MS Word - MDC Repository
advertisement

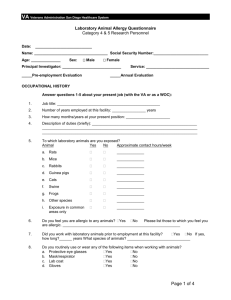
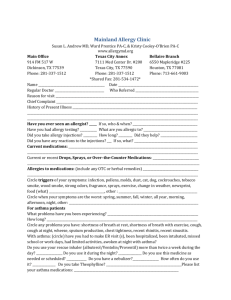
Online Repository Material: Text Content: Methods Description of studies in discovery and replication study Methodological consideration related to genome-wide interaction studies In utero smoke exposure GWIS - Details on the 27 SNPs in the discovery sample with a Pvalue<10-4 Childhood tobacco smoke exposure GWIS - details on the 31 SNPs in the discovery sample with a P-value<10-4 References Acknowledgements 1 Methods Subjects Data from nine individual studies were included in two meta-analyses: a meta-analysis on the interaction between single nucleotide polymorphisms (SNPs) and in utero smoke exposure and a meta-analysis on the interaction between SNPs and childhood smoke exposure (Table E1, Online Repository). All cases and controls were of European descent and two studies had a family structure. We focused on childhood onset asthma, because this disease has a strong genetic background interacting with environmental exposures. Childhood onset asthma was defined as asthma diagnosed by a doctor before the age of 16 years, which is consistent with the definition in the GABRIEL consortiumE1. In utero tobacco smoke exposure was defined as ‘exposure to maternal tobacco smoking at any time during pregnancy’. Childhood tobacco smoke exposure was defined as ‘exposure to passive tobacco smoking at any time from birth until 16 years of age’. Details on the outcome and exposure definition for the individual studies are provided in the Tables E1 to E4 (Online Repository). Genotyping and quality control Genotyping was carried out using the Illumina Human610 quad array (www.illumina.com) at CEACentre National de Génotypage, Evry, France. Details on the genotyping method have been described previously.E1 We restricted our meta-analyses to SNPs fulfilling the following quality control criteria in each study: genotype missing rate <3% in cases and controls, minor allele frequency >5% in controls and consistency with Hardy-Weinberg equilibrium in controls (P-value>10-4). Samples were considered with >95% genotyping success rate. We excluded putative non-European samples, identified using EIGENSTRAT2.0 software. Statistical analyses The effects of in utero tobacco smoke exposure and childhood tobacco smoke exposure were analyzed separately. All individual studies were analyzed using a logistic regression model containing the genetic effect, the effect of tobacco smoke exposure and an interaction term indicating the interaction between the genetic effect and tobacco smoke exposure. This way deviation from a multiplicative model is tested. Gender, age and informative principal components for within-Europe 2 diversity were included as covariates. For the studies containing family data, a cluster variable indicating the family relations was included. An additive genetic model was fitted to the data. For the discovery meta-analysis, we meta-analyzed the estimate of the interaction term of the individual studies. We calculated pooled interaction odds ratios (ORint) and 95% confidence intervals (CI) assuming a fixed effect model and a random effect model. A test for heterogeneity between studies was based on the Cochran’s Q statistic. We selected SNPs with an interaction P-value <10-4 based on the fixed effect model, and without heterogeneity (P-value Q-statistic <0.05) for follow-up in a replication set. Genome-wide significance would be reached at a P-value <9.3*10-8 with the number of SNPs tested. Our threshold for further follow-up was an arbitrary chosen P-value of <10-4 based on the number of SNPs meeting that threshold to select SNPs for the replication study. The selected SNPs were tested in a replication study consisting of four independent studies (Description of studies see Tables E1 to E4, Online Repository) and we meta-analyzed these in the combined set of discovery and replication cohorts as well. The effect of the selected SNPs among exposed and unexposed separately was also calculated in a stratified analysis. Analyses were conducted using Plink 1.07E2 and RE3. For annotation and inspection of linkage disequilibrium (LD) patterns WGAviewerE4 was used. A network analyses was performed for the SNPs with the largest interaction effect using GeneMANIA algorithm (www.genemania.org) to inspect a possible common pathway. 3 Description of studies in discovery and replication study British 1958 birth cohort (B58C) The 1958 British birth cohort is an ongoing follow-up of persons born in Britain during one week in 1958 (http://www.b58cgene.sgul.ac.uk/). At age 44-45, a full biomedical examination was performed from which DNA samples were prepared for use as a nationally representative reference series for genetic case-control studies.E5 About half of the cohort members with a history of asthma ascertained at any age up to 42 years, and a similar number of non-asthmatic controls, were included in the GABRIEL meta-analysisE1. For the purpose of this interaction analysis, childhood asthmatics were defined as persons reporting asthma ever at any follow-up whose parents also reported that they had asthma and/or wheezy bronchitis at any age up to and including 16 years. Maternal smoking after the fourth month of pregnancy was ascertained by interview with a midwife shortly after birth. Postnatal smoke exposure was ascertained from interview questions about maternal smoking and paternal smoking, administered at the 16-year follow-up. ALSPAC The Avon Longitudinal Study of Parents and Children (ALSPAC) is a population-based, birth cohort recruited during pregnancy. Pregnant women resident in Avon, United Kingdom with estimated dates of delivery between 1st April 1991 and 31st December 1992 were recruited through antenatal clinics. E6 From 14,451 women recruited, there were 14,072 live births and 13,988 children were alive at age one year. Children were followed from birth using self-completion questionnaires sent to their mothers at approximately annual intervals and, from 7 years of age, in yearly dedicated research clinics. Asthma is defined as an affirmative answer to a question at 91 months (approximately 7½ years), “Has a doctor ever told you that your child had asthma?” Data on passive smoke exposure in utero was collected from questionnaires sent to mothers during pregnancy at 18 weeks gestation. Postnatal exposure was derived from two questionnaires sent to mothers 5 or 6 times between 6 months and 78 months after birth. In utero smoke exposure was defined as “The mother smoked regularly in first 3 months of pregnancy (>1 cig/day)”. Childhood smoke exposure was defined as a positive response at any time to “The mother smokes regularly (>1 cigs/day currently smoked)” or “The child is exposed to a room or enclosed place where people are smoking during weekdays or weekends”. A total of 3,030 4 children had DNA available for genotyping and data on asthma at 91 months as well as other asthma related phenotypes. Of these, 625 (20.6%) had asthma and an equal number of controls was selected at random from the remainder. After ALSPAC-QC a total of 1,139 subjects were retained in the GWI study analysis on in utero smoke exposure and 1,025 subjects were retained in the GWI study analysis on childhood smoke exposure. BAMSE Between 1994 and 1996, 4,089 newborn infants were recruited in the BAMSE study, and questionnaire data on baseline study characteristics were obtained.E7The catchment area included central and north-western parts of Stockholm. At approximately one, two, four, and eight years of age, parents completed questionnaires on their children’s symptoms related to asthma and other allergic diseases. The response rates were 96%, 94%, 92% and 84%, respectively. At eight years of age, all children of the BAMSE study were invited to clinical testing where blood samples were obtained from 2,480 children. DNA was extracted from 2,033 samples after exclusion of samples with too little blood, lack of questionnaire data, or if parental consent to genetic analysis of the sample was not obtained. From these samples, all children with a doctor’s diagnosis of asthma (ever) were selected as cases and children with no history of asthma or other allergic diseases were selected as controls. Data on passive smoke exposure was collected from repeated questionnaires filled out by parents. In utero smoke exposure was defined as “The mother smoked at least one cigarette per day in any point of time during the pregnancy” as reported in the baseline questionnaire at approximately 2 months. Childhood smoke exposure was defined as “Any of the parents smoked at least one cigarette per day” at the time of any questionnaire, distributed at 2 months, 1, 2, 4 and 8 years. After genome-wide data QC and exclusion of subjects with missing values on smoke exposure a total of 484 subjects were retained in the GWI study analyses. ECRHS Sixteen centres (eight countries) in the European Community Respiratory Health Survey (ECRHS) have contributed samples to GABRIEL (http://www.ecrhs.org).E8,E9 In each centre, a representative community-based sample of at least 3000 adults aged 20-44 years were invited to complete a brief postal questionnaire asking about respiratory symptoms (ECRHS I - Stage 1) between 1991-1993. A 5 random sample of these (600 per centre) underwent intensive further investigation (ECRHS I - Stage 2 – random sample). Participants who had symptoms highly suggestive of asthma but who had not been selected at random to take part in Stage 2, were also invited to undergo intensive investigations (ECRHS I - Stage 2- enriched sample). About ten years later all adults who had taken part in Stage 2 were recontacted (ECRHS II) and again asked about respiratory symptoms. Samples suitable for DNA extraction were collected. For the GABRIEL initiative all cases of asthma were identified (participants from the random or enriched sample who said yes to the question „Have you ever had asthma? at either ECRHS I or ECRHS II). Controls were a random sample who answered “no to the same question in both surveys”. In utero smoke exposure was defined as any smoking by the mother during pregnancy. Childhood smoke exposure was defined as either mother or father smoked regularly during childhood (ECRHS1 main questionnaire). EGEA EGEA is a 12-year longitudinal survey which combines a case-control study and a family study (http://cesp.vjf.inserm.fr/~egeanet). The first survey (EGEA1) took place between 1992 and 1995.E10 The study population included 388 asthmatics recruited in chest clinics and their 1,244 family members plus 415 population-based controls (total of 2,047 subjects). The probands (asthmatics and controls) were between 7 and 70 years old at time of study. All probands and their two parents were of European ancestry and were born in France. The second survey (EGEA2) was conducted between 2003 and 2007 and included follow-up data in 1,543 subjects from the initial cohort and 58 new family members.E11 Data collected through face-to-face interviews and examination included extensive phenotypic characterization (detailed clinical data based on standardized questionnaire, skin prick tests, lung function tests, bronchial responsiveness, blood samples, white blood cell counts, total IgE), data on risk factors (environmental exposures, diet, physical activity, hormone-related events) and drug consumption. For the GABRIEL initiative, asthma was defined by a positive answer to the question "Have you ever had asthma attack "at EGEA1 (or at EGEA2 if not examined at EGEA1). In utero smoke exposure was defined in adults as an affirmative answer on the question “When your mother was pregnant, in particular with you, did she stop smoking during pregnancy?” Childhood smoke exposure was defined as an affirmative answer on either question “Did your mother ever smoke during your childhood (before 16 years old)?” or “Did your father ever smoke during your 6 childhood?” (for adults) and “Did his/her mother ever smoke when he/she was younger than 2 years?” or “Did his/her father ever smoke when he/she was younger than 2 years?” or “Did his/her father or mother or someone smoke in the household at the time of the questionnaire in EGEA1?” (for children). GABRIELA The GABRIELA study was carried out as a population survey in five rural regions of Europe: BadenWürttemberg and Bavaria in Germany, North/Central Switzerland, Tyrol in Austria, and Lower Silesia in Poland. The Polish center was not included in the GWI study analysis. Children aged 5-13 years were recruited through primary schools. A recruitment questionnaire was sent out to 132,366 children, of whom 79,888 (60.4%) returned their completed questionnaires (phase 1), containing questions on asthma. Of these children, 34,491 were eligible for phase 2 as defined by a documented parental consent to dust sampling, blood sampling, and genetic analyses and nationality of their study country. To enrich informative observations a stratified random selection process was applied in two steps. In a first step, 9,668 children were selected for phase 2 within the three exposure strata per center. In the second step, 1,708 children were selected for genotyping within exposure and outcome strata per center. In utero smoke exposure was defined as any smoking by the mother during pregnancy. Childhood smoke exposure was defined as current smoking by the father or the mother. Details on the study design are described in: Genuneit J et al., The GABRIEL Advanced Surveys: study design, participation, and evaluation of bias.E12 PIAMA The PIAMA study is a birth cohort study of children born between 1996-1997. Details of the study design have been published previously.E13 10,232 pregnant women completed a validated screening questionnaire at their prenatal health care clinic (n=52). Based on this screening, 7,862 women were invited to participate, of whom 4,146 women agreed and gave informed consent. Mothers reporting a history of asthma, current hay fever or allergy to pets or house dust mite were defined as allergic. Children were recruited during the first trimester of pregnancy. Follow-up of the children took place at 3 months of age and yearly from 1 to 8 years of age. At eight years of age, all children were invited to clinical testing including collection of blood samples for DNA extraction. The Medical Ethical Committees of the participating institutes approved the study, and all participants gave written 7 informed consent. The response rates to the annual questionnaires ranged from 3764 at age 1 to 3269 at age 8 years. For the GWI study, DNA from childhood asthma cases (children who have ever had a doctor’s diagnosis of asthma at age 8 years) and a set of non-asthmatic controls (children who never had a doctor’s diagnosis of asthma and who have never wheezed at age 8 years) were provided. In utero smoke exposure was defined as any smoking by the mother during pregnancy from week 4 of pregnancy. Childhood smoke exposure was defined as any smoking by the father or the mother inside the house between the child’s birth and 8 years of age. SAPALDIA SAPALDIA contributed all self-reported asthma cases as well as a random sample of controls. These subjects were obtained from among 6,055 SAPALDIA cohort subjects that participated in both, the baseline (1991) and follow-up (2002) examinations and agreed to providing blood for genetic analysis. SAPALDIA is a population-based cohort that originally recruited subjects aged 18 to 60 from population registries in eight Swiss communities representing the three largest language groups (German, French, Italian) as well as different levels of air pollution, altitude and degrees of urbanization. At both baseline and follow-up examination subjects underwent spirometry as well as a detailed interview on respiratory health, smoking history and lifestyle factors. At follow-up, 8,047 of 9,651 baseline subjects re-participated in at least one part of the study and a formal biobank was established. SAPALDIA questions about smoking and asthma status were equivalent to those used by the ECRHS. Asthma status was defined by an affirmative answer to the question “Have you ever had asthma” at baseline and/or follow-up interview. Childhood smoke exposure was defined as positive answer to either of the questions “Did your father regularly smoke when you were a child?” or “Did your mother regularly smoke when you were a child?”. In utero smoke exposure was present when the person’s mother either continuously smoked, or reduced or stopped smoking during pregnancy. Exposure during pregnancy was asked upon affirmatively answering the question on regular smoking of the mother during the person’s childhood. TOMSK TOMSK is a population-based family study conducted by the Research Institute of Medical Genetics and Siberian State Medical University (Tomsk, Russia) from 1998 onwards. E14 Both nuclear families 8 and extended pedigrees were recruited through atopic bronchial asthmatic probands. All participants were Russians or of a mixed ethnic origin due to marriages between Russians and major East Slavonic populations (Ukrainians, Byelorussians). Altogether, 196 families were studied, out of which 150 families were recruited in Tomsk Region Children Hospital and Tomsk Region Hospital (Tomsk, Russia), and 46 families were recruited in the city of Irkutsk hospitals by the staff of the Irkutsk State Institute of Doctors Advanced Training (Irkutsk, Russia). Both probands and their relatives were clinically examined to establish diagnosis of asthma and atopy by the GINA criteria (Global Initiative for Asthma: Global Strategy for Asthma Management and Prevention. http://www.ginasthma.org). Besides the clinical examination, laboratory and functional testing were conducted to assess common IgE levels (solid-phase immune-enzyme assay), specific sensitization (skin-prick tests), lung volumes (spirometry), and airway responsiveness (bronchoprovocative tests with methacholine). For the GWI study analysis, only children were included. Childhood smoke exposure was defined as an affirmative answer to the question “Are you currently exposed to passive smoking?”. Canadian Childhood Cohorts: CAPPS & SAGE CAPPS was initiated in 1995 to assess the effectiveness of a multifaceted intervention program on the primary prevention of asthma in high-risk infants. Full details have been previously publishedE15 and are available at http://www.genopha.ca/. Infants at high risk for developing asthma and other allergic disorders were identified and their mothers were recruited during their third trimester of pregnancy. Infants at high risk were defined as those who had a parent with asthma or two first-degree relatives with allergies or atopic disorders. The study had two recruitment centers in Canada, (Vancouver and Winnipeg). In total, there were 545 families recruited into the study (549 infants, 4 sets of twins). Loss to follow-up was minimal, with 86% of the families completing the questionnaire at the 7-year time point. For genetic analysis blood samples have been obtained from the children, and both parents. The Ethics Committees of the University of British Columbia and the University of Manitoba approved the study and parents provided written informed consent for participation. Childhood smoking exposure was measured in prospective manner by questionnaires administered to both parents (mother and father) at 7 time-points (prenatally, 2 weeks, 4, 8, and 12 months of life, and at age 2 and 7 years), home visits were conducted and exposure was confirmed by urine cotinine. Specific questions, full questionnaires, and timeline for administration of questionnaires can be found 9 at http://genapha.icapture.ubc.ca/smokingExposure.do#overview, smoking questions were asked of both parents and parents were asked if visitors were allowed to smoke in the home. If a child was exposed during pregnancy they were considered exposed prenatally, if they were exposed at anytime during the follow-up period (first 7 years of life) they were considered exposed during childhood for this analysis. SAGE is a population-based sample of 16,320 children, born in the province of Manitoba, Canada in the year of 1995. The SAGE study design has been previously described in detail. E16 In 2002, a onepage survey was mailed to families to enquire about their health and home environment exposure. Questions included several chronic conditions in childhood, including hay fever, food allergy and asthma. Parents were asked for permission to be contacted for further study and to link the survey data to their child’s health care database records. Children were stratified according to the presence of asthma (n=392), to the presence of hay fever or food allergy (n=192) and neither (n=3,002). Children with neither condition were further grouped by rural and urban location; the latter were further stratified by low and high income neighborhoods. All children in the asthma and allergy strata were invited to participate in the case-control study, as were a random sample (n=200) from the strata of children with neither condition. Childhood smoking exposure was measured retrospectively by questionnaires to both parents (mother and father) when the child was age 7 to 9 (depending on enrollment date). Questions were asked about smoking exposure during pregnancy and after birth to current age (7 to 9 depending on enrollment date) Specific questions, full questionnaires, and timeline for administration of questionnaires can be found at http://genapha.icapture.ubc.ca/smokingExposure.do#overview. If a child was exposed during pregnancy they were considered exposed for the prenatal analysis, if they were exposed at any time after birth they were considered exposed during childhood for this analysis. LifeLines The LifeLines cohort is a three-generation cohort that is designed to investigate universal risk factors and their modifiers for multifactorial diseases.E17 It is an observational follow-up study in a large representative sample of the population of the northern provinces of the Netherlands. Firstly, a random sample of persons aged between 25 and 50 years are contacted through their general practitioner and are invited to participate. Subsequently these probands invite their family members if present to take 10 part as well (parents, partner, parents in law, children), resulting in a three-generation study. At enrollment subjects undergo a medical examination where blood sample is collected for DNA extraction. Participants filled in a questionnaire at baseline containing a question on whether they ever had asthma, whether the diagnosis has been confirmed by a physician and what was the age of onset. Exposure to maternal smoking during pregnancy was defined as any smoking by the mother during pregnancy. Exposure to passive smoking was defined as any regular smoking by the father or the mother during childhood. Genotyping of 301,232 SNPs was performed with using Illumina HumanCytoSNP-12v2 array. Samples for 13,301 individuals were genotyped and passed QC. The data was imputed by BEAGLE 3.0. For the analyses on exposure to maternal smoking during pregnancy, 22 of 27 SNPs were successfully imputed and included in the replication study. For the analyses on passive smoking, 25 of 31 SNPs were successfully imputed and included in the replication study. MAS The MAS/ISAAC study is a combination of the MAS cohort, which contained only asthma cases and the ISAAC cohort, from which we only included the controls. The MAS and ISAAC cohort are both multi centre studies and consist of subjects from Germany. We inspected MDS plots for these cohorts and did not observe population stratification. Not all SNPs selected for the replication study could be included in the replication study, because ISAAC subjects were genotyped using a different platform (GABRIEL phase I) than the other GABRIEL cohorts (GABRIEL phase II). For the GWI study on exposure to maternal smoking during pregnancy, 16 of the 27 SNPs selected for replication could be included in the replication study. For the GWI study on exposure to passive smoking during childhood, 16 of the 31 SNPs selected for replication could be in the replication study. MAS consists of 1,314 healthy mature children born in 5 German cities in the year 1990.E18 All children were followed at the age of 1, 3, 6, 12, 18, and 24 months and at yearly intervals thereafter until age 15 years. Clinical and environmental assessment included standardized interviews, questionnaires, physical examinations, and environmental studies. DNAs from all children with a doctor diagnosis of asthma (ever) or with wheezing/whistling in the chest and the use of asthma medication in the previous 12 months at any time point during follow-up were provided for the GWIS. In utero smoke exposure was defined as any 11 smoking by the mother during pregnancy. Childhood smoke exposure was defined as any smoking at the child’s home or as the child’s exposure to a smoky room elsewhere up to 9 years of age. ISAAC The ISAAC study assessed the prevalence of asthma and allergies in schoolchildren and the asthma status was based on the parent’s report of a physician’s diagnosis of asthma at least once, or of spastic or asthmatic bronchitis more than once in self-administered questionnaires. Written informed consent was obtained from all parents of children included in these studies and study methods were approved by the respective ethics committees. All children were of German origin to control for population admixture. We only used control subjects from the ISAAC study. Data on smoke exposure was collected when the children were between 8 and 12 years of age. In utero smoke exposure was defined as an affirmative answer to the category “during pregnancy” in the question “Does or did the mother of the child smoke?”. Childhood smoke exposure was defined as an affirmative answer to one of the following questions “Is there smoking in the dwelling your child lives in?” or “Did/does the mother smoke?”. 12 Methodological consideration related to genome-wide interaction studies A general problem in GWI studies is their limited power, due to often a small number of subjects with overlapping exposures and genotypes. In our study, only about 15% of the asthma cases were exposed to tobacco smoke in utero resulting in less than 100 exposed cases in most individual studies (Table E1, Online Repository). A way to increase the power to detect an interaction is to assess the association between exposure and genotype in a case-only design or a two-step design.E19, E20 These designs assume that exposure and genotype are independent. We chose not to use these designs given the known strong genetic component for smoking addiction. Relative modest violations of this assumption can have a substantial impact on bias relating to the interaction parameters, E21 and lead to false positive or false negative findings. E22 In a two-step design the interaction is tested among a selection of SNPs. This selection is based on the same assumption that exposure and genotype are independent. The method we used to detect interactions between exposure and genotype did not assume exposure and genotype independence nor did we a priori select SNPs. To increase the power of our analysis we first selected the most promising SNPs using an arbitrary threshold for interaction <10-4 and included them in a replication study. A similar approach has been used recently in a GWI study on interaction between genetic markers and waist hip ratio on total serum cholesterol. E23 Another difficulty with combining multiple studies by meta-analysis is the difference in exposure and outcome definition between studies. The studies included in this GWI study differed in definition of smoke exposure and childhood asthma, the timing of the ascertainment of exposure and outcome (for instance prenatal or postnatal data collection on maternal smoking) and methods (questionnaire or interview). These differences between individual studies are inevitable in a meta-analysis and although they may not bias the results, they could create random error which makes it harder to detect a significant interaction. E24 In addition, due to retrospectively self-reported or parental reported passive smoke exposure children may have been misclassified according to their passive smoke exposure leading to an underestimation of the exposure effect. A GWI study has the advantage that it is specifically suited to identify novel SNPs that interact with an environmental exposure in an unbiased way. In contrast to a GWI approach, a GWA approach will not identify modest genetic effects that evolve into disease expression only in the presence of a given exposure, or even after overriding a specific threshold of this exposure. Large interaction effect 13 estimates, as observed in our GWI study, are due to the fact that the genetic effect in exposed versus non-exposed subjects is often in opposite direction. As a result, the effect of the genetic variant is attenuated in the total population when exposed and non-exposed subjects are analyzed together, like in a regular GWA study. Thus genetic effects may be missed in GWA studies because exposed and non-exposed subjects level out their opposite genetic effects. 14 In utero smoke exposure GWIS - Details on the 27 SNPs in the discovery sample with a Pvalue<10-4 We included 27 SNPs in the replication study. None of the interaction of SNPs with in utero tobacco smoke exposure reached statistical significance in the replication study after Bonferroni correction for multiple testing (0.05/27). Three SNPs had a P-value <0.05 based on the fixed effect model, but for rs14398 the interaction was in opposite direction in the replication study as in the discovery study. The largest interaction effect was observed for rs8094633 (discovery meta-analysis: ORint=2.13, 95%CI=1.48;3.06, P-value=4.29*10-5; replication meta-analysis: ORint=2.87, 95%CI=1.09;7.58, Pvalue=0.03) (Table 1). There was no sign of heterogeneity of effects for this SNP and the overall interaction estimate (when all studies were combined) was: ORint=2.21, P-value=4.67*10-6 (Table E5, Online Repository). In subjects with in utero tobacco smoke exposure, carriers of the minor allele C had an increased risk for asthma (OR=1.72, P-value=0.001) while in non-exposed subjects, carriers of the C allele had no increased asthma risk (OR=0.89, P-value=0.05) (Table E5, Online Repository). Leukocytes of smoking subjects express higher EPB41L3 mRNA levels than non-smoking subjectsE25 and modest evidence for association of EPB41L3 gene variants with tobacco smoking habits has been reported.E26 In our data, this SNP was not associated with in utero tobacco smoke exposure or childhood tobacco smoke exposure itself. Therefore the observed interaction is not likely to be explained by smoking addiction of the mother (data not shown). Another interesting SNP that interacted with in utero tobacco smoke exposure in the discovery meta-analysis, but could not be replicated is the SNP near IL5RA (interleukin 5 receptor subunit alpha). IL5Ralpha and IL5Rbeta together constitute the receptor for IL5. IL5RA is amongst others expressed on eosinophils and B-cells and plays an important role in the pathogenesis of allergy and asthma. E27,E28 Polymorphisms in IL5RA have been associated with allergy.E29,E30 The latter studies investigated different SNPs which are not in LD with the marker we found. 15 Childhood tobacco smoke exposure GWIS - details on the 31 SNPs in the discovery sample with a P-value<10-4 We included 31 SNPs in the replication study. None of the interactions of SNPs with childhood tobacco smoke exposure reached statistical significance in the replication study after Bonferroni correction for multiple testing (0.05/31). The largest interaction effect was found for rs1575472 (discovery meta-analysis: ORint=1.78, 95%CI=1.37;2.31, P=1.37*10-5; replication meta-analysis: ORint=1.51, 95%CI=0.99;2.31, P=0.06) (Table 2). The overall interaction estimate (when all studies were combined) was: ORint=1.70, P-value=2.52*10-6 (Table E6, Online Repository). In subjects with childhood tobacco smoke exposure, carriers of the minor allele G had an increased risk for asthma (OR=1.21, P-value=2.72*10-3), while in non-exposed subjects, carriers of the G allele had a decreased asthma risk (OR=0.73, P-value=1.46*10-4) (Table E6, Online Repository). The SNP rs1575472 is located on chromosome 6, intronic of PACRG, parkin co-regulated gene. 16 References E1. Moffatt MF, Gut IG, Demenais F, et al. A large-scale, consortium-based genomewide association study of asthma. N Engl J Med 2010; 363(13): 1211-21. E2. Purcell S, Neale B, Todd-Brown K, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 2007 http://pngu.mgh.harvard.edu/purcell/plink/; 81(3): 559-75. E3. R Development Core Team. R Foundation for Statistical Computing. R: A Language and Environment for Statistical Computing. http://www.R-project.org. 2011; . E4. Ge D, Zhang K, Need AC, et al. WGAViewer: software for genomic annotation of whole genome association studies. WGAviewer Dongliang Ge & David B. Goldstein http://people.genome.duke.edu/~dg48/WGAViewer/. Genome Res 2008; 18(4): 640-3. E5. Strachan DP, Rudnicka AR, Power C, et al. Lifecourse influences on health among British adults: effects of region of residence in childhood and adulthood. Int J Epidemiol 2007; 36(3): 522-31. E6. Golding J, Pembrey M, Jones R. ALSPAC--the Avon Longitudinal Study of Parents and Children. I. Study methodology. Paediatr Perinat Epidemiol 2001; 15(0269-5022; 1): 74-87. E7. Kull I, Melen E, Alm J, et al. Breast-feeding in relation to asthma, lung function, and sensitization in young schoolchildren. J Allergy Clin Immunol 2010; 125(5): 1013-9. E8. Burney PG, Luczynska C, Chinn S, Jarvis D. The European Community Respiratory Health Survey. Eur Respir J 1994; 7(5): 954-60. E9. E10. The European Community Respiratory Health Survey II. Eur.Respir.J. 2002; 20(5): 1071-9. Kauffmann F, Dizier MH, Annesi-Maesano I, et al. EGEA (Epidemiological study on the Genetics and Environment of Asthma, bronchial hyperresponsiveness and atopy)-- descriptive characteristics. Clin Exp Allergy 1999; 29 Suppl 4: 17-21. 17 E11. Siroux V, Boudier A, Bousquet J, et al. Phenotypic determinants of uncontrolled asthma. J Allergy Clin Immunol 2009; 124(4): 681,7.e3. E12. Genuneit J, Buchele G, Waser M, et al. The GABRIEL Advanced Surveys: study design, participation and evaluation of bias. Paediatr Perinat Epidemiol 2011; 25(5): 436-47. E13. Brunekreef B, Smit J, de Jongste J, et al. The prevention and incidence of asthma and mite allergy (PIAMA) birth cohort study: design and first results. Pediatr Allergy Immunol 2002; 13 Suppl 15(0905-6157): 55-60. E14. Freidin MB, Kobyakova OS, Ogorodova LM, Puzyrev VP. Association of polymorphisms in the human IL4 and IL5 genes with atopic bronchial asthma and severity of the disease. Comp Funct Genomics 2003; 4(3): 346-50. E15. Daley D, Lemire M, Akhabir L, et al. Analyses of associations with asthma in four asthma population samples from Canada and Australia. Hum Genet 2009; 125(4): 445-59. E16. Kozyrskyj AL, HayGlass KT, Sandford AJ, Pare PD, Chan-Yeung M, Becker AB. A novel study design to investigate the early-life origins of asthma in children (SAGE study). Allergy 2009; 64(8): 1185-93. E17. Stolk RP, Rosmalen JG, Postma DS, et al. Universal risk factors for multifactorial diseases: LifeLines: a three-generation population-based study. Eur J Epidemiol 2008; 23(1): 67-74. E18. Lau S, Nickel R, Niggemann B, et al. The development of childhood asthma: lessons from the German Multicentre Allergy Study (MAS). Paediatr Respir Rev 2002; 3(3): 265-72. E19. Mukherjee B, Ahn J, Gruber SB, Chatterjee N. Testing gene-environment interaction in large- scale case-control association studies: possible choices and comparisons. Am J Epidemiol 2012; 175(3): 177-90. E20. Ege MJ, Strachan DP, Cookson WO, et al. Gene-environment interaction for childhood asthma and exposure to farming in Central Europe. J Allergy Clin Immunol 2011; 127(1): 138,44, 144.e1-4. 18 E21. Hunter DJ. Gene-environment interactions in human diseases. Nat Rev Genet 2005; 6(4): 287-98. E22. Liu X, Fallin MD, Kao WH. Genetic dissection methods: designs used for tests of gene- environment interaction. Curr Opin Genet Dev 2004; 14(3): 241-5. 23. Surakka I, Isaacs A, Karssen LC, et al. A genome-wide screen for interactions reveals a new locus on 4p15 modifying the effect of waist-to-hip ratio on total cholesterol. PLoS Genet 2011; 7(10): e1002333. E24. Bookman EB, McAllister K, Gillanders E, et al. Gene-environment interplay in common complex diseases: forging an integrative model-recommendations from an NIH workshop. Genet Epidemiol 2011; . E25. Charlesworth JC, Curran JE, Johnson MP, et al. Transcriptomic epidemiology of smoking: the effect of smoking on gene expression in lymphocytes. BMC Med Genomics 2010; 3: 29. E26. Uhl GR, Drgon T, Johnson C, Ramoni MF, Behm FM, Rose JE. Genome-wide association for smoking cessation success in a trial of precessation nicotine replacement. Mol Med 2010; 16(11-12): 513-26. E27. Gorski P, Wittczak T, Walusiak J, Palczynski C, Ruta U, Kuna P, Alam R. Eotaxin but not MCP-3 induces eosinophil influx into nasal fluid in allergic patients. Allergy 2002; 57(6): 519-28. E28. Yasruel Z, Humbert M, Kotsimbos TC, et al. Membrane-bound and soluble alpha IL-5 receptor mRNA in the bronchial mucosa of atopic and nonatopic asthmatics. Am J Respir Crit Care Med 1997; 155(4): 1413-8. E29. Cheong HS, Kim LH, Park BL, et al. Association analysis of interleukin 5 receptor alpha subunit (IL5RA) polymorphisms and asthma. J Hum Genet 2005; 50(12): 628-34. E30. Kabesch M, Depner M, Dahmen I, et al. Polymorphisms in eosinophil pathway genes, asthma and atopy. Allergy 2007; 62(4): 423-8. 19 Acknowledgements ALSPAC We are extremely grateful to all the families who took part in the study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. The UK Medical Research Council and the Wellcome Trust (Grant ref: 093731) and the University of Bristol provide core support for ALSPAC. BAMSE The BAMSE Study was supported by the Swedish Research Council, Stockholm County Council, Centre for Allergy Research, Karolinska Institutet and the Swedish Heart Lung Foundation. Erik Melén is supported by a post doc grant from the Swedish Heart Lung Foundation, the Swedish Fulbright Commission and Riksbankens Jubileumsfond, Erik Rönnberg’s scholarship for research on early childhood diseases. EGEA We thank the EGEA cooperative group: Coordination : F Kauffmann; F Demenais (genetics); I Pin (clinical aspects). Respiratory epidemiology : Inserm U 700, Paris M Korobaeff (Egea1), F Neukirch (Egea1); Inserm U707, Paris : I Annesi-Maesano ; Inserm CESP/U 1018, Villejuif : F Kauffmann, N LeMoual, R Nadif, MP Oryszczyn ; Inserm U 823, Grenoble : V Siroux Genetics : Inserm U 393, Paris : J Feingold ; Inserm U 946, Paris : E Bouzigon , F Demenais, MH Dizier ; CNG, Evry : I Gut , M Lathrop. Clinical centers : Grenoble : I Pin, C Pison; Lyon : D Ecochard (Egea1), F Gormand, Y Pacheco ; Marseille : D Charpin (Egea1), D Vervloet ; Montpellier : J Bousquet ; Paris Cochin : A Lockhart (Egea1), R Matran (now in Lille) ; Paris Necker : E Paty, P Scheinmann ; Paris-Trousseau : A Grimfeld, J Just. Data and quality management : Inserm ex-U155 (Egea1) : J Hochez ; Inserm CESP/U 1018, Villejuif : N Le Moual, Inserm ex-U780 : C Ravault ; Inserm ex-U794 : N Chateigner ; Grenoble : J Ferran. The authors thank all those who participated to the setting of the study and on the various aspects of the examinations involved: interviewers, technicians for lung function testing, coders, those involved in quality control, data management and all those who supervised the study in 20 all centers. The authors are grateful to the three CIC-Inserm of Necker, Grenoble and Marseille who supported the study and in which subjects were examined. They are indebted to all the individuals who participated without whom that study would not have been possible. EGEA sources of funding: INSERM-Ministry of Research 'Cohortes et Collections' grant (4CH06G). French Ministry of Higher Education and Research, University Paris Diderot-Paris 7, grants from the French Agency for Environmental and Occupational Health Safety (grant AFSSETAPR- SE-2004), the French National Agency for Research (grants ANR 05-SEST-020- 02/05-9-97 and ANR 06-CEBS), PHRC-Paris, Merck Sharp & Dohme (MSD)). For the genotyping (as for all Gabriel groups): The GABRIEL genotyping was supported by a contract from the European Commission Framework Programme 6 (018996) and grants from the French Ministry of Research. GABRIELA The members of the GABRIELA study group are in alphabetical order: Silvia Apprich PhDG, Andrzej Boznanski MD, PhDK, Charlotte Braun-Fahrländer MDD,E, Gisela Büchele PhDC, William Cookson MD, DPhilA, Paul Cullinan MDA, Hanna Danielewicz MDK, Anna DębińskaK, Martin Depner PhDB, Markus Ege MDB, Urs Frey MD, PhDR , Oliver Fuchs MDL, Jon Genuneit MDC, Dick Heederik PhDF, Elisabeth Horak MDM, Anne Hyvärinen PhDH, Sabina Illi PhDB, Michael Kabesch MDN, Katalin KovacsM, Aleksandra Kosmęda PhDK, Wolfgang Kneifel PhDG, Philipp Latzin MD, PhDL, Roger Lauener MDP, Georg Loss MScD,E, Stephanie MacNeill MScA, Bernhard Morass MDM, Anne-Cécile Normand PhDQ, Ilka Noss PhDF, Renaud Piarroux MD, PhDQ, Helena Rintala PhDH, Mascha K Rochat MDB, Nikolaos SitaridisC, Barbara Sozanska MDK, David Strachan MDO, Christine Strunz-Lehner MPHB, Bertrand Sudre MD, PhDI, Erika von Mutius MD, MScB, Marco Waser PhDD,E, Juliane Weber MDB, Inge Wouters PhDF A Imperial College London, National Heart and Lung Institute, South Kensington Campus, London SW7 2AZ, United Kingdom. B LMU Munich, University Children’s Hospital, Lindwurmstrasse 4, D 80337, Munich, Germany. C Ulm University, Institute of Epidemiology and Medical Biometry, Helmholtzstraße 22, D-89081 Ulm, Germany. D Swiss Tropical and Public Health Institute, Socinstr. 57, P.O. Box, 4002 Basel, Switzerland. E University of Basel, Petersplatz 1, 4003 Basel, Switzerland 21 F Utrecht University, Institute for Risk Assessment Sciences (IRAS), Division of Environmental Epidemiology, PO Box 80178, 3508TD, Utrecht, The Netherlands. G BOKU Vienna, University of Natural Resources and Life Sciences, Department of Food Science and Technology, Muthgasse 18, A-1190 Vienna, Austria. H THL Kuopio, National Institute for Health and Welfare, PL 95 70701 Kuopio, Finland. I Université de Franche-Comté, UMR 6249 Chrono-Environnement, Département de Parasitologie/Mycologie, UFR SMP, 19 rue A. Paré, 25000 Besançon, France. K Wroclaw Medical University, 1st Department of Paediatrics, Allergology and Cardiology, ul. J.M. Hoene-Wronskiego 13C, 53-376 Wroclaw, Poland. L Division of Pulmonology, Department of Paediatrics, Bern University Hospital, Switzerland. M Department of Pediatrics and Adolescents, Division of Cardiology and Pulmonology, Innsbruck Medical University, Anichstr. 35, A-6020, Innsbruck, Austria. N Hannover Medical School, Clinic for Paediatric Pneumology and Neonatology, Carl-Neuberg-Str. 1, D-30625 Hannover, Germany. O St George’s, University of London, Cranmer Terrace, London SW17 0RE, United Kingdom. P High Mountain Hospital Davos, Herman-Burchard-Str. 1, CH-7265 DavosWolfgang. Q Department of Parasitology and Mycology, Hôpital de la Timone, Assistance PubliqueHôpitaux de Marseille, 13385 Marseille, France. R University Children’s Hospital (UKBB), Spitalstrasse 33, 4056 Basel, Switzerland. PIAMA The PIAMA study was funded by grants from the Dutch Asthma Fonds, the ZON-MW Netherlands Organization for Health Research and Development, the Stichting Astmabestrijding and the Ministry of the Environment and the Netherlands Ministry of Health, Welfare and Sport. SAPALDIA Research support: the Swiss National Science Foundation (grants no 33CS30_134276/1, 33CSCO108796, 3247BO-104283, 3247BO-104288, 3247BO-104284, 3247-065896, 3100-059302, 3200052720, 3200-042532, 4026-028099, 3233-054996, PDFMP3-123171), the Federal Office for Forest, Environment and Landscape, the Federal Office of Public Health, the Federal Office of Roads and Transport, the canton's government of Aargau, Basel-Stadt, Basel-Land, Geneva, Luzern, Ticino, Zurich, the Swiss Lung League, the canton's Lung League of Basel Stadt/ Basel Landschaft, Geneva, Ticino and Zurich, SUVA, Freiwillige Akademische Gesellschaft, UBS Wealth Foundation, Talecris 22 Biotherapeutics GmbH, Abbott Diagnostics, European Commission 018996 (GABRIEL), Wellcome Trust WT 084703MA. Current SAPALDIA Team: Study directorate: T Rochat (p), JM Gaspoz (c), N Künzli (e/exp), LJS Liu (exp), NM Probst Hensch (e/g), C Schindler (s). Scientific team: JC Barthélémy (c), W Berger (g), R Bettschart (p), A Bircher (a), G Bolognini (p), O Brändli (p), C Brombach (n), M Brutsche (p), L Burdet (p), M Frey (p), U Frey (pd), MW Gerbase (p), D Gold (e/c/p), E de Groot (c), W Karrer (p), R Keller (p), B Knöpfli (p), B Martin (pa), D Miedinger (o), U Neu (exp), L Nicod (p), M Pons (p), F Roche (c), T Rothe (p), E Russi (p), P Schmid-Grendelmeyer (a), A Schmidt-Trucksäss (pa), A Turk (p), J Schwartz (e), D. Stolz (p), P Straehl (exp), JM Tschopp (p), A von Eckardstein (cc), E Zemp Stutz (e). Scientific team at coordinating centers: M Adam (e/g), E Boes (g), PO Bridevaux (p), D Carballo (c), E Corradi (e), I Curjuric (e), J Dratva (e), A Di Pasquale (s), L Grize (s), D Keidel (s), S Kriemler (pa), A Kumar (g), M Imboden (g), N Maire (s), A Mehta (e), F Meier (e), H Phuleria (exp), E Schaffner (s), GA Thun (g) A Ineichen (exp), M Ragettli (e), M Ritter (exp), T Schikowski (e), G Stern (pd), M Tarantino (s), M Tsai (e), M Wanner (pa) (a) allergology, (c) cardiology, (cc) clinical chemistry, (e) epidemiology, (exp) exposure, (g) genetic and molecular biology, (m) meteorology, (n) nutrition, (o) occupational health, (p) pneumology, (pa) physical activity, (pd) pediatrics, (s) statistics. Acknowledgements: The study could not have been done without the help of the study participants, technical and administrative support and the medical teams and field workers at the local study sites. Local fieldworkers : Aarau: S Brun, G Giger, M Sperisen, M Stahel, Basel: C Bürli, C Dahler, N Oertli, I Harreh, F Karrer, G Novicic, N Wyttenbacher, Davos: A Saner, P Senn, R Winzeler, Geneva: F Bonfils, B Blicharz, C Landolt, J Rochat, Lugano: S Boccia, E Gehrig, MT Mandia, G Solari, B Viscardi, Montana: AP Bieri, C Darioly, M Maire, Payerne: F Ding, P Danieli A Vonnez, Wald: D Bodmer, E Hochstrasser, R Kunz, C Meier, J Rakic, U Schafroth, A Walder. Administrative staff: C Gabriel, R Gutknecht. Canadian Childhood Cohorts: CAPPS & SAGE CAPPS and SAGE were funded by the Canadian Institutes for Health Research and by AllerGen NCE Inc. (the Allergy, Genes and Environment Network), a member of the Networks of Centres of Excellence Canada program. DD is the recipient of a Michael Smith Foundation for Health Research (MSFHR) Career Scholar Award and holds a Tier II Canadian Research Chair appointment 23 LifeLines The LifeLines Cohort Study, and generation and management of GWAS genotype data for the LifeLines Cohort Study is supported by the Netherlands Organization of Scientific Research NWO (grant 175.010.2007.006), the Economic Structure Enhancing Fund (FES) of the Dutch government, the Ministry of Economic Affairs, the Ministry of Education, Culture and Science, the Ministry for Health, Welfare and Sports, the Northern Netherlands Collaboration of Provinces (SNN), the Province of Groningen, University Medical Center Groningen, the University of Groningen, Dutch Kidney Foundation and Dutch Diabetes Research Foundation. The authors are grateful to the study participants, the staff from the LifeLines Cohort Study and Medical Biobank Northern Netherlands, and the participating general practitioners and pharmacists. 24