GI Physiology -Five major functions of the GI system:
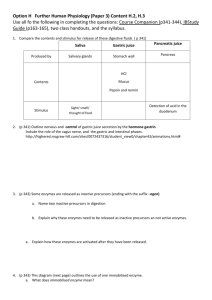
advertisement

GI Physiology -Five major functions of the GI system: -Ingestion -Mastication -Deglutition -Digestion (mechanical, chemical) -Absorption -Elimination -The GI tract is essentially one long tube -Tract organs - mouth, pharynx, esophagus, stomach, intestines, etc -Accessory organ - connected to tract by ducts - salivary glands (parotid), gall bladder, pancreas, liver, etc -Blockages of the ducts cause dysfunction of GI system -All tract organs are isolated from each other by sphincters -One exception: ileosecal valve - strongest in the body -The GI tube itself has (four or) five layers or tunics, listed below from outer to inner: -Serosa: Functions to protect the structures from other structures in the region -Muscularis layer - Longitudinal Muscle Fibers: Parallel the tract - when they contract, they shorten the tube - Circular Muscle Fibers: When they contract, they segment the tube -Submucosal Layer: absorption, secretion, well-endowed with nerves and blood vessels -Mucosal Layer: in contact with the contents of the lumen, secretion, absorption, protection of the tract Enteric Nervous System -Unique set of neurons located within the walls of the tract from esophagus to anus -Consists of two layers of neurons: -Myenteric plexus (Auerbach's plexus) - located between circular fibers and longitudinal fibers -Controls tract movement -Submucosal layer - located in submucosa - associated with stimulating secretory activity in the tract, sensory functions -ANS function: -Parasympathetic innervation of the tract (except for a few fibers that go to the mouth and larynx) is via CNX (Vagus) -These fibers provide innervation to the esophagus, stomach, pancreas, and the first half of the large intestine, to small degree small intestine -Sacral parasympathetic arises from S2, S3, S4 - innervate the distal half of the large intestine, including the -sigmoid colon, anal regions -Increase in parasympathetic activity increases activity of the GI tract -Sympathetic innveration of the tract arise from the sympathetic chain between T8-L2 -These fibers go to all parts of the tract (unlike parasympathetic fibers) -Primary NT is nor epinephrine -Increase in SNS activity serves to decrease activity -- strong SNS innervation can totally block GI activity Reflexes associated with GI activity -Categorized based on where reflexes originate -Distention is a key player - triggers nerves within the walls of the tract -1) Within the entire enteric system - control GI secretions, regulate peristalsis, regulate mixing contractions (no propulsion), and perform some local inhibition -2) Involve a loop between the gut and the prevertebral sympathetic ganglia along thorax and lumbar vertebrae and then back to the gut -Gastrocolic reflex involves originates in the stomach to the colon and causes us to have the urge to evacuate the colon as the stomach fills - type of defecation reflex -Enterogastric reflex initiates in the entero (SI) and proximal part of L intestine, acts on the stomach to cause a decrease in gastric motility and secretions -Colonoileal reflex prevents ileal emptying into the colon when the colon is full -3) Between the gut and the CNS (brainstem) - among these are reflexes that control gastric, motor and secretory activity, pain reflexes that cause a decrease in GI motility, and the defecation reflex producing powerful colonic, rectal, and abdominal contractions -Two classifications of functional GI movement are mixing movements and propulsive movements: -Mixing movements - result of alternating contractions between longitudinal and circular muscle contractions -Propulsive movements (peristalsis) - contraction ring moving along the tube -Distention is the most common stimulus for peristalsis -Ring of contraction about 2-3cm above the area of distention coupled with relaxation 2-3 cm below -*Atropine is a drug that paralyzes cholinergic activity, completely blocks peristalsis -Able to move both ways, but dies out when going upward bc the myenteric plexus polarizes in an anal direction -Law of the gut - ensures analward movement during peristalsis. -Mastication or chewing begins mechanical digestion -Esp important in breaking down cellulose (fruits and vegetables) -Deglutition (swallowing) 1) Voluntary stage which involves moving the bolus of food back towards the or pharynx 2) Pharyngeal stage - involuntary - swallowing receptors near the beginning of the pharynx -When stimulated by the bolus, they trigger a series of reactions as follows: -Elevation of the soft palate (covers nares, preventing reflux into nose), elevation of the vocal cord and hyoid bone (epiglottis covers the larynx, directing bolus into esophagus), relaxation of the upper esophageal sphincter in the upper 3-4cm of the esophagus (allows food to enter esophagus) + contraction of superior constrictor muscles of the pharynx (initiates peristalsis, pushes bolus into esophagus) -Sensory portions of CNV and IX transmit impulses that originate in sensitive areas in the tonsillar pillars @ the opening of the pharynx - transmit impulses to the medulla -Once impulses reach medulla, the swallowing center takes over, orchestrates an orderly sequence of neuronal and mechanical activity, forcing bolus down into stomach -Swallowing center in medulla inhibits respiratory center 3) Esophageal stage - primarily peristalsis, pushing bolus toward lower esophageal sphincter - 2-4 cm above the junction of the stomach and esophagus -Primary function of the sphincter is to prevent reflux of stomach contents and proteolytic enzymes into the esophagus -Stomach is responsible for storing large quantities of food, mixing food w/pepsin and other digestive enzymes, slow expulsion of food into small intestine -Food becomes white, milky, viscous substance called chyme when it leaves the stomach Factors that regulate gastric emptying -Degree of distention of stomach is a major stimulus for regulating the strength of antral contractions (antrim = distal part of the stomach proximal to pyloric sphincter) -Secretion of gastrin from the antral mucosa increases the strength of antral contractions and inhibits the pyloric sphincter, promoting gastric emptying -Several duodenal factors that inhibit gastric emptying: -Degree of duodenal distention, irritation of the duodenal mucosa, the pH of the duodenal chyme (acidic chyme = decreased gastric emptying), high concentration of fat (and protein), hormonal feedback mechanisms from duodenum (stimulated by the presence of fat in the chyme) -These hormones travel in the vascular system - called the enterogastrones decrease gastric activity -Cholecystekinin (CCK) released as a result of fatty chyme, inhibits action of gastrin -Secretin - released by duodenal mucosa, decreases gastric motility -GIP (Gastric inhibiting peptide) - released by duodenal mucosa, decreases gastric motility -Movements in the small intestine are generally mixing actions triggered by distention (myenteric plexus) -Peristaltic waves in SI (very slow) - net movement of the contents of the SI averages 1 cm per minute -Takes bt 3 and 5 hours for passage of chyme from pylorus to ileosecal valve -At the end of the SI (ileum), is the ileocecal valve - primary function to prevent backflow of fecal material from the colon to the ileum -It is the only valve in the GI tract and is the strongest valve in body -Movements in the colon are also sluggish - allows time for reabsorption of water and electrolytes -Only 80-150 mL of original chyme are left (out of 1500 mL) Secretory Activities of the GI tract -Two major functions of secretions: -Lubrication of tract (mucus) -Secretion of digestive enzymes for chemical digestion -The entire tract has varying concentrations of lubricating goblet cells - protect the walls of the tract, esp from proteolytic enzymes -The primary stimulus for secretion is distention -submucosal plexus is associated w/secretion, distention puts direct pressure on those neurons -Tactile stimulation - activates the ANS to stimulate secretory activity; also hormones (CCK and secretin) -Mucus functions to lubricate the wall of the tract, assists in adhering food particles together, buffering effect -Highly resistant to activity of digestive enzymes -First major secretion is saliva: -Glands - submandibular, submaxillary, parotid, etc -Contains salivary amylase or ptyalin - starch digesting enzyme, mucus, electrolytes (HCO3, etc), along with two bacteriocidal substances (thiocyonate and lysozyme - kill bacteria in food), antibodies that kill oral bacteria -Individuals that do not have sufficient salivary production are prone to cavities, ulcerations, infx in the mouth -Saliva secretion is associated with CNVII and CNIX -Carbohydrate digestion begins in the mouth -Esophageal secretion: there are NO digestive enzymes found in esophageal secretions, only mucus to protect the tube and facilitate movement -There is, digestion occurring in the esophagus as a continuation of the oral digestion of starch -The gastric mucosa most complicated - extra structures -Thick mucus that is s&s by the goblet cells -Oxyntic (gastric) glands - s&s pepsinogen, the intrinsic factor (Vitamin B12 absorption in intestine) -Pyloric glands - s&s pepsinogen and gastrin -Chief cells - s&s pepsinogen -Oxyntic (Parietal cells) -s&s HCl -Pepsinogen is activated by HCl into pepsin - proteolytic enzyme that works in a pH range of bt 1.8 and 3.5 -Pepsin is only enzyme in the body to work at such a low pH (others need normal or slightly basic pH) -Begins protein digestion -Gastric secretion - vagal trunks - stimulate the enteric nervous system, gastrin release by distention of the stomach -Review the biliary tree, including the pancreatic duct and common bile duct coming together to form the hepatopancreatic duct swelling = hepatopancreatic ampulla - drain into duodenum through the sphincter of Oddi -Pancreatic juice contains enzymes for digesting proteins, carbons, and fats -S&s by pancreas in their INACTIVE form -Trypsinogen activated when it gets into SI into trypsin by enterokinase -Enterokinase is s&s by duodenal mucosa -Chymotrypsinogen activated by trypsin to give chymotrypsin -Procarboxypeptidase activated by trypsin to give carboxypeptidase -Trypsin and chymotrypsin lyse proteins into tri- and dipeptides -Carboxypeptidase breaks the ensuing polypeptides into amino acids -Completion of protein digestion to amino acids occurs in the duodenum as a result of the pancreatic proteases -Activation should not take place until reaching the duodenum -Pancreas also secretes a trypsin inhibiting factor - prevents conversion of trypsinogen until reaching the duodenum -If trypsinogen is activated into trypsin before the duodenum (insufficient inhibiting factor, blockage in the pancreatic duct) enzymes can digest the pancreas within 4-5 hours -The pancreas also secretes pancreatic amylase digests carbohydrates to disaccharide level (incomplete digestion) -Pancreatic lipase: digests fats into free fatty acids and glycerol - long process - facilitated by bile (complete) -Regulation of pancreatic juice secretion is neural and hormonal mechanisms: -Neural more significant: presence of chyme in the duodenum triggers duodenal secretion of secretin, CCK in varying amounts -Secretin does not stimulate the cells in the pancreas that secrete digestive enzymes, but does cause release of pancreatic juice w/high concentration of bicarbonate ions -Released in response to chyme with a low pH -Bicarbonate neutralizes the acidic chyme -CCK is released by duodenal mucosa - triggers pancreatic juice release w/high conc of pancreatic enzymes facilitates digestion in the duodenum -Gastrin release in the stomach (which increases gastric motility and facilitates gastric emptying) also affects the pancreas in the same way that CCK does -Bile is produced constantly by all hepatic cells -Drains through hepatic ducts cystic duct gall bladder where it is stored and concentrated -Total secretion of bile by the hepatocytes is bt 700 and 1200 mL per day -Max volume of gallbladder: 65-75 mL -Bile @ gallbladder is concentrated (water reabsorbed, leaving behind the main constitutents - bile salts, small amt of cholesterol, lecithin, bilirubin) -For the gall bladder to empty, the sphincter of Oddi relaxes - gallbladder contracts - caused by CCK -Bile emulsifies fat so that the water based digestive enzyme has greater surface area on which to work on -Bile salts also help in the absorption of fatty acids bc they form small complexes w/lipids called micelles -Highly soluble, absorbed through duodenal mucosa -Without bile salts, 30-40% of lipids are lost and excreted in the feces -When fat is not absorbed adequately, there is a deficiency in the fat soluble vitamins - A, D, E, K -A, D, E stored by body; K is not stored - without adequate absorption, the liver cannot synthesize many of the important clotting factors (prothrombin, Factors VII, IX, X) -Under abnormal conditions, cholesterol can precipitate out, causing gallstones (also caused by too much reabsorption of water, lecithin or bile salts from the bile) -Secretions of the SI is primarily mucus in response to distention, tactile stimulus -There are NO digestive enzymes secreted by the SI into the lumen -Digestive enzymes are found in the cells that line the SI - break down disaccharides into monosaccharides -Sucrase digests the disaccharide sucrose into two monosaccharides -Fructose and glucose -Maltase digests maltose into two glucose molecules -Lactase digests lactose into glucose and galactose -The secretions of the large intestine is primarily mucus - compacts fecal matter, protects the wall of the LI -Absorption occurs as a result of increased surface area as needed -Wall of the SI is highly modified to increase surface area to facilitate absorptive process -Villi, microvilli - collectively increase area by 20 fold -Surface area of SI is approx 250 square meters -Each villus contains extensive capillary networks between arterioles and venuoles -Surrounds a central lacteal for the reabsorption of lymph -Vascular system to transport of absorbed material to the liver -Reabsorption can be passive or active - along the cells of the SI are many mitrochondria for ATP synthesis to drive the active reabsorption -In addition to nutrients, electrolytes are reabsorbed, along with disaccharides, amino acids, free fatty acids, glycerols -90% of water and electrolytes that passes through ileocecal valve is reabsorbed - occurs in the proximal half of the colon -Distal half of the LI is primarily for the storage of fecal matter before it is eliminated