Cerebellum
advertisement
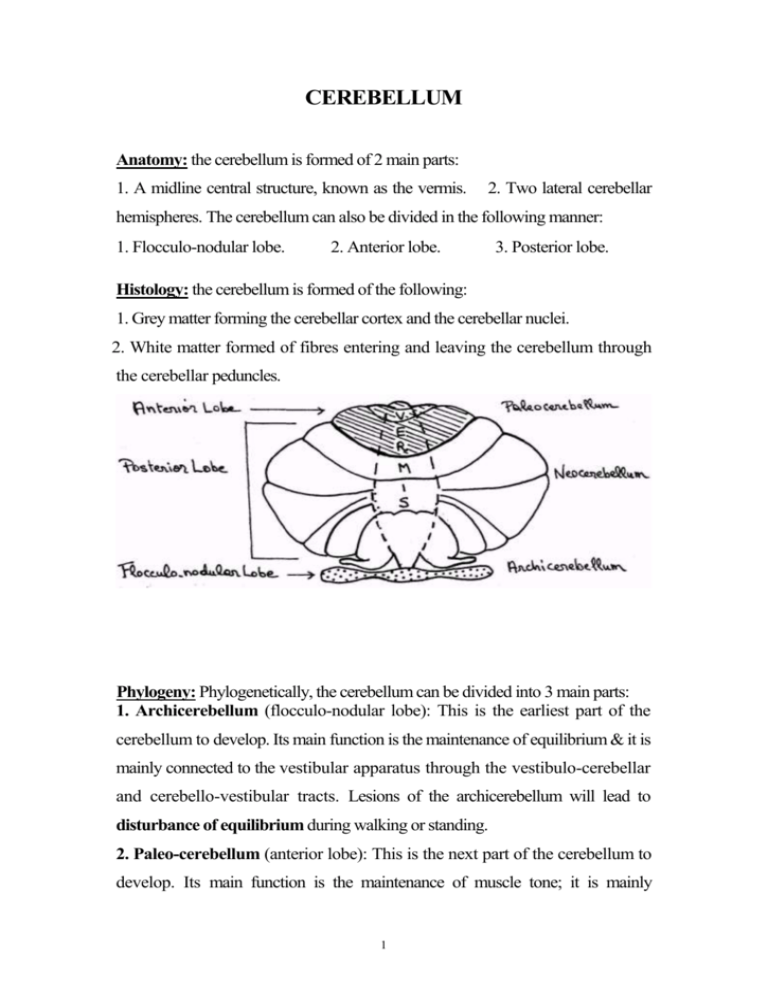
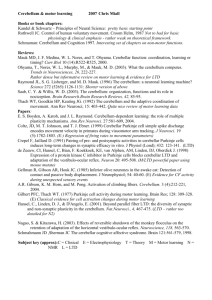
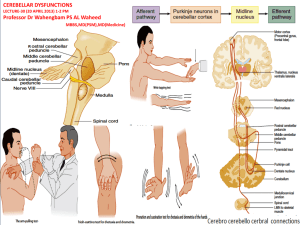
CEREBELLUM Anatomy: the cerebellum is formed of 2 main parts: 1. A midline central structure, known as the vermis. 2. Two lateral cerebellar hemispheres. The cerebellum can also be divided in the following manner: 1. Flocculo-nodular lobe. 2. Anterior lobe. 3. Posterior lobe. Histology: the cerebellum is formed of the following: 1. Grey matter forming the cerebellar cortex and the cerebellar nuclei. 2. White matter formed of fibres entering and leaving the cerebellum through the cerebellar peduncles. Phylogeny: Phylogenetically, the cerebellum can be divided into 3 main parts: 1. Archicerebellum (flocculo-nodular lobe): This is the earliest part of the cerebellum to develop. Its main function is the maintenance of equilibrium & it is mainly connected to the vestibular apparatus through the vestibulo-cerebellar and cerebello-vestibular tracts. Lesions of the archicerebellum will lead to disturbance of equilibrium during walking or standing. 2. Paleo-cerebellum (anterior lobe): This is the next part of the cerebellum to develop. Its main function is the maintenance of muscle tone; it is mainly 1 connected to the spinal cord through the ventral and dorsal spino-cerebellar tracts. Lesion of the paleo-cerebellum will lead to disturbance of the muscle tone (hypotonia). 3. Neocerebellum (posterior lobe): This is the most recent part of the cerebellum to develop. Its main function is the coordination and regulation of the fine delicate voluntary motor activity. It is mainly connected to the cerebral hemispheres through the dentato-rubro-thalamo-cortical tract. Lesion of the neocerebellum will lead to incoordination of movements. ATAXIAS Definition: Incoordination of voluntary motor activity with or without disequilibration in the absence of motor weakness. Types: There may be cerebellar, sensory, vestibular, combined or hysterical ataxia. CEREBELLAR ATAXIA Causes I. Herido-familial: 1. Friedreich's ataxia. 2. Marie's ataxia. II. Symptomatic: 1. Congenital: Arnold Chiari syndrome. 2. Infective: Encephalitis, cerebellar abscess or tuberculoma. 3. Vascular: Superior, middle and inferior cerebellar artery occlusion. 4. Toxic: Alcohol. 5. Neoplastic: Medulloblastoma (tumour of the vermis), astrocytoma (tumour of the hemisphere). 6. Demyelinating: D.S. 2 7. Metabolic: Cortical cerebellar degeneration 2ry to malignancy. III. Idiopathic: Delayed cortical cerebellar degeneration in old age. Clinical picture: 1. Incoordination of movements of different muscles in the form of: a) Nystagmus in the eyes. b) Staccato speech. d) Titubation of the trunk. c) Nodding of the head. e) Kinetic tremors of the limbs. 2. Hypotonia and hyporeflexia of the affected muscles. 3. Gait disturbance: Wide base or drunken gait in archicerebellar lesions. 4. Positive tests of non-equilibrium coordination: Tests of cerebellar ataxia: 1. Finger-to-nose test 2. Finger-to-finger test. 3. Finger-to-doctor's finger test. 4. Adiadokokinesis or Dysdiadokokinesis. 5. Rebound phenomenon. 6. Buttoning and unbuttoning test. 7. Heel-to-knee test. 8. Walking along a straight line. HERIDO-FAM1LIAL ATAXIAS I. Friedreich's Ataxia 1. It occurs in the 1st decade of life. 2. Gradual onset and slowly progressive course. 3. Positive family history is common as it is inherited as an autosomal dominant disease. 4. Pathologically, there is degeneration of: Cerebellum specially the 3 archicerebellum & the spinocerebellar tracts, pyramidal tracts, posterior columns and peripheral nerves. 5. It presents with: - Progressive cerebellar ataxia of the archicerebellar type i.e. disturbance of equilibrium in the form of gait disturbance and trunkal ataxia. - Diminished or lost deep reflexes with positive Babinski sign. The loss of reflexes is due to the degeneration of the peripheral nerves, posterior columns and cerebellum. The positive Babinski sign is due to pyramidal lesion. - Impairment of deep sensations (movement, position and vibration), i.e. sensory ataxia due to degeneration of the posterior columns. - Stock and glove hyposthesia with lost ankle reflex and preserved knee reflex due to degeneration of the peripheral nerves. 6. Skeletal deformities as pes cavus or kyphoscoliosis which are frequent. 7. Congenital heart disease and E.C.G. changes which are common. II. Marie's Ataxia 1. It occurs in the 2nd and 3rd decades of life. 2. Gradual onset and slowly progressive course. 3. Pathologically, there is degeneration of: Cerebellum specially the neocerebellum and Pyramidal tracts. 4. It presents with progressive manifestations of neocerebellar degeneration i.e. tremors of the extremities, staccato speech, nystagmus ... associated with exaggerated deep reflexes and positive Babinski sign due to pyramidal tract degeneration. 5. Mental impairment, ocular nerve paralysis and extrapyramidal syndromes are occasionally present. 4 SENSORY ATAXIA Definition: It is ataxia due to loss of the proprioceptive (deep) sensations, at any point in their pathway. Causes: 1. Peripheral nerve: Peripheral neuropathy specially diabetic, alcoholic and nutritional. 2. Posterior root: Tabes dorsalis. 3. Posterior column: Subacute combined degeneration. 4. Medial lemniscus: Brain stem lesions. 5. Thalamus: Thalamic syndrome. 6. Cortical sensory area: Parietal lobe lesions. Clinical picture: 1. Kinetic tremors as tested by finger-to-nose or finger-tofinger tests appear only on closure of the eyes. 2. Rhomberg's test: When the patient stands with his feet close together & his eyes closed, his body sways & he may fall if not supported. 3. Stamping gait: Heavy strike of the ground on walking due to lost deep sensation. Rhomberg test 4. Deep sensory loss. 5. Hypotonia & hyporeflexia. 5 VESTIBULAR ATAXIA It is ataxia due to lesions of the vestibular division of the eighth cranial nerve. Causes: Labyrinthitis, or acoustic neuroma. Clinical Picture: 1. Vertigo, tinnitus, deafness. 2. Vestibular nystagmus. 3. Impaired tests for vestibular function. Modified from: Elwan H: Principles of Neurology.University book center, Cairo, Egypt, 2007. 6 Rehabilitation of Ataxia The cerebellum and motor control: The anatomical connections of the cerebellum indicate that the cerebellum acts as comparator between sensory input and motor output as it compares the voluntary command for movement with the sensory signals produced by the evolving movement. If motor commands and evolving sensory signals are not appropriately matched, the cerebellum will provide corrective feedback to motor pathways capable of influencing the movement prior to the end of movement. Without such a function, movement will be inaccurate. The cerebellum is assumed to perform predictive compensatory modification in preparation of movement. The cerebellum also acts as adaptive feed-forward control system, which programs or models voluntary movement skills based on a memory of previous sensory input and motor output. Problems of the ataxic patient: 1. Cerebellar ataxic movement patterns result from the impairment of the timing and duration of muscle activation or the magnitude and scaling of force production during voluntary movement. A lack of programmed deceleration is thought to be responsible for the overshoot of dysmetria and oscillation around the end of reaching movement. Patients with cerebellar pathology exhibit hypermetria when they are asked to make rapid tracking movement to a target. Commonly, the abnormal findings that occur with this task are (a) agonist muscle activity is reduced in magnitude and prolonged in time and (b) antagonist muscle activity is delayed resulting in delayed deceleration. 2. Balance abnormalities are characterized by increased postural sway, either excessive or diminished responses to perturbations, poor control of 7 equilibrium during motions of other body parts, and abnormal oscillations of the trunk (titubation). 3. Oro-facial dysfunction due to nystagmus, nodding of head, speech is characterized by dysarthria (staccato speech) and secondary respiratory problems, hypotonia and poor sitting balance. 4. Poor eye-hand coordination is due to nystagmus, nodding of the head, poor sitting balance, proximal instability and intention tremors. 5. Proximal instability around shoulders and pelvis, interfering with control of arm movement and manipulation of objects and interfering with control of the pelvis in weight bearing respectively. 6. Gait problems: They are due to dysmetria and the inability to coordinate the trunk and limbs for safe and smooth walking. Balance is poor, and there is inability to stand on one leg or perform tandem gait. As the condition progresses, walking is characterized by widened base; turning is problematic and can result in falls; and there is high stepping, staggering, and lurching from side to side. 7. Secondary problems as respiratory, circulatory and deformities. Assessment: 1. Assessment of coordination (Equilibrium and Non Equilibrium): a) Equilibrium (balance): Two types of balance were recognized, which are static and dynamic balance. Static balance refers to the ability to control, maintain, and regain the center of gravity (COG) within the base of support (BOS) with the subject still and not subjected to outside perturbations. Dynamic balance is required for daily living activities as walking, running, and stair climbing. Dynamic activities move the COG between boundaries of the BOS and sometimes outside the BOS. 8 There are different methods of balance assessment include noninstrumented and instrumented methods: non-instrumented: - Berg Balance Test. - Functional Reach Test. - Timed Up and Go Test. Instrumented: - Balance Master. - Computerized Dynamic Posturography. - Biodex stability system. b) Non-equilibrium coordination: all non-equilibrium tests should be repeated while the eyes are closed. During these tests, physical therapist should observe proximal stability, reciprocal movement, accuracy of time and place, tremors, dysmetria and decomposition of movement. 2. Asthenia: The cerebellar Pt may experience mild asthenia, i.e., weakness, fatigability. Formal strength testing by dynamometry does show some decrease in the maximum force of contraction. 3. Hypotonia: (passive movement). 4. Gait: (temporal and spatial parameters). 5. Functional capabilities: Such as bed mobility and posture, and ability to dress, groom and eat. Description of performance can include assistance needed, level of effort involved, and time complete the activity. 9 Treatment: The primary goal of the physiotherapy in the rehabilitation of ataxia is to make patient as functional as possible under conditions of maximum safety and reasonable energy cost. The therapist uses the treatment strategies to make the patient perform as independent as possible within the present functional level. The goals of physical therapy can be described as: 1. Improving balance and postural reactions against external stimuli and gravitational changes 2. Improving and increasing postural stabilization following the development of joint stabilization. 3. Developing upper extremity functions 4. Through developing independent and functional gait, improving the life quality of the patient by increasing the patient's independence while performing daily life activities. Main principles of training 1. Throughout the whole training program, exercises should be practiced consciously at first, and in later stages should be followed by automatic exercise activities 2. Exercises should progress from simple to complex. 3. Activities should be practiced first with the eyes open and later with the eyes closed 4. After achieving proximal stabilization, the coordinated movement of the distal segments should be taken into consideration 5. Compensation methods and supportive aids and equipment should be employed when necessary. 6. Treatment should be supported by an appropriate home exercise program and sports activities. 10 Balance training: The patient should be trained in antigravity positions, following the neuro-developmental order, the patient should be trained to come onto the forearms from lying face down, to come onto the knees, half knees and into a sitting position, and to establish static and dynamic balance in these positions. Subsequently, the patient should be trained in positions in which the support surface is narrowed or the center of gravity is changed in order to make the balance activities difficult. (e.g. establishing balance on two or three extremities in the crawling position). In the standing position, following the transferring of weight onto the front, back and sides, narrowing the support surface and balance training in tandem position, balance training on one leg should be performed. This is a position with which ataxic patients have great difficulty. Another option is to perform balance training on the posturography device in order to benefit from visual feedback obtained from observing the patient's ability to sustain his/her postural oscillation in the center of gravity. Movable surfaces are more challenging for the patient. The patient must be safe at all times which may necessitate the need of additional support staff. Use of atilt board or ball or balance master may all be indicated, but safely must always be the first consideration. Proximal stability: The stabilization of the proximal muscles and stabilization of the trunk should be improved. For this purpose, it is appropriate to use the PNF techniques (Rhythmic Stabilization). Coordination training: - Frankle’s exercises:- It is a planned series of exercises, designed to compensate deep sensory loss through utilization of intact senses such as vision and hearing. Simple exercises should be adequately performed at 11 first before progressing to more difficult patterns. Exercises can be done from lying, sitting and standing. While it is described for the lower extremities, similar ones can be developed for the upper extremities. - PNF techniques: slow reversal, slow reversal-hold and reciprocal patterns. Tremors: a. Use of ankle-weighted belt (2-3 LB) and wrist-weighted belt (1-2 LB) weights are considered to be effective in the management of ataxia. They are attached to the affected limb to provide a constant resistance which may dampen the tremor. Weights may be of a value as temporary aid to compensate or dampen tremor, prior to or during performance of a functional task. b. Relaxation by biofeedback training. Relaxation with EMG biofeedback reduces tremor severity and improves functional performance. Gait training: When the patient begins to walk within the parallel bar, he will need precise feedback as to step length, step width, body rotation and trunk position. Also use the following applications: walking on two narrow lines, tandem gait, backward gait, stopping and turning. When the person is ready to walk outside of the parallel bars, a decision will need to be made about an ambulatory aid. Aids, which may be necessary, may also be an obstacle because patients will now need to control position and movement of the device as well as themselves. A walker is typically the most stable. Weighted walker is preferable as it affords more stability. Crutches or canes require reciprocal movement of the arms and legs with appropriate timing and placement; this is too hard or impossible for the patient. 12