outcomes ............................................................................. 6 BSc (Hons) Physiotherapy Modules ............................................................................ 7 MSc Physiotherapy (pre-registration) .............................................................................. 9 Course Philosophy ....................................................................................................... 9 Course Aims ................................................................................................................ 9 Overall Course Learning Outcomes ........................................................................... 10 MSc Physiotherapy (pre-registration) Modules .......................................................... 11 Clinical Skills.................................................................................................................. 13 BSc (Hons) Physiotherapy ......................................................................................... 18 MSc Physiotherapy .................................................................................................... 18 Peer Assisted Learning (PAL) .................................................................................... 19 BSc Physiotherapy ................................................................................................. 19 MSc Physiotherapy ................................................................................................ 20 Accountability ......................................................................................................... 20 Responsibilities ...................................................................................................... 20 Practice Education Module Descriptors ......................................................................... 26 Year 2 BSc (Hons) Physiotherapy Practice Module ................................................... 26 Year 1 MSc Physiotherapy (pre-registration) Practice Module................................... 26 Year 3 BSc (Hons) Physiotherapy Practice Module ................................................... 33 Year 2 MSc Physiotherapy Practice Module .............................................................. 33 Roles and Responsibilities............................................................................................. 38 Role of The Practice Educator ................................................................................... 38 Role of the Link tutor .................................................................................................. 42 Role of the Practice Placement Co-ordinator ............................................................. 42 Assessment ................................................................................................................... 43 Practice Placement Assessment Form ...................................................................... 43 Student Supervision ................................................................................................... 44 Learning Contract ...................................................................................................... 44 1 The Midway Assessment ........................................................................................... 45 Practice Portfolio ........................................................................................................... 48 Placement Problems / Issues ........................................................................................ 50 The Failing Student .................................................................................................... 50 Danger of Failure form............................................................................................ 51 Safety on Placement .................................................................................................. 52 Universal Precautions .................................................................................................... 57 Personal Property .......................................................................................................... 57 Security.......................................................................................................................... 57 Student Consent To Act As A Model For Teaching Sessions ........................................ 58 Additional Requirments On Placement .......................................................................... 58 Practice Placement Hours ............................................................................................. 59 Student Absence During Practice Placement ................................................................ 61 Submission Of Assessment Form ................................................................................. 62 Equal Opportunities ....................................................................................................... 63 Disability Support ....................................................................................................... 64 Administration Of Placements ....................................................................................... 66 Practice Educator Study Days ....................................................................................... 67 Travel, Claims And Other Relevant Documentation ...................................................... 69 e-Appendicies are available at: http://www.healthcare.ac.uk/schools/rehabilitation-sciences/practice-resources/ 2 Welcome Dear Practice Educator and Students, Welcome to the practice education programme for BSc (Hons) Physiotherapy and MSc Physiotherapy, Kingston University/St. George’s University of London. The practice education element is a key part of both courses. Practice based learning gives students the opportunity to consolidate knowledge, apply theory and enhance skills. Practice education facilitates transitional learning and ensures that all students practice physiotherapy safely and competently. This handbook is designed to provide the information necessary to make practice based education a valuable and worthwhile experience for all concerned. It includes: An overview of both curriculums An overview of course programme modules An overview of roles and responsibilities of the student and supporting staff while on placement Strategies to support learning in the clinical setting Practice placements are often the highlight of a student’s physiotherapy course and the greatest strength of a practice placement is the patient contact offered and the support provided by the Practice Educator. The practice components of both physiotherapy programmes are very similar and differences are highlighted throughout the document. Students on both programmes of study undertake observational Peer-Assisted-Learning clinical practice visits (PAL Clinical) and complete six five-week placements. The Practice Education Team monitors every student’s profile ensuring that each individual gains clinical experience where practically possible with clients across the age range and within a variety of settings including neurological, musculoskeletal and cardio respiratory conditions and to reflect pathways of care. Each clinical environment is unique and offers students different insights and experiences. Students differ considerably; some students may require more support whilst some may achieve more during one practice placement than in another. The Visiting / LinkTutor can assist the Practice Educator and the student in making the most of the opportunities provided by the placement. All students are assessed on placement via the common assessment form (see eAppendix 3 http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-forpre-registration-physiotherapy-practice-educators/ ). All students are expected to pass each placement in turn before proceeding to the next placement. While the BSc student’s final grade/ mark contributes to their degree status, the MSc students do not receive credits for their placements. Students are expected to read and be familiar with the content of the handbook and should be able to access it throughout their placements. We encourage the student and the Practice Educator to take advantage of the information provided in this booklet so that both can make the most of the practice education programme. 3 Should you have any comments or queries about the content of this handbook please feel free to contact the Practice Education Team at the School of Rehabilitation Sciences. All feedback is important and is valued. Thank you for your on-going support for the practice education programme and St George’s, University of London/Kingston University. Yours Sincerely Mary Jane Cole Senior Lecturer Physiotherapy Practice Education Practice Placement Co-ordinator Alison Jones Senior Lecturer Physiotherapy Practice Education Practice Placement Co-ordinator 4 BSc (Hons) Physiotherapy Course Philosophy Students graduating from the BSc (Hons) Physiotherapy programme will be safe, competent, autonomous, reflective practitioners equipped with the knowledge, understanding and skills to apply a person-centred approach to physiotherapy. They will be eligible to apply for registration with the Health and Care Professions Council (HCPC) and for membership of the Chartered Society of Physiotherapy (CSP). A range of teaching activities will promote independent learning skills, including fostering intellectual curiosity, as well as developing the awareness of self and others necessary to be an effective team worker in healthcare, research and the broader community. The course will promote an understanding of professional identity that includes multi-disciplinary working and modernisation of healthcare roles. Concordant with this, is an attitude to professional practice that embeds continuing professional and personal development. The emergent professional will have an understanding of the social and political context in which they will practice and a strong sense of professional scope of practice in accordance with the HCPC standards and CSP code of professional values and behaviour. Ultimately graduates will demonstrate responsibility and accountability to service user and service needs. It is paramount that physiotherapists have good communication skills in order to build effective partnerships with service users and carers and deliver interventions effectively. It is also important that physiotherapists have other skills not specific to physiotherapy including adaptability, critical reflection and problem solving. In addition, graduates will be conversant with emerging policy and guidelines and demonstrate a critical approach to applying evidence to meet the needs of individuals and populations. They will also be able to demonstrate responsible assertiveness and possess entrepreneurial and management skills, which are essential to the modern physiotherapist in the changing climate of healthcare provision. The course philosophy recognises that to be effective, undergraduate physiotherapy education must support students’ acquisition of core physiotherapy skills as well as the key skills outlined above, which are transferable to a range of personal and professional situations and settings. This will, in turn, facilitate a seamless transition from the academic learning environment to evidence-informed healthcare practice in a wide variety of settings. Course Aims In accordance with the aims of the Faculty of Health, Social Care and Education, the Health and Social Care Professions (HCPC) Standards of Education and Training (SETs) and Standards of Proficiency (SoPs) and the Chartered Society of Physiotherapy (CSP) Learning and Development Principles this course aims to: Develop professional knowledge, understanding, skills and behaviour, in order to work as an effective, autonomous physiotherapist Promote communication skills such as listening, empathy and sensitivity to engender a caring person-centred approach to physiotherapy practice 5 Foster critical thinking, reflection, and skills of self-directed learning for lifelong personal and professional development Enable graduates to respond to changing political and societal contexts, to provide services which meet the needs of individuals and populations Inspire a responsibility to promote excellence within the Physiotherapy Profession and across disciplines Overall Course Learning Outcomes On successful completion of the course the students will be able to demonstrate achievement of the following learning outcomes: Apply principles, concepts, practice and communication skills essential for safe and effective person-centred physiotherapy practice in a variety of settings Plan and implement a variety of treatment plans in collaboration with patients/carers using a flexible and comprehensive clinical reasoning framework Identify his/her individual learning needs to promote lifelong learning through independent study and self-evaluation Demonstrate critical insight into management concepts necessary to meet the changing needs and demands of variable health and social care environments Critically analyse and evaluate literature and clinical experience to inform practice Apply academic and reflective skills to communicate and work with professional colleagues to provide person-centred health care The learning outcomes for each of the 3 years of study are noted in the relevant section below The course curriculum is detailed in e-Appendix 1 at http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ 6 BSc (Hons) Physiotherapy Modules Module Code PT 4001 PT 4002 PT 4003 PT 4004 PT 2009 PT 2010 PT 2011 PT 2013 PT 2014 PT 2015 PT 3007 PT 3009 PT 3010 PT 3011 PT 3015 Module Title Interprofessional Foundation Programme Assessment, Structure and Function Pathology, health promotion and rehabilitation Factors Influencing Professional practice Management of people with Musculoskeletal Dysfunction Management of Complex Cardiorespiratory Dysfunction Neurological Rehabilitation Research Methods in Health and Social Care Integrating Clinical Concepts Practice Placements 1,2,3 Physiotherapy Practice in Context Research in Practice Interprofessional Debates/Management Critical Reflection and Reasoning Practice Placements 4,5,6 Level 4 Credits 30 4 30 4 30 4 30 5 30 5 15 5 5 15 15 5 4,5 6 30 15 30 6 6 30 15 6 15 6 30 Integration between the School-based modules and practice placements is of paramount importance and is addressed in the module delivery of this course. All module descriptors are available in e-Appendix 1 at http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ 7 Week Year 1 Practice Education Handbook 2013/14 Year 2 CR ICC NR ASF FIPP IFP 6 7 8 Mar Apr May June July PP 1 Pre clini cal CRR Term Break RP PIC Year3 IDM CRR RP PIC ASF FIPP PHPR PP 2 Study Week PP 5 Term Break Pre clinical yr 2 PP 4 Year 3 PIC Physiotherapy in context RP Research Project CRRCritical reflection and reasoning IDMInterprofessional debates and management PP Clinical placements 4,5,6 CR ICC NR MSK RM P FIPP A L ASF IFP 30 30 15 15 30 FIPP PHPR CR ICC NR MSK RM P A L RP PIC 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 Feb Term Break Year 1 Credits IFP Interprofessional foundation programme 30 ASF Assessment structure and function 30 PHPR Pathology, Health Promotion and Rehabilitation 30 FIPP Factors influencing Physiotherapy practice 30 Year 2 ICC Integrating Clinical Concepts 30 MSK Management of Musculoskeletal disorders 30 NR Neurological Rehabilitation 15 CR Management of complex cardiorespiratory conditions15 RM Research Methods 15 PP Practice placements 1,2,3 15 5 Jan Term Break CRR 4 Term Break MSK RM 3 Dec Term Break PP 2 Nov Revision RP PIC 1 SepOct BSc (Hons) Physiotherapy Indicative Course Plan 15/16 Indicative Course Plan, BSc (Hons) Physiotherapy Practice placement blocks (PP1-6) shown in green Exams PP 3 PP 6 ________________________________________________________________________________ 8 MSc Physiotherapy (pre-registration) Course Philosophy Students graduating from the MSc Physiotherapy (pre-registration) programme will be competent, autonomous practitioners equipped with the knowledge, understanding and skills to apply a person centred approach to physiotherapy. They will be eligible to apply for registration with the Health Professions Council (HPC) and membership of the Chartered Society of Physiotherapy (CSP). Blended learning and teaching activities will promote independent learning skills, including fostering intellectual curiosity, as well as developing the awareness of self and others necessary to be an effective team worker in health and social care, and research. The course will promote an understanding of professional identity that includes interprofessional working and modernisation of healthcare roles. Concordant with this, is an attitude to professional practice that embeds continuing professional and personal development. The emergent professional will have an understanding of the ethical, political and societal contexts in which they will practice and a strong sense of professional identity. Graduates will develop advanced critical skills which include the examination of differing perspectives, beliefs and theories. It is important that physiotherapists, in addition to core physiotherapy skills, have relevant transferrable skills such as decision making, effective communication, adaptability and critical reflection which will all be emphasised and nurtured. Importantly, graduates will also be able to demonstrate responsible assertiveness and possess entrepreneurial and management skills, which are desirable to the modern physiotherapist. This will, in turn, facilitate a seamless transition from the academic learning environment to evidence informed clinical practice. Course Aims In accordance with the strategic plan of the Faculty of Health and Social Care Sciences, this course aims to ensure graduates: Develop relevant knowledge, understanding, skills, and professional behaviour in order to work as a safe, effective, autonomous physiotherapist Promote empathy and sensitivity to engender a person centred approach to physiotherapy practice Respond to changing political and societal contexts, in the delivery of effective, safe services which meet the needs of individuals and populations Develop a critical awareness and systematic understanding of research methods used in health and social care research Develop effective interprofessional working and enhance service delivery Critically evaluate their effectiveness in relation to the delivery of person centred physiotherapy ________________________________________________________________________________ Practice Education Handbook 2013/14 9 Overall Course Learning Outcomes On completion of the programme the participant will be able to: Apply principles, concepts and skills essential for safe, competent and autonomous physiotherapy practice in a variety of settings Plan and implement a variety of prevention and treatment plans using a flexible and comprehensive clinical reasoning framework Demonstrate advanced critical thinking in the approach to the practice of physiotherapy in order to make decisions on the choice and effectiveness of interventions for individuals and groups in the context of the changing needs and demands of variable health and social care environments Demonstrate advanced research skills in implementing an independent research project which is relevant to physiotherapy practice within Health and Social Care Evaluate and synthesise the factors influencing interprofessional working in physiotherapy practice including those factors which may influence successful team working and person-centred programmes of care Demonstrate independent study and self-evaluation, decision-making, leadership, self-responsibility and advanced personal strategies for lifelong learning including evidence of reflective practice Apply and critically evaluate effective communication skills for shared decision making and team working Illustrate and critically evaluate innovative, evidence based, person-centred interventions ________________________________________________________________________________ Practice Education Handbook 2013/14 10 MSc Physiotherapy (pre-registration) Modules Prerequisite Year 1 Module title Essentials of physiotherapy Management of Musculoskeletal Dysfunction Management of Complex Cardiorespiratory Dysfunction Neurological rehabilitation Level 4 5 15 5 15 5 Evaluation of Reflection in Rehabilitation 15 7 Psychology for Exercise for Health 15 7 None 4/5 Physiotherapy in context 30 30M/90(tot) 7 Interprofessional Debates and Management Professional Development in Rehabilitation Research Project 15 7 15 7 60 7 Self-Management in people with long term and neurological conditions 15 7 None 6 Clinical placements Year 2 Credits No credits – level 4 catch up module 30 Clinical placements 135M The course curriculum is detailed in e-Appendix 2 at http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ ________________________________________________________________________________ Practice Education Handbook 2013/14 11 Indicative Course Plan, MSc Physiotherapy Practice placement blocks shown in blue ________________________________________________________________________________ Practice Education Handbook 2013/14 12 Clinical Skills The following tables provide an overview of the principal clinical skills that Physiotherapy students have studied, and been examined upon, during both BSc (Hons) Physiotherapy and MSc Physiotherapy programmes. Clinical skills developed and assessed prior to Level 4 (1) Placement Module Skills Interprofessional Foundation Programme (BSc) Factor Influencing Professional Practice (BSc) Assessment, Structure and Function (BSc) Basic life support Hand hygiene BMI Vital signs - temperature, pulse and respiration Peak flow Blood pressure Urine and glucose testing Glasgow Coma Scale (not tested) Communication skills o Introduction and closing an interview o Informed consent o Verbal and no-verbal skills to facilitate communication Essentials of Physiotherapy (MSc) Factor Influencing Professional Practice (BSc) Assessment, Structure and Function (BSc) Surface anatomy palpation and location o Finding pulses – carotid, brachial, radial, femoral, posterior tibial, dorsalis pedis o Heart –location of valves and how to use stethoscope to hear values o Abdomen – surface anatomy of major organs (including bladder) o Using percussion to assess abdomen o Location of thyroid, hyoid, trachea o Cranial nerves (anatomy but not tests) Manual handling (preliminary skills) Sit to stand with assist 1 or 2 Walking with assist 1 or 2 Turning or moving in bed with assist 2 Neuromusculoskeletal Pathology, Health Promotion and Rehabilitation (BSc) Essentials of Physiotherapy (MSc) Assessment and Examination Skills Outline of basis for subjective examination Red flags Observation of posture Analysis of functional movement (e.g. gait, sit to stand, reach) Assessment of balance / proprioception (key tasks) MRC muscle testing major muscle groups (e.g. shoulder flexors) Static Resisted testing major muscle groups (not individual muscles) Muscle length tests (key muscles – gastrocnemius, rectus femoris, hamstrings, biceps brachii) 13 Palpation of bony landmarks and soft tissues. AROM – spinal and peripheral PROM – peripheral Goniometry Accessory movements – peripheral AP, PA and long caudad major joints (shoulder, elbow, wrist, hip, knee, talocrural) Spinal accessory – PA, unilateral PA introduction Reflex testing Rehabilitation Communication skills - therapeutic relationship, Goal setting, empowerment Teaching therapeutic exercise – for strength, endurance, stretch, balance and ROM including using a variety of equipment / resources but with particular emphasis on what can be used for home. Active assisted exercise Electrotherapy modalities – Hot/Cold therapy, US, PSWD, Electrical Stimulation, TENS, Interferential Soft tissue techniques – massage and deep tendon frictions. Neurology Assessment and Examination Skills Observation of posture Analysis of functional movement (e.g. gait, sit to stand, reaching) Assessment of balance, standing and walking Rehabilitation PNF Improvement of balance Re-education of functional tasks, using a task specific training approach, e.g. rising to stand, reaching to grasp Management of dizziness and vestibular dysfunction Cardiorespiratory Assessment and Examination Skills Auscultation and surface lung-heart and pleura marking Normal and added breath sounds Lung function tests –interpretation Lung volumes and capacities Arterial blood gases (basic principles and interpretation) Interpretation of investigations such as BP/HR/SaO2 Assessing correct use of meter dose inhalers Peak expiratory flow meters (PEF) Chest X-rays (basic principles) SOAP notes Field walking tests Complete respiratory assessment The oxygen dissociation curve and common oxygen delivery systems Assessment of dyspnoea Basic risk assessment in post-operative patients (in year 2, term 2) 14 Integrating Clinical Concepts (BSc) Evaluation of Reflection in Rehabilitation (MSc) Rehabilitation Breathing control and implications for work of breathing Positioning for reducing WOB, V/Q mismatch, breathlessness ACBT (and ACBT with percussion, vibrations, shaking, use of Cornet, Flutter and PEP) Postural Drainage Rehabilitation of amputees Principles of mobilisation and exercise (such as effects on BP, HR, V/Q) Basic considerations when treating patients with chest drain in situ Pulmonary and Cardiac rehabilitation (year 2, term 2) Exploring the psychological and social aspects of health including how aspects such as communication, relationship with patients and responses to rehabilitation influence outcomes Introduction to clinical reasoning Skills developed and assessed in Year 2 BSc and Year 1 MSc Module Skills Management of Neuromusculoskeletal Dysfunction Neuro-musculoskeletal Assessment and Examination Skills Further development of Patient Screening for practice (Special questions, Red/ Yellow Flags, Cervical Artery, Neurology, Pathology) Special tests – Specific Muscle and Ligament Stability tests Neuro-dynamics – ULNT1, Slump and SLR Passive Physiological Intervertebral Movements (PPIVMs) – Lumbar only Rehabilitation Consideration of different approaches to musculoskeletal practice (e.g. Structure, Function, Myofascial, Neuro-dynamics, McKenzie) Manual therapy skills o Joint physiological and accessory mobilisations, o Integrating techniques, e.g. PNF Hold Relax o Trigger points o Management of Neurological NAG’s, SNAG’s, MWM’s Developed but not assessed Hydrotherapy (introduction to principles) Combining movement Core stability (lumbar spine) Hands and plastics – specialist principles Taping Acupuncture (introduction to principles) Neurology 15 Movement Dysfunction Management of Complex Cardiorespiratory Dysfunction More emphasis is placed on the effects of pathology and rehabilitation strategies. Assessment and examination Effect of pathology on functional activities e.g. ataxia, tone etc Prevention of secondary complications Rehabilitation Self management strategies Re-education of walking Management of ataxia and low tone Management of postural deformity and secondary problems following neurological disorders. Management of Spasticity Management of the upper limb following stroke, mobilisation and support of the shoulder Physiotherapy role in dysphasia, dysarthria and swallowing problems Use of lower limb orthoses Respiratory Assessment and Examination Detailed analysis of objective markers (e.g. blood gases, chest Xrays etc.) ITU charts – how to read them and extract relevant information from them Assessing multi-system failure Assessment of fluid balance Common lines Assessing risk in post-operative patients. Common ITU infusions and effects on respiratory system Rehabilitation Manual inflation Suctioning Bronchial hygiene techniques in self ventilated patients Modes of Ventilation in ITU Weaning from mechanical ventilation Oxygen Therapy Tracheotomy care Pulmonary rehabilitation Non-invasive ventilation Rehabilitation of complex medical patients Ventilation/ perfusion and positioning in complex cases Aspiration assessment and emergency response Effect of different pathologies on the cardio-respiratory system Detailed analysis of objective markers (e.g. blood gases) 16 Skills developed and assessed in Year 3 BSc and Year 2 MSc Neuro-Musculoskeletal Assessment and Examination Skills No additional skills taught / assessed for neuro-musculoskeletal Discussions about how to adapt for different individuals / client groups Neurology No further skills taught but will have considered extra pathologies and current evidence through lectures delivered by clinical experts in related fields e.g. Paediatrics, Learning Disability. Respiratory Considerations for on-call working Please see the module descriptors in e-Appendices 1 and 2 for more information http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ 17 Practice Education Programme BSc (Hons) Physiotherapy The practice based component of the course includes: Four half days on observational Peer-Assisted-Learning clinical practice visits (PAL Clinical) in Year 1 30 weeks of practice based placements. Year 2: 3 five week placements (Levels 4 and 5) Year 3: 3 five week placements (Level 6) A number of physiotherapy practice sessions in university. Total: approximately 1000 hours of clinical practice. (NB. Some international students require evidence of more hours in specified settings) MSc Physiotherapy The clinical and practice based component includes: Two half days on observational Peer-Assisted-Learning clinical practice visits(PAL Clinical) in Year 1 30 weeks of practice based placements 3 five week placements, Levels 4(1) and 5(2) in Year 2 3 five week placements in Year 3, Level 6(3) A number of physiotherapy practice sessions in university. Total: approximately 1000 hours of clinical practice. (NB. Some international students require evidence of more hours in specified settings) 18 Peer Assisted Learning (PAL) Each 1st year student visits a final year student on practice placement. Aims: To give the novice student the opportunity to observe physiotherapy in practice which might include: patient-health professional interactions moving and handling basic physiotherapeutic techniques management and day-to-day running of different clinical services the relevance of psychosocial factors influencing patient management To provide the 1st year student with a clinical context for the theoretical learning To provide the final year student with an opportunity to demonstrate skills in professionalism, communication and management while negotiating the visit and supervising the 1st year student. BSc Physiotherapy: (See course plan). PAL Clinical 1 – 2 separate half day visits (occasionally 1 full day visit) to a 3rd year student during the January placement PAL Clinical 2 – 2 separate half day visits (occasionally 1 full day visit) to a 3rd year student during the May placement. Assessment of PAL 1st year students: Following PAL Clinical 1: Summative assessment in February where the students undertake a 10 minute oral presentation to their personal tutors and peers. The student is expected to: o Discuss the physical, biological and psycho-social factors underlying human health and function, relative to a particular patient they observed during their practice visit o Demonstrate the ability to report findings in a clear and concise manner using appropriate terminology o Begin to demonstrate critical thinking, problem identification and appraisal of information o Analyse specific patient problems and identify basics of physiotherapy skills Following PAL Clinical 2: Formative assessment via a structured reflective account of their PAL clinical experiences (including a personal development plan/ SWOT). Formative assessment relates to critical thinking and reflective skills, linking theory to practice and preparation for professionalism required in clinical practice. Students also receive feedback from their student supervisor in terms of professionalism 3rd year students: Summative assessment of inter-personal and professional skills and clinical reasoning using the level 6 common assessment form 19 MSc Physiotherapy PAL Clinical – 2 half day visits to a final year (MSc) student during the October placement. Assessment 1st year students: No summative assessment but students are asked to reflect on their PAL experience in writing and share this with their personal tutor for formative feedback purposes. In addition final year students provide formative feedback to the 1st year student on professionalism Final year students: Summative assessment of inter-personal and professional skills and clinical reasoning using the level 6 common assessment form Accountability The organisation of the PAL Clinical visits is the joint responsibility of the 1st and final year students (not the responsibility of the Practice Educator). During a PAL visit, the 1st year student is accountable to the final year student who is, in turn, accountable to the Practice Educator. The 1st year student is expected to: Observe student and/ or practitioner in the clinical setting Interact with the patients verbally and/ or have minimal manual contact (e.g. auscultation, feeling chest expansion or passive movement of a limb) Uphold the confidentiality and dignity of the patient at all times during and after the visit Communicate with patients, carers, staff and others as appropriate Access patient documentation and make relevant anonymised notes (in consultation with the final year student and Practice Educator) Wear appropriate clinical uniform and behave in a professional manner at all times Maintain health and safety (e.g. infection control, back-care etc) Adheres to the rules of professional conduct (CSP 2011 and HPC 2008) What the 1st year student cannot do: Assess or treat patients Assist in the moving and handling of patients (specifically patient transfers) without the direct approval and supervision of the Practice Educator Responsibilities The Practice Education Team: Informs the clinical site (via PMP – the Placement Management Partnership) in writing/ email of dates of PAL clinical visits approximately 6 weeks in advance. Allocates PAL clinical visits to 1st year and final year students at least 2 weeks prior to the start of the practice placement 20 Provides 1st year and final year students with guidance and information for the organisation of the PAL clinical visit (including learning outcomes, roles and responsibilities etc) Oversees the PAL clinical visits process and ‘trouble-shoots’ as required Collects and evaluates student and practice staff feedback to monitor the efficacy of this PAL clinical experience The 1st year student: Informs the final year student if they are unable to attend the PAL Clinical visit in good time Makes contact prior to the final year student going on placement (1st year BSc student has prime responsibility for establishing contact for PAL clinical 2) BSc students only: o Initiates discussion with the final year student on an appropriate topic from the practice experience in anticipation of their PAL presentation o Maintains patient confidentiality and dignity in note-taking in preparation for their PAL presentation o Following PAL Clinical 1 delivers a presentation o Is familiar with and plans for the reflective formative assessment before undertaking the 2nd PAL clinical visit i.e. document a SWOT. Receives formative feedback from personal tutor MSc students only: o Is familiar with and plans for reflective formative assessment before undertaking the PAL visit. Receives formative feedback from personal tutor The Final year student: The final year student is accountable to the Practice Educator in ensuring the safety of all persons involved with the clinical observation i.e. 1st year student, patients/ service users If the placement cannot take place as planned, the final year student is responsible for contacting the Practice Educator and the 1st year student to organise an alternative observation Communicates effectively with the 1st year student (final year student has prime responsibility for establishing contact for PAL Clinical 1 BSc and PAL Clinical MSc) Plans for the visit by the 1st year student. This includes selection of appropriate patients/ service users for the 1st year student to observe (demonstrating clear clinical reasoning for the selection to their Practice Educator) and liaison with relevant patients/ carers/ multi-disciplinary team members Communicates effectively with the Practice Educator in planning the visit by the 1st year student (this should start on day 1 of the placement) Completes a local risk assessment prior to the PAL clinical visits and gives it to the Practice Educator Ensures on-going informed patient consent prior to and during the visit (may include discussion with family/ carers/ relevant health care workers) Guides the 1st year student during the visit regarding local health and safety issues (which may include a risk assessment), infection control, use of any equipment etc Supervises the 1st year student during any interactions with patients The final year student can refuse to proceed with the clinical experience if the 1st year student is unprofessional in any way 21 Provides feedback to the 1st year student of their conduct during the visit Facilitates a discussion with the 1st year student to develop an outline for the PAL presentation required by the 1st year student following PAL clinical 1 (BSc) Responds to the discussion initiated by the 1st year student on an appropriate topic for the reflective formative assessment following PAL clinical 2 (BSc) or MSc PAL The Practice Educator: Is aware of upcoming visit (notified by the university Practice Education Team, PMP or by the local practice liaison) Provides feedback to the final year student following the PAL visit via the Level 6 common assessment form Informs the students if they are not performing responsibilities appropriately Discontinues the visit if either student is unprofessional in any way and informs the university Practice Education Team by email or telephone Postpones the 1st year visit if the final year student is not present (i.e. off sick) or if the final year student has not adequately prepared for the visit (i.e. not gaining patient consent) and informs the Practice Education Team Informs the Practice Education Team if the final year student is not suitable to have a 1st year visit (e.g. the final year student is failing the placement) as soon as unsuitability is identified 22 Process for PAL Clinical Visits Procedures – Prior to start of practice placement Person responsible 1. 1st and final year students paired with each other and informed of dates and practice sites for PAL clinical visit 2. Practice site informed in writing/ email of PAL clinical visits dates approx. Ideally 6 weeks prior to the planned visit (except in circumstances of short-term changes to placements) 3. 1st year and final year students given guidance and information for the organisation of the PAL clinical visit (including learning outcomes, roles and responsibilities, uniform etc) 4. 1st and final year students to establish communication with each other Practice Education Team Practice Education Team 5. 1st year student to plan for PAL clinical visit (travel, uniform, etc) with full awareness of the aims and objectives of the clinical visits 6. Practice Educator made aware of dates of PAL clinical visit in upcoming student supervision Procedures – Start of practice placement 7. PAL clinical visit discussed with Practice Educator (this should start on day 1 of the placement) 8. PAL clinical visit planned (including patient selection, risk assessment and informed patient consent) and agreed with Practice Educator 9. Planned visit communicated to 1st year student 10. Planned visit confirmed and agreed with Final year student Practice placement coordinator/ senior lecturer Final year student initiates PAL Clinical 1 (BSc and MSc). 1st year student initiates PAL Clinical 2 (BSc) 1st year student Practice Education Team Final year student Final year student Final year student (see point 4) 1st year student (see point 4) Procedures during PAL practice visit 11. Initial introduction to the practice environment by the final year student to the 1st year to include: daily routine of the working environment, any key issues related to the clinical setting 12. The final year reminds the 1st year student of fundamental standards of professionalism e.g. courtesy, appearance, manner, confidentiality, punctuality, time-keeping, respect and dignity of colleagues and patients, adaptability 13. The final year student guides the 1st year student with regards to health and safety issues (which can include a risk assessment, equipment and manual handling if appropriate) and infection control 14. The final year will have sought permission from patients prior to the visit and before introducing the 1st year student. The final year student should remind the 1st year student to maintain confidentiality and dignity of the patient at all times 15. After the initial introduction, the final year student is to perform their usual assessments and/ or treatments with the 1st year student observing them Final year student Final year student Final year student Final year student Final year student 23 16. The 1st year student is able to interact with the patients verbally or have minimal manual contact e.g. auscultation, feeling chest expansion or passive movement of a limb. The 1st year student is not allowed to participate in the transfer of patients without the approval and supervision of the Practice Educator Final and 1st year students Intended Learning Outcomes (ILOs) related to the PAL clinical experience For 1st year student: 1. Familiarises themselves with the daily routine of the working environment and key issues relating to the particular clinical setting they enter 2. Recognises the importance of infection control in the clinical environment and up-todate manual handling skills 3. Demonstrates respect for the dignity and confidentiality of patients at all times during and after the PAL clinical visits 4. Applies fundamental standards of professionalism e.g. courtesy, appearance and manner 5. Initiates professional communication towards the patients, the final year student and any health care professionals the student meets during their practice visit 6. Records key relevant information relating to the clinical observation including informed consent and confidentiality 7. Demonstrates knowledge of the codes of professional conduct from both the CSP and HCPC 8. Is familiar with the subjective and objective patient assessment processes 9. Introduces themselves to goal setting, treatment and progression of treatment 10. Introduces themselves to physiotherapy note-writing, including abbreviations 11. Recognises the importance of key medical investigations relative to particular placements e.g. ABGs, x-rays, scans, and the relevance of correct interpretation for treatment planning 12. Reflects on their experience and performance during practice visits. Documents their reflections 13. Undertakes basic literature searches, relevant to their practice visits to supply evidence to support critical thinking and reflection 14. Reflects on what is required of the student in the clinical setting and consider strategies to address those requirements For final year student related to PAL Clinical visit (taken from level 6 common assessment form) 1. Demonstrates sensitivity to the needs of the patient taking into account physical, psychosocial and cultural needs e.g. while seeking on-going informed consent for the PAL clinical visit 2. Maintains appropriate relationships within a team in organising a visit by the 1st year student 3. Communicates in a professional manner with patients/ service users, relatives, carers and colleagues 4. Demonstrates self-management of workload (appropriate to the practice environment), responding to varying circumstances in a professional manner 5. Demonstrates autonomy, accountability and knowledge of own professional and personal scope of practice whilst acknowledging cross professional boundaries 24 References: CSP (2011) Code of Professional values and Behaviour http://www.csp.org.uk/professional-union/professionalism/csp-expectationsmembers/code-professional-values-behaviour HPC (2008) Standards of Conduct, Performance and Ethics http://www.hpcuk.org/aboutregistration/standards/standardsofconductperformanceandethics/ 25 Practice Education Module Descriptors Year 2 BSc (Hons) Physiotherapy Practice Module DATE OF VALIDATION: April 2013 DATE OF REVISION: MODULE CODE TITLE: N/A PT2015 LEVEL 5 CREDITS 15 CREDITS 0 Practice Placements 1, 2 and 3 Year 1 MSc Physiotherapy (pre-registration) Practice Module DATE OF VALIDATION: October 2012 DATE OF REVISION: April 2017 MODULE CODE TITLE: LEVEL 4 &5 Practice Placements 1, 2 and 3 MODULE SUMMARY: The practice education element is a key academic learning process of the course. It facilitates transitional learning and ensures that all students practise physiotherapy safely and competently. All students must pass all practice placements independently to progress on this module. The assessment form, common to all Physiotherapy programmes in London and the South East of England, is used (see e-Appendix 3). Students are assessed by their Practice Educator/s and supported by the Visiting / Link (academic) Tutor. LEVEL 4 All students must complete a 5 week placement (PP1) assessed at Level 4. This is the first placement in BSc Year 2 and the first in MSc Year 1. This practice experience allows the student to develop skills which are assessed using PASS/FAIL criteria at Level 4. LEVEL 5 Two placements – PP2 and PP3 – provide the student with the opportunity to develop their ability in, and understanding of, physiotherapy skills and clinical decision-making. Students will primarily be concerned with consolidating their theoretical knowledge and developing their understanding through the experience of treating patients. They should be involved with the complete management of a service user/client or patient, from assessment to discharge and the experience of patients/clients or service users should span the age range where possible. Initially they will require guidance as they develop the necessary skills. Placements 2 and 3 are assessed at Level 5 and criteria- 26 referenced (see definitive document) and the results of these contribute to the final award and evaluate a progressive level of personal and professional development. PRE-REQUISITES: BSc (Hons) Physiotherapy All Level 4 modules. This includes the 5 week placement (PP1) which takes place in Year 2 and is assessed using PASS/FAIL criteria at level 4 using the common assessment form (see e-Appendix 3 http://www.healthcare.ac.uk/courses/rehabilitationsciences/information-for-pre-registration-physiotherapy-practice-educators/ ) and does not contribute to the overall weighting of the module mark. Preparation for practice includes manual handling training and safeguarding. MSc Physiotherapy Essentials of Physiotherapy. Preparation for practice includes manual handling training and safeguarding. CO-REQUISITES: BSc (Hons) Physiotherapy Concurrent attendance in other first year modules. MSc Physiotherapy Concurrent attendance in other first year modules: Management of Musculoskeletal Movement Dysfunction (30) Management of Cardio-respiratory Dysfunction (15) Neurological Rehabilitation (15) Evaluation of reflection in rehabilitation (15) Psychology for Exercise and Health (15 KEY SKILLS: Communication Self-awareness Interpersonal Creativity and problem solving Working with others Information and communication technology Application of numeracy and literacy Improving own learning and performance Research literacy AIMS: This module will enable students: To develop interpersonal skills, professionalism, clinical reasoning and the management of a variety of patients through clinical experience To continue to evolve independent learning 27 LEARNING OUTCOMES: On successful completion of the module the students will be able to demonstrate achievement of the following learning outcomes. Mandatory requirements 1. Integrate health and safety legislation into physiotherapy practice taking account of local policy and procedures. 2. Demonstrate non-discriminatory practice. 3. Fulfil all responsibilities related to legal ethical and local considerations of professional practice including clinical information (CSP, 2011; HCPC, 2008). Interpersonal skills domain (20% of PP assessment) 4. Establish a therapeutic relationship, demonstrating sensitivity to the needs of others, having an awareness of physical, psychosocial and cultural needs. 5. Establish appropriate relationships within a team, i.e. health and social care staff and students. 6. Communicate in a professional manner with patients/clients, relatives, carers and colleagues using verbal, non-verbal, listening and writing skills. Professionalism domain (10% of PP assessment) 7. Identify individual learning needs, areas for development and the means for addressing these. 8. Develop a reflective approach to practice and respond appropriately to feedback. 9. Manage their workload (appropriate to the practice environment), and respond to varying circumstances in a professional manner. 10. Demonstrate accountability and knowledge of own professional and personal scope of practice; whilst recognising and acknowledging the contributions of team members to the patient/client centred approach Treatment / Management domain (35% of PP assessment) 11. Apply appropriate assessment and treatment strategies, safely and effectively. 12. Monitor and review the on-going effectiveness of planned activity, recognising the need to modify management in conjunction with patients/clients or carers. 13. Ensure the patient/client is central in the management of their health and well-being. Clinical Reasoning domain (35% of PP assessment) 14. Demonstrate an awareness of a holistic process of enquiry by undertaking physiotherapy assessment strategies which are appropriate for the patient. 15. Recognise and interpret clinical features to formulate a problem list using the findings from the patient assessment. 16. Set SMART goals with patients/clients and/or carers as appropriate. 17. Plan individualised treatment/management programmes considering available resources. 18. Select and interpret appropriate measures to evaluate the outcome 28 of physiotherapy interventions. 19. Demonstrate order, clarity and clinical reasoning in documentation. INDICATIVE CURRICULUM CONTENT: The experience gained in each placement is determined by a number of factors including the range of patients/clients/service users, the learning opportunities and the individual learning needs and interests of the student. It is also influenced by the student’s level of knowledge, interest and experience and by the organisation and management needs of the placement. However, the experience is measured against the outcomes for the Levels 4 and 5 placements. The Practice Educator and student will negotiate a learning contract to maximise learning in each environment. The University Practice Education Team will monitor each student’s practice placement profile throughout the entire course to ensure that each individual has experience within and across care pathways with service uses of all ages, including care of the older person, in both acute and community settings and where possible in areas that reflect learning gained in the respiratory/cardiorespiratory, neurological and musculoskeletal modules. Student experience in the clinical practice environment is not seen as stand-alone. BSc (Hons) Physiotherapy Clinical reasoning and theory to practice links are developed by the experience on placement and through further reflection in the associated module ‘Integrating Clinical Concepts’ which is assessed by a reflective practice portfolio. MSc Physiotherapy Clinical reasoning and theory to practice links are developed by the experience on placement and through reflection. Students are encouraged to seek formative feedback on reflective writing skills after PP3 in anticipation and preparation for an associated module in Year 2 ‘Professional Development in Rehabilitation’. This module is assessed by a reflective practice portfolio. LEARNING AND TEACHING STRATEGIES: The practice working week comprises 32 hours per week. Practice placement 1 include prepractice preparation 6 weeks 5 weeks Practice placement 2 Practice placement 3 5 weeks Total Hours: 16 x 32 512 Key note lectures and tutorials: In addition to the pre-practice week (PP1) all students attend a series of further lectures in preparation for PPs 2 and 3. Tutorials in the BSc Integrating Clinical Concepts (ICC) module relate to clinical practice and are included in the BSc overall hours. 29 It is anticipated that students will undertake self-directed private study as further preparation. Practice placement 2 preparation lecture 2 hours Practice placement 3 preparation lecture 2 hours ICC tutorials (BSc) 15 hours Private self-directed study Unknown Total Hours: Approx. 19 Total Hours: approximately 531 ASSESSMENT STRATEGY: This is a practice based assessment based on the student performance on placement Summative 1 Type of assessment Weighting Assesses Learning Outcomes Assessor Practice Placement 1 PASS/FAIL ALL Practice Educator Summative 2 Type of assessment Weighting Assesses Learning Outcomes Assessor Practice Placement 2 50% ALL Practice Educator Summative 3 Type of assessment Weighting Assesses Learning Outcomes Assessor Practice Placement 3 50% ALL Practice Educator BSc (Hons) Physiotherapy A final average mark from practice placement assessments at Level 5 will determine the total practice module mark. MSc Physiotherapy There is no overall mark for this module; the module outcome is pass/ fail. The practice placement assessment form includes criteria to assess HCPC proficiencies including: Practising within legal and ethical boundaries commensurate with level of learning Practising in a non-discriminatory manner Maintaining confidentiality Obtaining informed consent Exercising a professional duty of care Working in partnership with other professional support staff, service, their relatives and carers Demonstrating effective skills in communication 30 Throughout the programme, the practice placements are structured such that they are progressive in nature (academic levels 4, 5 and 6). The universities within the Placement Management Partnership (PMP) have agreed these levels and each designated level reflects the performance standard and not the year of study. The levels of placement assessment reflect the levels of achievable outcome in relation to the development of the extent of the student’s learning. The practice placements are assessed by the Practice Educator who will be HCPC registered, in most cases a Physiotherapist. The Practice Educator may, at times, wish to delegate their supervision of the student to another, suitably registered professional (e.g Occupational Therapist), in order to maximise the learning opportunities afforded to the student. Whoever has responsibility for assessing the student must be familiar with the common assessment form. All placements must be passed independently for successful completion of Year 2 BSc and Year 1 MSc. Achieving a pass: It IS a requirement that the PP1 (Level 4) placement is passed prior to commencement of the module. Practice placements 2 and 3 must be passed separately in order to achieve an overall pass for this module. RECOMMENDED READING: This will vary dependent upon the clinical context. Students are encouraged to refer to appropriate texts/ journals recommended in the various university based modules and to conduct independent literature searches and critical analyses as appropriate to inform their practice. Students may be guided by placement specific recommended reading, accessible from Practice Educators directly or via practice placement information sheets available on each provider’s page on the Placement Management Partnership system. See e-Appendix 6. Ainslie. T.(2012). The Concise Guide to Physiotherapy: Assessment and Treatment. Churchill Livingstone. Elsevier, Oxford. Kenyon, J. & Kenyon, K. (2009).The Physiotherapy Pocket Book – Essential Facts at your Fingertips. Churchill Livingstone. CSP (2011) Code of Professional values and Behaviour http://www.csp.org.uk/professional-union/professionalism/csp-expectationsmembers/code-professional-values-behaviour HPC (2008) Standards of Conduct, Performance and Ethics http://www.hpcuk.org/aboutregistration/standards/standardsofconductperformanceandethics/ 31 Practice Education Online Resources at http://www.healthcare.ac.uk/schools/rehabilitation-sciences/practice-resources/ Module Evaluation The module will be routinely evaluated by the students at the end of their practice placement experience. MODULE LEADER AND KEY TEACHING STAFF CONTRIBUTING TO THE MODULE: Mary Jane Cole and Alison Jones 32 Year 3 BSc (Hons) Physiotherapy Practice Module DATE OF VALIDATION: April 2008 DATE OF REVISION: MODULE CODE April 2013 PT3015 LEVEL 6 CREDITS 30 6 CREDITS 0 TITLE: Practice Placements 4, 5 and 6 Year 2 MSc Physiotherapy Practice Module DATE OF VALIDATION: October 2012 DATE OF REVISION: MODULE CODE April 2017 LEVEL TITLE: Practice Placements 4, 5 and 6 MODULE SUMMARY: The practice education element is a key academic learning process of the course. It facilitates transitional learning and ensures that all students practice physiotherapy safely and competently. All students must pass all practice placements independently to progress on this module. The assessment form – common to all Physiotherapy programmes in London and the South East of England – Level 6 is used. Students are assessed by a Practice Educator/s and supported by the Link tutor. LEVEL 6 There are three five-week practice placements in this module. Students have the opportunity to develop their ability to practise effectively and independently further within the clinical setting. Students will still require guidance as they develop the specialised skills required for certain areas of clinical practice but should demonstrate more advanced communication, management skills and clinical reasoning and integration of theory to practice. This is fostered by the 3rd Year BSc (Hons) or 2nd Year MSc student taking the responsibility for a first year student during their PAL clinical visits. Students are being prepared to take up the role of an independent, reflective and autonomous practitioner. PRE-REQUISITES: BSc (Hons) Physiotherapy Successful completion of BSc (Hons) Physiotherapy Year 2 Practice Module PT2015 is expected prior to the first Level 6 placement. Preparation for practice includes manual handling training and safeguarding. MSc Physiotherapy Successful completion of MSc Physiotherapy Year 1 Practice Module is expected prior to the first Level 6 placement. 33 Completion of manual handling training. CO-REQUISITES: BSc (Hons) Physiotherapy Participation in all concurrent 3rd year modules. MSc Physiotherapy Research Project: 60 credits Physiotherapy practice in context: 30 credits Interprofessional debate/ management: 15 credits Professional development in rehabilitation: 15 credits Self-Management in people with long term and neurological conditions: 15 credits KEY SKILLS: Communication Problem Solving Information and Communication Technology Improving own Learning and Performance Application of Numbers Working with Others AIMS: The aims of this module are to: Further develop clinical reasoning and the treatment and management of a variety of patients in the wider clinical environment using the skills and knowledge acquired in years one and two and to continue to evolve independent learning. Assume the responsibility of an independent, autonomous practitioner. LEARNING OUTCOMES: On successful completion of the module the students will be able to demonstrate achievement of the following learning outcomes: Mandatory requirements 1. Integrate health and safety legislation into physiotherapy practice taking account of local policy and procedures. 2. Demonstrate non-discriminatory practice. 3. Fulfil all responsibilities related to legal ethical and local considerations of professional practice including clinical information (CSP, 2011; HCPC, 2008). Interpersonal Skills domain (20% of PP assessment) 4. Develop a therapeutic relationship demonstrating sensitivity to the needs of others, taking into account physical, psychosocial and cultural needs. 5. Initiate and maintain appropriate relationships within a team, i.e. health and social care staff and students, including external agencies. 34 6. Communicate in a professional manner with patients/clients, relatives, carers and colleagues using verbal, non-verbal, listening and writing skills. Professionalism domain (10% of PP assessment) 7. Demonstrate the ability to recognise and take responsibility for their own learning needs and identify areas for future development. 8. Demonstrate reflection and self-critical awareness skills and respond appropriately to feedback. 9. Demonstrate self-management of workload (appropriate to the practice environment), responding to varying circumstances in a professional manner. 10. Demonstrate autonomy, accountability and knowledge of own professional and personal scope of practice whilst acknowledging crossprofessional boundaries. Treatment / Management domain (30% of PP assessment) 11. Apply appropriate assessment and treatment strategies, safely and effectively. 12. Monitor and review the on-going effectiveness of planned activity and modify it in conjunction with patients/clients or carers. 13. Actively facilitate the patient/client to manage their own health and wellbeing, ensuring they are central to the delivery of care. Clinical reasoning domain (40% of PP assessment) 14. Justify appropriate physiotherapy assessment strategies to complete a logical and holistic process of enquiry. 15. Interpret findings from assessment in order to identify the individual’s strengths and problems as well as a physiotherapy diagnosis. 16. Set SMART goals with patients/clients and/or carers as appropriate. 17. Develop specific and effective treatment plans with patients/clients and/or carers as appropriate. 18. Select appropriate measures to evaluate the outcome of physiotherapy interventions. 19. Demonstrate evidence of clinical reasoning throughout documentation. INDICATIVE CURRICULUM CONTENT: The experience gained in each placement is determined by the setting and the patients/clients/service users receiving treatment. It is also influenced by the student’s level of knowledge, interest and experience and by the organisation and management needs of the placement. However, the experience is measured against the outcomes for the Level 6 placements. Practice Educators and students will negotiate a learning contract to maximise learning in each environment. The university Practice Education Team will monitor each student’s practice placement profile throughout the entire course to ensure that each individual has experience within and across care pathways with patients and service uses of all ages, including care of the older person, in both acute and community settings and wherever possible in areas that reflect learning gained in include the respiratory/cardiorespiratory, neurological and, musculoskeletal modules. Student experience in the clinical practice environment is not seen as stand-alone. 35 There is an opportunity for final year students to demonstrate their skills in professionalism and management by facilitating the PAL clinical visits with the 1 st year students. Additionally this allows the final year student to reflect on their achievements, recognise their own level of skill and encourage learning in others. There is no ‘elective’ placement however students can express a preference for a specialist area or placement provider for their last placement (PP6), however this entirely depends on whether the Practice Education Team consider this a viable option in terms of a student’s placement profile and the suitability and appropriateness of the ‘optional’ placement BSc (Hons) Physiotherapy Clinical reasoning and theory to practice links are developed by the experience on placement and through further reflection in the associated module ‘Critical reflection and reasoning’ which is assessed by a reflective practice portfolio. MSc Physiotherapy Clinical reasoning and theory to practice links are developed by the experience on placement and through further reflection via an associated module in Year 2 ‘Professional Development in Rehabilitation’. This module is assessed by a reflective practice portfolio.. LEARNING AND TEACHING STRATEGIES: The clinical working week comprises of 32 hours per week. Practice placement 4 Practice placement 5 Practice placement 6 5 weeks 5 weeks 5 weeks Total Hours: 15 x 32 480 ASSESSMENT STRATEGY: Assessment(s) Practice placements 4, 5 and 6: Level 6 assessment form Learning Assessed All Outcomes Weighting % 1/3 each Throughout the programme, the practice placements are structured such that they are progressive in nature (levels 4, 5 and 6). The universities using the common assessment form have agreed these levels; each designated level reflects the performance standard and not the year of study. The levels of placement assessment reflect the levels of achievable outcome in relation to the development of the extent of the student’s learning. The practice placements are assessed by the Practice Educator who will be HCPC registered or registered with another recognised Health Care Professional Body. A final average mark from practice placement assessments at Level 6 will determine the final practice module mark. Practice placements 4, 5 and 6 must be passed independently for successful completion of this module. Each assessment is weighted as follows: 1. Interpersonal Skills 20% 2. Professionalism 10% 36 3. Treatment & Management 4. Clinical Reasoning 30% 40% Achieving a pass: It IS a requirement that each clinical placement must be passed separately in order to achieve an overall pass for this module. RECOMMENDED READING: This will vary dependent upon the clinical context. Students are encouraged to refer to appropriate texts/ journals recommended in the various university-based modules and to conduct independent literature searches and critical analyses as appropriate to inform their practice. Students may be guided by placement specific recommended reading, accessible from Practice Educators directly or via practice placement information sheets available on each provider’s page on the Placement Management Partnership system. See e-Appendix 6. Ainslie. T. (2012). The Concise Guide to Physiotherapy: Assessment and Treatment. Churchill Livingstone. Elsevier, Oxford. Kenyon, J. & Kenyon, K. (2009).The Physiotherapy Pocket Book – Essential Facts at your Fingertips. Churchill Livingstone. CSP (2011) Code of Professional values and Behaviour http://www.csp.org.uk/professional-union/professionalism/csp-expectationsmembers/code-professional-values-behaviour HPC (2008) Standards of Conduct, Performance and Ethics http://www.hpcuk.org/aboutregistration/standards/standardsofconductperformanceandethics/ Practice Education Online Resources at http://www.healthcare.ac.uk/schools/rehabilitation-sciences/practice-resources/ MODULE EVALUATION The module will be routinely evaluated by the students at the end of their practice placement experience. MODULE LEADER AND KEY TEACHING STAFF CONTRIBUTING TO THE MODULE: Mary Jane Cole and Alison Jones 37 Roles and Responsibilities Role of the Practice Educator (PE) For each placement, each student is assigned a named Practice Educator/s who is normally an HCPC registered Physiotherapist. The Practice Educator may, at times, wish to delegate their supervision of the student to another, suitably registered professional, in order to maximise the learning opportunities afforded to the student.. It is possible that the named PE may be another HCPC registered professional e.g. Occupational Therapist The Practice Educator together with the student will discuss expectations of the placement, supervise the student and negotiate the learning opportunities necessary to meet required learning outcomes. Other clinicians in the practice setting will also be encouraged to support the Practice Educator in this supervision The Practice Educator is responsible for assessing the student’s competence and will consult with others who have been involved with the student in different settings, where appropriate A key element of the role is to provide the student with regular feedback about progress and to support the development of action plans and learning contracts to assist the achievement of learning outcomes and identification of learning opportunities. A halfway feedback session between the student and their Practice Educator is required for all placements The Practice Educator is a critical facilitator of the learning experience on placement, achieving this through placement planning, effective communication, supervision and feedback to the student Progress is also discussed with the Link tutor. During this visit progress is discussed together with the Practice Educator and Link Tutor and learning outcomes for the remainder of the clinical placement can be agreed The Practice Educator is required to complete assessment documentation. This enables the mutual validation of evidence to support the acquisition of specific skills and appropriate level of competence. See e-Appendix 3 for assessment criteria http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ The Practice Educator is invited to undertake a regular update by attending Practice Education Study days at the School of Rehabilitation Sciences. In preparation for the placement the Practice Educator should: Ensure the placement information on PMP’s website is up-to-date. See e-Appendix 6:http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ Where relevant, ensure the student has a SMART card for e-record keeping. Be aware of the student’s expected level of knowledge and skills and match expectations accordingly (click for the skills taught in university prior to placements) Prepare an appropriate timetable for the student, scheduling time for feedback, preparation and reflection. During the first week the Practice Educator should: Facilitate the student’s integration into the department Provide the student with the most direct contact details so the student can arrange the midway visit by the Link tutor 38 Discuss and agree working hours Inducting the student to the departmental health and safety policy to specific patient groups/ conditions (e.g. infection control, moving and handling, hazard control and risk management). The Practice Educator must highlight high risk areas. Clarify expectations e.g. when formal feedback will be given, caseload, responsibilities and accountability Discuss a learning agreement with the student, negotiating personal objectives Facilitate learning. This may include the organising of appropriate tutorial sessions Provide a range of experiential learning opportunities that respect the rights and needs of patients or clients or colleagues Provide appropriate regular scheduled feedback Take responsibility for the day to day management of the placement Be available to the student and provide advice as appropriate Find time to meet the Link Tutor around midway in the placement Contact the Link Tutor if there any questions or concerns regarding the student If the student is at risk of failing, inform the Link tutor as the earliest point in the placement and complete the Danger of Failure Form (e-Appendix 4 http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/) Undertake assessment of the student On the final day of the practice placement the Practice Educator should keep a photocopy of the completed assessment form and return the completed paperwork to the student. Reference: Cross, V., Moore, A., Morris, J., Caladine, L., Hilton, R and H. Bristow. (2006) The practice-based educator. A reflective tool for CPD and accreditation Role of the Student Prior to the placement the student should: Be aware of all course assessment requirements and regulations relating to the clinical practice components of the course Have completed information governance via http://www.eiceresources.org/ and provided evidence of completion to Practice Education Team administrator. This is an annual requirement for students prior to placements. Students should bring their certificate of information governance to each placement Access information about the practice placement at the earliest opportunity e.g. for recommended reading for the specialist area. This information should be available via the Placement Management Partnership (PMP) (see e-Appendix 6 http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ ) or from the clinical educator/ contact named on the allocation email Review learning outcomes for each practice placement, identify learning needs and setting personal objectives related to the placement and in development of the portfolio Do a SWOT analysis Make contact with the practice area and Practice Educator at the earliest convenience prior to the start of the placement to establish if any additional pre- 39 placement preparation is required e.g. SMART card requirement (this is necessary for record keeping on some placements) Have the contact details of the Link Tutor prior to each placement Update and refresh knowledge/ skills prior to each placement; placement information may include recommended reading Collect appropriate paperwork e.g. assessment form Prior to the placement the student may wish to disclose any disability or specific learning need to their Practice Educator. Please note that students are encouraged to disclose; the university is unable to do this without permission from the student. In most circumstances this is advisable so that the educator can tailor support accordingly Seek formal permission from the School initially and then approval from the placement for any time away from placement or adjustment of placement hours for other commitments (eg: caring commitments, learning support, work). Permission must be sought as soon as possible/ ideally six weeks prior to the start of placement. Please see Student Absence for more details During the placement the student should: Maintain professional behaviour and confidentiality at all times Ensure a time is arranged at the beginning of the placement to discuss expectations, identify learning needs and review learning outcomes with their Practice Educator Identify their strengths and limitations and share these with their educator at the beginning of the placement If the student discloses a disability, the student must discuss any specific learning needs or requirements with their educator Take responsibility for their own learning and proactively seek learning opportunities Ensure that dates are established for completion of the practice placement assessment form at midway and end of placement Inform the Practice Educator of the name and contact details of the Link Tutor Liaise with their Link Tutor within the first week of placement to arrange the mid-way visit. Provide contact number for themselves and their named educator Take responsibility for completing their clinical portfolio (as required in relation to any accompanying relevant assignment) and meeting their learning needs. Time during the placement may be available for this and should be negotiated with their educator Be aware of all departmental policies and procedures including accident and incident reports, manual handling, health and safety policies etc. Students must ensure that their educator has informed them of any local policies Contact their educator and clinical practice area ASAP if they are going to arrive late Contact both the School and the clinical practice area (before 8.30 am) ifunwell . The course requires any absence from placement to be recorded on the placement assessment form and a medical certificate to be produced if the student is unable to attend placement for more than 7 days (including weekends). Inform the School about any absences in addition to sickness (see ‘prior’ to placement) Contact the Link Tutor if problems arise on clinical placement at the earliest opportunity Complete online evaluation (via PMP) towards the end of each placement. The PMP prompts the student to do this via an email 40 Prior to leaving the placement ensure the assessment form is completed with relevant signatures from the Practice Educator Be aware of the European Working Time Directive in relation to placement hours and any paid work which they are is undertaking. Students should not exceed the EWTD and should meet with the practice education team to discuss this if they are concerned. For further guidance please see: www.gov.uk/maximum-weekly-working-hours/overview After the placement: It is the responsibility of the student to return the placement assessment form to the Programme Office within one week of the completion of the placement. The assessment form should include completed learning objectives, a post placement reflection of achievement and final SWOT 41 Role of the Link Tutor The purpose of the Link Tutor is to support both the student and their educator/s during the placement. The Link Tutor may be a physiotherapy academic staff member of the School of Rehabilitation Sciences or the student’s personal tutor or a suitably qualified non-academic Physiotherapist. In the first year of placements students and their educator receive a visit around the half way point in the placement In the final year of placements support to the student and his/ her educator/s will be by telephone, again around the half way point. However in the final year of placements a physical visit will be made if either student and/ or educator requests, where the placement is new to the University or as required Approximately one week before placement the Link Tutor is informed which students they are supporting He/she will inform the student of their availability to visit by the end of the first week of placement Requests the student/s liaise with their educator – the student confirms a mutually agreed time and venue for the midway visit Maintains contact with student/s (and Practice Educators as necessary) to support both with practice-based-learning Visits the practice site during placement around the midpoint of the placement to meet with the student and their educator Follow the procedure for the Midway visit Distribute ‘practice’ newsletters to the placement site/ educator (as prompted by Practice Education Team). Newsletters serve to inform placements about relevant university based matters e.g. Practice Educator study days, placement shortfalls, post-graduate and CPPD opportunities The Link Tutor acts as a moderator (see Midway visit) Document all interactions with students and Practice Educators, including an impression of the placement with regards to level of support and standards. Reports are submitted – in paper or e-format – to the Practice Education Programme Administrator. See e-Appendix 7 http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ Role of the Practice Placement Co-ordinator Promote quality patient centred practice based learning Develop, organise, implement, monitor and evaluate the practice education programmes (BSc and MSc) Implement educational programmes for Practice Educators Be a resource for all parties involved in practice based learning within the Faculty and beyond Liaise with other London HEIs to coordinate PMP placements Liaise with Placement Management Partnership Engage with placement providers via termly Practice Education Liaison Meetings, London Physiotherapy Mangers Forums, London Regional Network Meetings 42 Facilitate practice based learning with Link Tutors, students and Practice Educators as required Assessment Practice Placement Assessment Form See e-Appendix 3 http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ ) There are 3 different levels of assessment (academic Levels 4, 5 and 6). The Link tutor or practice placement co-ordinator can give further guidance if required. The assessment of the student’s performance is divided into two parts. Part One This part carries no marks but the student’s performance in these areas must be satisfactory in order to pass the placement. This part overrides Part 2 of the assessment form if any objective is failed at any point in the placement. In a situation where there is concern relating to safety or professional behaviour a written warning must be completed and must be signed by both student and Practice Educator. A written warning does not constitute failure. Practice Educators must ensure that the relevant boxes are ticked, signed and dated to indicate pass or fail for each objective in Part 1. Part Two This contains four areas of practice each of which contributes to the overall grade: Interpersonal Skills Professionalism Treatment/Management Clinical Reasoning The stated learning outcomes indicate what the student should have achieved by the end of the placement (if a particular learning outcome is not applicable it should be recorded as such, signed by the Practice Educator and disregarded when marking that section). The final grade for the placement is calculated by the University using the marks from Part 2. The four sections are weighted differently at different assessment levels as follows: Interpersonal Skills Professionalism Treatment/Management Clinical Reasoning Level 4 and Level 5 20% 10% 35% 35% Level 6 20% 10% 30% 40% 43 Student Supervision Students must be under the supervision and within reasonable contact of a Practice Educator at all times to comply with the conditions of indemnity. Students in their final year should require less direct supervision than students in earlier years as they should be developing clinical competence and confidence as they approach the end of the course. It is a mandatory requirement that after the student has completed the assessment of a patient/ client/ service user, the proposed patient/ client/ service user management procedures, or any changes to existing patient interventions, are discussed with a Physiotherapist prior to implementing the procedures, to comply with the conditions of indemnity. Students should always know where their Practice Educator or appointed deputy can be located during clinical time. Procedures for contact, should the need arise, such as phone or bleep, should be known. If the student is under the supervision of an appointed deputy to a named Practice Educator, that person must be suitably experienced. If the Practice Educator has to leave the work area and an appointed deputy is not available, then the student stops treating patients/clients but may continue with relevant learning activities such as reading patient notes, books, papers etc. Alternatively, the student leaves the area and continues learning activities in another agreed location. Learning Contract Each clinical practice placement assessment form includes a learning contract which is designed to support learning in the practice setting. The purpose of the contract is to provide a structured learning environment and to encourage students to take responsibility for their learning. During the contracting process students will develop negotiating skills and improve communication, organizational and time management skills. Students are encouraged to address a learning outcome from each of the four areas of practice (interpersonal skills, professionalism, treatment/management, clinical reasoning) and relate them to their current placement. Correct use of the learning contract and the placement assessment form enables the student to benefit maximally from the time spent in the clinical setting. Guidelines for completion of the Learning Contract The student completes the needs identified box (akin to a SWOT analysis) by reflecting upon their strengths and weaknesses. Areas for development and improvement or any areas of special interest can be identified prior to the start of the placement. Following discussion, the student and Practice Educator discuss the resources available on the placement. Via negotiation the student and educator identify the 44 learning outcomes for that placement based on the learning outcomes in each section of the clinical placement assessment form The planned learning outcomes are written in the appropriate boxes as well as the methods by which students and staff will recognise when learning has been achieved The agreement is reviewed at the halfway point of the placement and normally coincides with the halfway assessment. Learning outcomes achieved are recognised, any problems encountered are discussed and if required, remedial measures are determined for implementation during the second half of the placement The agreement is further reviewed at the end of the placement and any problems encountered are discussed as necessary. Students should ensure they complete the reflection on achievement of learning outcomes. Any areas that need to be addressed in subsequent placements are identified The student documents a further short SWOT in anticipation of subsequent placements The role of completing the learning contract is generally the responsibility of the student and will be monitored by the Practice Educator The Midway Assessment This is a key element of the clinical assessment form. Any challenges that may have arisen during the first half of the placement are identified and appropriate remedial action is determined for implementation during the second half of the placement. The problem and action must be documented on the midway assessment so that it is clear to the student and the Practice Educator what steps are to be taken so that the student has every chance of successfully completing the placement. This enables students to utilise their time in each placement effectively and efficiently. Guidelines for completion of the Midway Assessment The students are assessed against the learning outcomes for the four areas of practice, interpersonal skills, professionalism, treatment and management and clinical reasoning. Grading the individual learning outcomes by underlining/ highlighting the appropriate descriptors gives a clear indication to the student and the educator the areas that must be focused on to improve the student’s performance in the second half of the placement. In the comments box the educator can illustrate how the student was graded with objective comments as appropriate. There should always be recommendations of what the student needs to focus on to improve their performance. If you have any questions or queries please do not hesitate to contact the Practice Coordinators or discuss the assessment form with the LinkTutor. Midway Visit and Assessment Procedure The role of the Link tutor is key to the process by which the University supports its students and educators on the practice placement. The Link Tutor should plan support to the student and educator around the mid-way point of the placement to coincide with 45 timing of the student’s half way assessment and provides the opportunity for discussion and feedback which can be significant in the continuing student learning experience. Students are routinely visited on all placements in the first year of placements. In the final year of placements, a phone call to both student and educator is current practice. Please note that where a visit does not take place there must always be communication between the Link Tutor and the Practice Educator and with the student to affirm that progress and outcomes are satisfactory. Wherever or whenever a visit is deemed necessary by any party i.e. the University, the student or the Practice Educator, this must be arranged, for example where a student is struggling or if a placement is new to the university. Practice education modules are moderated in the same way as others in the School of Rehabilitation Sciences. It is recommended that this moderation take place during the midway visit, led by the Link Tutor. A record of the visit is noted routinely and is placed in the student’s file. This provides helpful information to refer to particularly when a student is experiencing difficulties around performance and may be in danger of failing. In addition, Link Tutors are prompted to comment generally on their impression of the placement e.g. supportive; novice educators and serves to alert the Practice Education Team if additional support is necessary. Format of visit During the physical midway visit the Link Tutor meets with the student and their educator together in a suitable setting e.g. quiet room, away from interruption. A threeway discussion is preferred to ensure that there is a transparent process of dealing with feedback and any potential conflict. The student should remind their educator of this format. If a three-way discussion is not possible due to sickness, absence or an urgent clinical issue then the Link Tutor must ensure that further communication is conducted in a transparent way subsequent to the meeting (e.g. via email or telephone including student and educator). During the mid-way visit the Link Tutor enquires about the student’s performance. It is expected that this will either be in light of the midway assessment marks, or if not yet completed, a prediction of these marks. This discussion should also include how the marks have been awarded. The Link Tutor should use the Link Tutor proforma to document points from the meeting. During the midway visit or telephone discussion the following should be raised: 1. Outline of the purpose of the visit (including the benefits of the 3 way discussion process) 2. The nature of the placement e.g. caseload 3. the amount and level of supervision 4. Nature and amount of feedback provided 5. The Link Tutor should enquire and be assured about the student’s ability to practise safely 6. The assessment form and the student’s strengths and weaknesses in relation to the documented learning outcomes. Ideally, and certainly with final year 46 students, the student should identify some of their strengths and weaknesses themselves as this promotes the independent learner 7. The Practice Educator comments on expectations of the student and how these have been met 8. Negotiation of how the student intends to demonstrate learning outcomes for the remainder of the placement with examples of actions documented on the Link Tutor report form. It is useful – particularly with more senior students – to encourage them to ‘lead’ this discussion as it facilitates an opportunity for them to determine their own learning needs (in preparation for future lifelong learning processes) 9. A summary of the midway visit, outcomes and any agreed actions should be clearly documented on the Link Tutor report form. Any subsequent communications or actions are dated and documented on the same form 10. At the end of the meeting there should be clarity and agreement amongst all around priorities, actions and expectations in terms of learning outcomes for the remainder of the placement. All parties should agree and sign the Link Tutor report form if possible 11. The Link Tutor emails a short summary of agreed actions to student and educator 12. Following completion of the placement the Link Tutor forwards the form to the practice education Programme Administrator within one week following the end of the placement. See placementproblems for further information. 47 Practice Portfolio Students are encouraged to reflect on their learning, their competency and on clinical and professional issues by developing a clinical practice based portfolio. The CSP (2011) recommends that: 1) You should be looking to record your learning and the change it made to your practice rather than the factual details of your experience. 2) Keeping your portfolio should be seen as part of your working life. It should be integrated into your work, rather than an extension of it. (CSP 2011) The clinical portfolio has two main purposes: (1) It is a record of the student’s clinical experiences during the course. It has the potential to be an excellent resource for the student as new information is gathered from the practice placement experience. It can act as a valuable resource for future placements and in preparation for job applications. It introduces the student to the concept of lifelong learning and the requirement for evidencing CPD for the purposes of registration with the HCPC. Writing reflectively in a portfolio gives the student the opportunity to identify what has been learned from ‘significant events’ and how their practice has or will change as a consequence. The student may wish to share some personal reflections with their Practice Educator. Reflective accounts can contribute positively to any of the placement learning outcomes e.g. inter personal skills, clinical reasoning. The portfolio should reflect personal and professional growth and development as the student progresses through their placements. Students are encouraged to use the CSP ePortfolio as a repository for evidence of their CPD. (2) There are clinically associated university based modules within both programmes. These modules are designed to augment the clinical education experience, to enrich integration of academic and clinical practice and to develop heightened skills of reflection. One of the requirements is that the students complete a record of selected manual handling techniques whilst on practice placement. The student may request that you observe them performing these techniques and sign to say that they are independent. The student needs to complete a minimum of 40% of these manual handling techniques during Year 2 (BSc), Year 1 (MSc) and another 40% during Year3 (BSc), Year 2 (MSc). a. BSc (Hons) Physiotherapy The modules Integrating Clinical Concepts (Year 2) and Clinical Reflection and Reasoning (Year 3) – see e-Appendix 1 - draw upon the student’s clinical experiences gained in placements. b. MSc Physiotherapy The module Professional Development in Rehabilitation in Year 2 is assessed via a clinical profile. 48 Involvement of the Practice Educator in the Student’s Clinical Portfolio Students will require their educator to sign the Manual Handling Competency checklist. The student is expected to compile other content required for the portfolio independently. However there may be some tasks that the student is completing for their module or personal portfolio – that the educator might like to integrate into the experience he/she is providing for the student e.g. clinical reasoning forms, significant incident reflective practice forms. Evidence from student documented reflections can illustrate and support learning outcomes e.g. demonstrating clinical reasoning via an annotated reference or significant incident. Students value feedback on their reflective writing skills. It is hoped that the Practice Educator will support the completion of the clinical portfolio by allowing the student the equivalent of a half-day a month (approximately an hour a week) to work on this activity. This reflects the CSP’s recommendation on the time clinicians should spend in normal work hours on CPD. References: CSP. (2008). Keeping a Portfolio CSP 2008. The CPD Process. 49 Placement Problems / Issues If problems or issues arise during the placement, or as a consequence of the placement experience it is important that the student receives support at an early stage rather than waiting until their work has been affected. The student may choose to talk things over with their Practice Educator in the first instance. If concerns continue or the student does not wish to discuss concerns with their educator the student should be encouraged to contact the Link tutor at the earliest opportunity – the Link Tutor designated to visit the placement is the first person to call upon for guidance. Additionally, there are support systems at the School of Rehabilitation Sciences and a range of resources to support the practice educator are available at http://www.healthcare.ac.uk/schools/rehabilitation-sciences/practiceresources/ An early meeting together with the Link Tutor is advised. If problems persist on placement the student, Practice Educator and/ or Link Tutor may choose to discuss these further with the University practice placement co-ordinator. If a student is experiencing problems prior to the commencement of their placement (e.g. sick family member, issues with child care etc) or has a general anxiety concerning their forthcoming placement, the School of Rehabilitation Sciences encourages prior disclosure of these problems to the placement co-ordinator who can inform the Practice Educator and Link tutor as appropriate. However, information can only be disclosed if the student has given their consent. If the School has not received the consent of a student this information cannot be provided. Link Tutors may ask a student being visited if they wish to disclose any issues that may have an impact on the placement experience; again, it is the student’s choice to inform or otherwise. It should be noted that a student may wish any disclosure to remain confidential between themselves and the Link tutor. The Failing Student Occasionally a student may not be performing at an acceptable level and is not progressing despite all support and opportunities provided. It is never an easy decision to fail a student but sometimes this is both necessary and appropriate. Failure may be in relation to the learning outcomes in Part 2 of the placement assessment form. On occasion it may be in relation to Learning Outcomes in Part 1 of the placement assessment form i.e. Safety (LO1) Non-discriminatory practice (LO2) Rules of Professional Conduct (LO3) Please note that failure of any aspect of Part 1 of the assessment form overrides Part 2. See below for specific guidance on safety on clinical placement. The following process is to be followed: 50 If a student is at any risk of failing a practice placement, for whatever reason, it is the responsibility of the Practice Educator to inform the Link Tutor at the earliest opportunity. This allows collaborative discussions involving the student, Practice Educator and Link tutor to focus on identifying the problems, action plan and possible solutions An academic member of the University Practice Education Team will respond to any concerns raised by Practice Educators within one working day via email or telephone Once the University is informed extra support can be provided to the practice placement, normally via the Link tutor. An action plan should be agreed between the student, Practice Educator and the Link tutor – the ‘Danger of Failure’ form can be used here (see e-Appendix 4) – within 3 working days, via email telephone or in person. A visit can be organised within 5 working days to support the student and Practice Educator if required or requested If it is known that a student is at risk of failing the practice placement it should be discussed with the student as soon as the risk is apparent. At this point the Danger of Failure form must be completed. If the risk remains at midway assessment this must be documented accordingly on the assessment form (signed by both student and Practice Educator). Both completion of the Danger of Failure form and the assessment form gives the student all opportunity to understand where the problems lie and to act constructively on feedback. A copy of the Danger of Failure form must be given to the student and the Link Tutor Danger of Failure form Indicators of poor performance and an action plan with objectives to be achieved should be written. The report must be written as soon as possible following the possibility of failure being apparent and must not be delayed until the halfway or final assessment. It must be signed – or agreed via email – by all those involved in the assessment of the student i.e. Practice Educator, Link Tutor and the student. The action plan should identify the minimal acceptable standard for a student to pass the clinical placement. The action plan should illustrate to the student what steps are to be taken so that he/ she has every chance of successfully completing the clinical placement Placements will not normally be terminated unless it is mutually agreed by academic and practice staff that the student is unsafe to themselves, patients or staff. This will constitute a failed placement and is recorded in Part 1 of the assessment form. See below for guidance on safety 51 A failed placement Students are permitted only ONE resit of ONE of the practice placements in any ONE academic year. Students are expected to gain experience on placement in areas of physiotherapy that reflect cardio-respiratory, neurological, musculoskeletal, rehabilitation for older people and in a range of settings including the community. A failed student will be required to repeat the placement in the same speciality and in a similar setting to that of the failed placement, wherever possible, and at a time to be determined by the practice placement co-ordinator in consultation with the Course Director. This may result in the student graduating later. Where a placement of the same speciality is not available all efforts will be made to place the student in as close a related placement as possible A second failure of a placement in any ONE academic year (regardless of whether this is a resit at one particular placement or a first attempt at a subsequent placement, having failed an earlier placement) will normally result in the termination of the student's registration on the BSc (Hons) Physiotherapy programme of study. If a student feels that there are mitigating circumstances that have affected their performance then they have a right to appeal and this process will be in accordance with the SGUL General Regulations. This is subject to consideration of mitigation by the Board of Examiners Should the placement be failed more than once, a student’s registration is normally terminated. If a student feels that there are mitigating circumstances that have affected their performance then they have a right to appeal and this process will be in accordance with the SGUL General Regulations Safety on Placement Prior to any practice placement the student will have been assessed for competency in core manual handling techniques in the University setting. Lectures, tutorials and practical sessions refer to additional safety related issues including self-positioning when treating and safe use and application of equipment. Reference is made to ‘risk assessment’ e.g. prior to manual handling, assessment and patient treatment and intervention. However the practice setting presents additional potential hazards with which students may be unfamiliar. The Practice Educator must highlight high risk areas. With guidance the student must apply reasonable knowledge of departmental health and safety policy to specific patient groups/ conditions (e.g. infection control, moving and handling, equipment, hazard control and risk management). The University makes recommendations to reduce the risk of a student failing a placement on grounds of unsafe practice: During placement induction all students should be informed of local hospital and physiotherapy policies or protocols on safe practice and given the opportunity to 52 clarify any misunderstandings (e.g. policies may differ across settings and placement experiences) Whereas the final year student is expected to be able to assess and treat patients safely, the student on their first placement will require more supervision and guidance with safety issues. Irrespective of the student’s level there should be clear expectations by the Practice Educator of what is considered safe and unsafe practice and the educator should ensure that the student understands these clearly Examples of best and unsafe practice are helpful: o Safe practice e.g. policy of 2 therapists in attendance when a patient first practises stairs; carrying out standard checks on patients after electrotherapy (Cross, V. 2001) o Unsafe practice e.g. student alone in attendance when a patient first practises stairs; not carrying out standard checks on patients after electrotherapy (Cross, V. 2001) When potential or actual unsafe practice has been noted, the student must be advised accordingly. Where a patient, student or individual is unharmed this can be viewed as a constructive learning experience. The student must understand and appreciate the safety risk, its severity, reflect upon and learn from this and from feedback from their Practice Educator and/ or others. Subsequently they should demonstrate their ability to avoid repeating their ‘mistake’ and apply good practice. There should be no need for any written warning. Local trust safety documentation can also guide this process and can be a helpful learning process for the student. In some situations however a first ‘written’ warning may be required. There must be documentation of this first warning on both the Danger of Failure form and the assessment form (Part 1). The student needs to understand in a constructive way the potential of their unsafe practice and what the outcome is if the same unsafe practice is repeated i.e. a final warning or outright ‘fail’ if a serious breach of safety or harm has taken place. Should the student make the same mistake a second time despite verbal and written feedback, this warrants a final written warning or, in the case of a serious breach of safety, a fail. If a student demonstrates unsafe practice in a further but unrelated incident, due consideration must be made as to its relevance to the first incident recorded. A second but unrelated incident should not necessarily warrant a final written warning. See point 2 in checklist below. It must be noted that what justifies as unsafe practice can vary between specialities and across different settings. Practice Educators must be confident that their student knows the contraindications to treatments that would otherwise count as unsafe practice e.g. nasal suction for a patient with a fractured skull; and the risks associated with working in certain environments. The Practice Educator has the final decision on what warrants safe or unsafe practice. 53 Documentation of forms should be succinct and explicit, highlighting incorrect practice. Examples of practice that can warrant a ‘warning’ or ‘fail’: Examples of warnings – in an outpatient musculoskeletal setting – may include: o Not recognising and or able to ask the appropriate red flag or special questions during a subjective (despite running through them beforehand) o Not knowing the appropriate contraindications to ask prior to treatment e.g. such as electrotherapy or mobilisations (despite running through them) o Patient handling and positioning e.g. bed height/ risk of patient falling, poor/ inappropriate handling of limbs o Harm coming to a patient after inappropriate moving and handling o Using a piece of equipment that has not been shown to the student e.g. Laser o Failing to comply with CSP standards in regards to notes, goal setting, including patient/ carers in treatment plans, “documentation is either of poor quality or absent”. o Interpersonal skills e.g. lack of feedback to supervisor and continuing to not check they are treating appropriately o Unable to leave a student on their own to carry out a subjective and objective (by the end of the placement) Examples of warnings – in a ward setting – may include: o Not putting correct footwear on patients o Not looking at the observation charts prior to assessments o Not re-attaching patients to oxygen without prompting o Not being aware of precautions/contraindications to treatments o Missing patients off a caseload list Examples of what may warrant a fail in a ward setting may include: o Any of the above repeated after a final written warning has been given o Compromising a patient’s airway o Using a piece of equipment that has not been shown to the student e.g. IPPB, manual hyperinflation and any suctioning equipment without being shown or without the clinical educator being present o Harm coming to a patient after inappropriate moving and handling o Unable to leave a student on their own o A combination of different examples of safety issues happening throughout a placement Part 1 of the Placement Assessment Form identifies a ‘fail’ as: o Failure to apply knowledge of departmental health & safety policy to specific patient groups/conditions (e.g. infection control, moving and handling, hazard control and risk management) o Persistently fails to protect self or use protective equipment correctly o Is unaware of or disregards the contraindications of treatment o Persistently applies treatment techniques and handling skills in a way which puts patient and/or self at risk o Is unreliable in reporting and often fails to tell the educator about adverse findings and/or patient complaints o Persists in unsafe practice despite verbal instruction and/or warnings 54 It may be helpful to refer to a checklist to guide the Practice Educator with the process for managing students who are in danger of failing due to unsafe practice. Checklist 1. Is the student in danger of failing due to safety issues? No – no specific action required Yes o Discuss and feedback to student o Contact Link tutor to discuss support strategies and/ or arrange visit. Refer to Danger of Failure form o Meet with Link tutor – prior to mid-way visit if required. Action plan agreed between Practice Educator, student and Link tutor o Complete Danger of Failure form and distribute to relevant parties o First written warning IF indicated and document on Part 1 of placement assessment form o Student must know outcome i.e. if repeats same incident will receive a written warning or a final ‘written’ warning (if already received a documented warning) or an outright ‘fail’ depending on significance of safety breach o Discussion of risk assessment o Practice Educator to monitor performance and feedback to student and Link tutor 2. Does student demonstrate further unsafe practice? No – no specific action required other than positive feedback to student on improved performance Yes – is this different to the first incident? o If distinctly different the process is as above o If this is a repeat of the first example of unsafe practice a final warning should be given and documented on Part 1 of the assessment form o Further discussion and review of action plan between practice educator, student and Link tutor o Discussion of risk assessment o Monitor performance 3. Is the same incident repeated a further time? No – no specific action required other than positive feedback to student on improved performance Yes – this warrants either a final written warning or a fail (depending on previous steps in process) o As above if a final written warning o The Link tutor and university practice placement co-ordinator must be informed o All documentation must be completed and agreed by clinical educator and student prior to the student leaving the placement o If student fails and are deemed to be unsafe, they must leave the placement 4. Are there other factors underpinning a student’s ability to practise safely? 55 It is possible that communication or learning difficulties may underpin safe practice on placement e.g. poor written, spoken or understanding of English. In this situation it is possible that the placement may have to be terminated on grounds of safety. It is imperative that any concerns whatsoever regarding communication or professional behaviour are brought to the attention of the Link tutor at the earliest opportunity. Reference: Cross, V. (2001) Approaching Consensus in Clinical Competence Assessment. Physiotherapy. 87. 7: 341-350. Students raising concerns in practice Within the programmes of study there are opportunities for students and those that support them from the university and in practice settings to use The pathway to address concerns during practice placement about teaching and learning or where a student observes or identifies a situation or event, which has the potential to cause risk or harm to an individual(s) or organisation is in e-Appendix 8 at http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ ). 56 Professional conduct Health and Safety policies dictate the parameters of dress and appearance in the clinical situation. As a general guideline, students should wear defined clinical uniform on all clinical placements unless otherwise advised by their Practice Educator. Students will be expected to conform to the uniform requirements of each clinical site. The uniform is normally a short-sleeved white tunic, blue trousers and soft-soled, non-slip footwear in black or navy blue. No obtrusive make-up should be worn and jewellery, if any, should be discreet. Wedding rings, plain stud earrings and fob watches are normally acceptable. Hair should be kept off the face and long hair should be tied up. Students should not wear their uniform outside of the clinical site due to the risk of cross infection e.g. MRSA in the community. Students will be required to demonstrate adherence to the rules of professional conduct in every practice setting commensurate with their level of experience. The CSP Code of Professional Values and Behaviour sets out the profession’s expectations of all members: qualified physiotherapists, associates and students. This should be adhered to by all students at all times across the programme. CSP (2011) Code of Professional Values and Behaviour http://www.csp.org.uk/professional-union/professionalism/csp-expectationsmembers/code-professional-values-behaviour HPC (2008) Standards of Conduct, Performance and Ethics http://www.hpcuk.org/aboutregistration/standards/standardsofconductperformanceandethics/ Disclosure and Barring Service (DBS) As part of the registration and enrolment process in Year 1, all students are required to complete a DBS clearance. Students have a responsibility to self-declare should their status be affected. Universal precautions Hepatitis B, T.B, HIV Undergraduates are (at present) required to have active immunity to Hepatitis B. Before entering a clinical area it is the responsibility of the student to be familiar with the policy of the unit concerning HIV and Hepatitis B and any other disease categorised as confidential or notifiable or one that requires extra precautions to be taken. Every person entering a clinical area has the responsibility of implementing the agreed policy of the area concerning HIV and Hepatitis B. Personal property Neither hospitals nor Universities accept responsibility for the theft or loss of student’s personal property. It is their responsibility to take extreme care when in class or in the clinical setting particularly with jewellery which may have been removed in the practical class or to treat a patient in a clinical setting. Security 57 Due to the increasing number of thefts and other related incidents on University and Hospital premises there are frequent security checks. Students should carry their student identity card (e.g. Library card) with them at all times and produce it when requested by a person in authority. Student consent to act as a model for teaching sessions To avoid injuries and prevent emotional distress the clinical educator should obtain informed consent from students when the student is required to act as a model for learning and teaching purposes. Additional requirements on placement Increasingly in musculoskeletal outpatient settings the student will require a SMART Card and NHS RIO training. Where this is necessary this should be stated clearly on the student information provided via the Placement Management Partnership (PMP). The process to acquire SMART Cards can take some time (up to several weeks in some Trusts) and the student must be mindful of this and be sure to check if a SMART Card is required at the earliest opportunity. A SMART card is increasingly required in practice settings for the purposes of record keeping and where this is necessary, the process of how to obtain one must be outlined in the information sheet. NB the responsibility to provide this is changing; it may be the provider’s or for students starting this academic year, the University’s. 58 Practice Placement Hours Students are required to complete approximately 1000 hours of practice-based learning (CSP 2010) as follows: Practice placement 1 including 1 week pre-practice preparation Practice placement 2 Practice placement 3 PAL visits (BSc and MSc) Academic modules: Integrating Clinical Concepts (ICC) Critical reflection & reasoning (CRR) (BSc) Professional development in rehabilitation (PDR) (MSc) Practice placement 4 Practice placement 5 Clinical placement 6 Total Hours: 31 weeks x 32 hours 6 weeks 5 weeks 5 weeks Approx 1 week 5 weeks 5 weeks 5 weeks 1024 Each practice placement will normally comprise a minimum of 32 hours a week. Students are aware that they are required to fit in with the service requirements of the practice placement, e.g. 7 day working, 12 hour shifts etc. However to enable effective learning students may benefit from planned time during the week e.g. one half-day off per week. This time is normally negotiable but some students may have commitments that are not negotiable e.g. dyslexia support or caring commitments. In some cases students may wish to work additional hours to make up placement hours lost due to illness or bank holidays. The working hours for the placement should be discussed early in the first week of placement (see role of practice educator). Please remember when organising working hours that in some cases the students may spend up to 3 to 4 hours travelling a day. We recommend that students monitor their hours in practice and if required, consider enhancing the time on placement by negotiating with their Practice Educator. In addition, some international students are expected to complete additional hours as guided by the country’s regulatory body. Recording placement hours The clinical placement assessment form carries a ‘record of the hours completed’ on placement. The hours spent on practice placement must be recorded by the student and upon completion must be totalled and signed off by the Practice Educator. If completion of the recommended hours on placement is at risk due to absence, (see Absence during Placement) arrangements can normally be made for the student to make up the required number of hours either during the placement itself or prior to graduation. Under certain circumstances, the hours may have to be completed after other course components have been satisfied. A student must complete a minimum of 50% of the practice placement for it to be counted towards their degree classification. The Practice Educator must be confident 59 that they can give a fair assessment of the student’s performance. The emphasis in this situation would be on the quality of the student’s performance and the student’s ability to achieve the learning outcomes within the time frame. If on discussion with the Link Tutor, the Practice Educator feels unable to give a true assessment of the student’s performance, this placement will not count towards their degree classification (deferral of practice placement). Reference: CSP. (2010) Learning and Development Principles for CSP Accreditation of Qualifying Programmes in Physiotherapy. Available at: http://www.csp.org.uk/documents/learning-development-principles-cspaccreditation-qualifying-programmes-physiotherapy 60 Student Absence during Practice Placement It is the responsibility of the student to inform the Practice Educator in the event of any absence during a placement by 8.30am each morning of absence, indicating approximately how long they expect to be absent. The student must also inform the School via the Practice Placement Administrator placementteam@sgul.kingston.ac.uk The absence will be recorded and the appropriate academic staff informed if necessary. If the student is unable to attend placement for more than 7 days (including weekends) then the student will need to be signed off work by their GP and a medical certificate will need to submitted to the placement coordinators Compassionate and/ or other forms of leave If a student is aware prior to the commencement of a placement that they will be absent for any length of time, written approval must be sought from the Practice Education Team/ placement co-ordinator, stating the duration and reason for the absence e.g. family wedding. If approved, the School of Rehabilitation Sciences will inform the clinical practice site of permission to be absent from placement. Occasionally a practice placement cannot support a planned absence and this may lead to the placement being substituted with a site that can better deal with a particular situation. The reason for any absence is recorded by the Programme Administrator placementteam@sgul.kingston.ac.uk Holidays cannot be taken during clinical practice placements. Nor can a student be absent from a placement for work purposes. Mitigating Circumstances If for reasons of sickness, family or other possible extenuating circumstances a student is unable to start, complete or withdraw from a placement, the student must follow the School’s mitigating circumstances procedure. In cases of ill health the student must have health clearance from Occupational Health. This appointment is requested by the student’s personal tutor and should be expedited as quickly as possible so that arrangements can proceed with arranging subsequent placements. The decision to defer or repeat a placement is at the discretion of the Exams Officer. Where a student is advised by the university to discontinue a placement the student must sign a disclaimer that they ‘wish to continue with the placement despite advice given by the university’. The student must understand that where learning outcomes are poor e.g. a failed placement, it is not possible to claim mitigating circumstances retrospectively. 61 Submission of Assessment Form Before returning the completed assessment form, the Practice Educator must take a photocopy for their own records. Occasionally the Practice Educator may be contacted by the School to verify the content of the assessment form. Students are encouraged to take a copy of the assessment forms before submitting them as they cannot be subsequently returned and office staff cannot provide photocopies. It is the student’s responsibility to submit the original assessment form (NOT a photocopy) to the School of Rehabilitation Sciences. Completed clinical practice assessment forms must be posted by hand in the assessment box outside the Pre-reg Programme Office, Room number 72. 2nd Floor Grosvenor Wing, St George’s Hospital, University of London by 4pm on the Friday following the end of a practice placement. The responsibility for the submission of these documents lies entirely with the student. In the exceptional situations where the student is unable to manually submit the completed assessment form, the form should be posted by Royal Mail – via recorded delivery – to the programme office for the attention of the Practice Education Team programme administrator. The student must inform the administrator by email of this at the earliest opportunity and retain a copy of the recorded delivery details. Assessment forms handed in after 4pm on the day of submission will be marked as a late submission and the mark will normally be capped at the pass mark. The exception to this is where the candidate is able to show good reason for the late submission (e.g. mitigating circumstances). The Board of Examiners may, at its discretion, use the full range of marks available for that assessment. 62 Equal Opportunities Policy statement The School of Rehabilitation Sciences, Faculty of Health and Social Care Sciences, Kingston University, St George’s University of London confirms its commitment to a comprehensive policy of equal opportunities in employment in which individuals are selected and treated on the basis of their relevant merits and abilities and are given equal opportunities within the School. The aim of this policy is to ensure that no job applicant or employee should receive less favourable treatment on any grounds not relevant to good employment practice. The School is committed to action to make this policy fully effective Disability Statement The School of Rehabilitation Sciences, Faculty of Health and Social Care Sciences, Kingston University, St George’s, University of London is committed to the fair and equal treatment of all individuals regardless of disablement. The Faculty is also committed to full compliance with the requirements of the Equality Act 2010 and the Special Educational Needs and Disability Act 2001 and other anti-discrimination laws. For further information see link: http://homeoffice.gov.uk/equalities/equality-act/ All programmes offered by the Faculty have both academic and clinical practice components and either lead to, or are dependent upon, registration with professional bodies. Therefore all applications will be considered in relation to guidelines set out by both the relevant professional bodies and the university and will be subject to occupational health clearance. It is acknowledged that practice areas are varied in the nature of the client group and specialty and also in their philosophy of care. All local NHS Trusts and other placement providers have equal opportunity policies to which staff members adhere. Placement areas are selected in order to enable all students to achieve the required skills on completion of the programme. It is not possible to select specific placements for individual students but where possible consideration will be given for students with specific needs. Students are again reminded that adjustments may be dependent on their disclosing their disability to appropriate staff on clinical placement. Disclosure of Information The School of Rehabilitation Sciences actively encourages prior disclosure of any special needs or requirements before the commencement of a practice placement. However, information can only be disclosed to the placement site if the student has given their consent. If consent has been received we encourage the student to contact their Practice Educator directly to discuss any concerns and anxieties either person may have. Some students prefer to have this discussion during the first week of a placement. Students who are comfortable to disclose their disability currently write a letter/ send an email to the Practice Educator as soon as practically possible prior to the commencement of the placement. If a placement is arranged at the last minute due to cancellations or shortfalls this information unfortunately will not be sent within the optimal timeframe for 63 ease of planning appropriate placement support. If the School has the permission of the student to disclose information the School will do this in as timely a manner as it is able to. Disability Support (see e-Appendix 5 at http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ ) All students will have been cleared by Occupational Health prior to commencement of the course and encouraged to declare to the university their disability. It is likely that they will have had a needs assessment. Support specific to that assessment that is practicable to provide will have been given in university. Some of that support may be available to the student while on practice placement and a resource pack to support practice educators with disabled students is available at http://www.healthcare.ac.uk/schools/rehabilitation-sciences/practice-resources/. Students are not obliged to divulge their disability or learning need. Whilst it is the student’s choice to divulge such information the practice education team strongly recommends that students divulge and discuss their disability with their practice educator. Prior to arriving on placement, should a student with a disability choose to divulge their need they should consider the following: Sending a disclosing letter/ email to the Practice Educator. This should include a statement of their impairment and the strategies or equipment that the students may be using. This letter may be supported by the student’s Summary of Support Needs. This document is forwarded to the department from the Disabilities Adviser after consultation with the student The Practice Educator should be notified 6 weeks prior to commencing each placement where practicable and given opportunities by the student to discuss their strategies in the clinical environment they are entering Where students have a placement changed at the last minute they will bring their letter to the new placement The Practice Educator and the student can contact the University Disability Coordinator (see Staff List) to assist at any stage with this process Providing that a student has been needs assessed, clinical practice and academic progress should be within the normal criteria for developing learning contracts and assessment of that placement. At the commencement of a placement and throughout that placement, the student’s progress should be consistent with the normal demands placed on a student for their stage in training. However strategies used effectively that have been discussed prior to the placement and which can be accommodated in the clinical environment, should be taken into consideration as successful contributions to achieving a satisfactory placement Permission by the student must be sought from the Practice Educator for the use of certain pieces of equipment e.g. Dictaphones. The Practice Educator may need to refer to local Trust/ department policy for guidance It is advisable for the half way assessment to be clearly documented and discussed with the Link tutor. Additional support for that student, if appropriate or necessary, may then be given. 64 Declaring or recognising disability for the first time: Some students choose not to declare a disability or indeed may not be aware they have a disability and this may only become apparent when they begin to experience problems on practice placement. Normally students declare a disability in University and support for this will be carried out during University activities. However if a student is declaring to the Practice Educator for the first time or if this is the first occasion where a disability may be suspected: The Practice Educator is advised to notify the Link tutor who will in turn liaise with the practice placement co-ordinator and the disability co-ordinator. It is helpful if a precise but brief report can be submitted to the college at half way As the formal process of disability NEEDS assessment and support takes time and may be longer than the duration of the placement, the measure of support may be limited at this stage. The formal disability assessment support process will swing into action at this stage The student will be expected to proceed to completion of the placement and be assessed by the normal criteria for their stage A report of their half way and final report for the placement should be sent to the Examinations Officer and Course Director advising them of the difficulties the student experienced and any support that was given. This will then be considered at subsequent exam boards in the student’s progress At the discretion of the Disability officer and Course Director or Personal Tutor a student can at any time be referred back to Occupational Health for further assessment 65 Administration of Placements Placement Allocation When allocating placements to each student a number of factors are considered. The student profile of clinical practice experience and theoretical knowledge is taken into account to ensure that each individual addresses core areas of practice. Student requests with regard to geographical location and extenuating circumstances are then considered as far as possible and practical. Due to the availability of clinical placements students may be required to travel up to two hours each way to their clinical site. Where there are extenuating circumstances the Practice Placement Cocoordinator must be informed. Placement Information and Process The School endeavours to place students as early as possible with the academic year. The aim is to inform students at the earliest opportunity and where possible in anticipation of the upcoming year/ practice module. However, with placement shortfalls the School is not always in a position to do this. Students will be kept informed of progress with placements and allocation via announcements on Student ‘Study Space’. Requests and offers for placements are managed by the Placement Management Partnership (PMP). See e-Appendix 6 at http://www.healthcare.ac.uk/courses/rehabilitation-sciences/information-for-preregistration-physiotherapy-practice-educators/ The School’s Practice Education Team requests placements via PMP up to one year in advance. The team allocates students via PMP and students are informed directly via email from the PMP where they are placed. The allocation system is not full proof e.g. following initial allocations placements can be cancelled by provider placement sites at short notice; students may have to cancel a placement; placement allocations may need to be swopped across the student cohort. It is the student’s responsibility to check their email account regularly and keep their contact details up to date with the Undergraduate (Physiotherapy) Programme Administration office (room 72) and registry (Ground Floor Hunter Wing). Remember also, if circumstances change e.g. childcare, the Administration Office must be informed. The School recommends the student contacts the placement site at the earliest convenience via the contact details on the PMP email – unless the specific site information via the PMP support website says otherwise – for information, pre-requisites and guidance in preparation for the placement e.g. 1. If a SMART card is required the process the student must follow to acquire this. NB this can take several weeks. 2. What preparation is required pre placement e.g. reading. The PMP email also provides a link to their support site for placement information. 66 Audit of Placements The Universities involved in the PMP system have collaborated to produce common audit forms for Practice Educators and students. Both Practice Educator and students evaluate the practice placements. Students are requested and prompted by PMP to complete the Student Placement Feedback form after every placement. Feedback is anonymised, valued and important in helping the University and the placement providers evaluate and develop good practice. Placements are audited annually in line with quality and contract performance indicators and standards. This process is also facilitated by the PMP system. The School anticipates that all stakeholders undertake these audits. Thank you. The PMP – in summary: • A web-based system for all London Allied Health Profession students • Has the capacity to use the student’s term-time postcode from the SGUL student database to assist placing student close to placement where possible • All students will have individual log-in access to • View allocated placements • Complete placement feedback questionnaires • Individual log-in access via password, will be emailed to all students • Automatic email tells the student to log on when placement allocated/changed • Pre-placement information via providers on the PMP website Key PMP Contacts Charlotte Adams Placement Management Partnership Consultant (Physiotherapy) Placement Management Partnership Consultancy Team Phone: 0844 811 5037 charlotte.adams@tribalgroup.com E-mail: support.pmpartnership@tribalgroup.com Website: www.pmpartnership.org.uk Practice Educator Study Days The London group of Universities collaborate to organise a series of study days over the academic year to support both new and experienced Practice Educators. The dates for these CPD events are posted on the PMP system https://www.pmpartnership.org.uk/PlacementProvider_Pages/Documents.aspx?placem entproviderid=1246 and on the faculty website at http://www.healthcare.ac.uk/schools/rehabilitation-sciences/practice-resources/ 67 For information on the Study Days at Kingston University / St George’s, University of London (held at St George’s Hospital site) please contact the Programme Administrator Faye McGill placementteam@sgul.kingston.ac.uk Broad areas covered in the Practice Educators’ Study Day include: Physiotherapy pre-reg content, the practice curriculum placement allocation process, practice education resources, contacts Roles and responsibilities Common assessment form Setting learning outcomes and expectations Evaluation Teaching and planning on placement, models of supervision Disability The failing student Productivity Emerging practice education settings Reflection in practice Transferable skills Reflective practice Bespoke study stays are also available for individual practice sites on request, please contact the Placement Co-ordinators for more details. 68 Travel, Claims and Other Relevant Documentation Travelling to the placement – Student advice It is the student’s responsibility to find the best route to the placement. The School recommends www.transportdirect.info www.nationalrail.co.uk and www.tfl.gov.uk for travel information. Alternatively National Rail Enquiries on 08457 48 49 50 or London Travel Information on 0207 222 1234. If travelling to practice placement by car students must be appropriately insured i.e. cover for business use. Travel claims Travel Claim forms can be found outside the Pre-reg Programme office. Completed forms – with receipts – must be returned via the black box provided outside the Pre-reg programme office, designated for this specific purpose. Copies of all travel claims and relevant receipts must be retained. Queries about payment of travel claims should be addressed with the Faculty Finance Officer. Please email PaymentsNB@kingston.ac.uk or by telephone 020 8417 6401 Students can claim for journeys undertaken by public transport, car, motorbike or bicycle between their term time residence and a clinical placement site providing the cost is in excess of their normal daily travel costs from their term-time residence to their college i.e. the difference in travel costs incurred when attending placement rather than teaching/ attending the School of Rehabilitation Sciences. Please see http://www.nhsbsa.nhs.uk/816.aspx A worked comparison example is featured below. Reason for Travel Cost incurred Home to teaching site Home to placement site £12 Cost reimbursed £20 £8 The NHS bursary scheme states that daily travelling costs between the term-time residence and college is included in the basic bursary. If the student is not incurring any additional cost whilst travelling to the clinical placement site he/ she is not out of pocket as the money has already been provided. Steps to follow 1. Claim travel expenses from the Faculty using the green forms available outside the Pre-reg programme office, Level Two Grosvenor Wing 69 2. The cheapest form of transport to travel to and from placements (including free/ concessionary schemes) must be used. All supporting documentation/ receipts must be submitted with the travel claim form (receipts stapled to the claim form) 3. Excess travel expenses will be reimbursed monthly and claims should be sent in as soon as possible, on a monthly basis and NOT three monthly, termly or yearly. Forms completed outside the deadline of 3 months from incurring the expenditure may not be paid 5. A clear justification for travel will quicken the process 6. It is the sole responsibility of the student to retain a photocopy of the claim form and all supporting documentation/ receipts. Occasionally receipts may be lost, if there are no photocopies of the receipts no claim can be made 7. All travel claim forms must include a St George’s Student I.D number, a current address, bank details and the student’s signature. If any of this information is missing the form will be returned to the School office causing a delay in the claim 8. All travel claim forms must be placed in the black box outside the Pre-reg Programme office. They will be collected by the Programme Administrator before forwarding to the Faculty Finance Office. To ensure prompt payment they need to be put in the black box by the 5th of each month 9. Queries about payment of travel claims should be addressed with the Faculty Finance Officer. Please email PaymentsNB@kingston.ac.uk or by telephone 020 8417 6401 Accommodation whilst on placement In some situations it is not feasible for students to travel to and from a placement on a daily basis and accommodation local to the clinical site may be advisable. For example if a student has to travel more than two hours in one direction on public transport or if it is impossible to get to the clinical site on time using public transport. Some practice provider sites offer accommodation and this information can be found on the provider information sheet. Enquires must be made at the earliest opportunity if local accommodation may be necessary. In the first instance this should be discussed with the Practice Placement Co-ordinator. Queries around reimbursement entitlements are available from the Faculty Finance Officer. Please email PaymentsNB@kingston.ac.uk or by telephone 020 8417 6401. 70