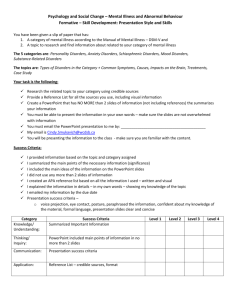
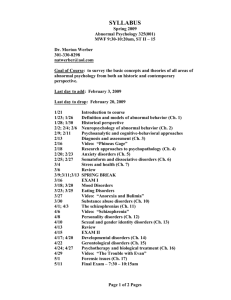
ABNORMAL AND CLINICAL PSYCHOLOGY

qwertyuiopasdfghjklzxcvbnmqwerty uiopasdfghjklzxcvbnmqwertyuiopasd fghjklzxcvbnmqwertyuiopasdfghjklzx cvbnmqwertyuiopasdfghjklzxcvbnmq wertyuiopasdfghjklzxcvbnmqwertyui opasdfghjklzxcvbnmqwertyuiopasdfg hjklzxcvbnmqwertyuiopasdfghjklzxc vbnmqwertyuiopasdfghjklzxcvbnmq wertyuiopasdfghjklzxcvbnmqwertyui opasdfghjklzxcvbnmqwertyuiopasdfg hjklzxcvbnmqwertyuiopasdfghjklzxc vbnmqwertyuiopasdfghjklzxcvbnmq wertyuiopasdfghjklzxcvbnmqwertyui opasdfghjklzxcvbnmqwertyuiopasdfg hjklzxcvbnmrtyuiopasdfghjklzxcvbn mqwertyuiopasdfghjklzxcvbnmqwert yuiopasdfghjklzxcvbnmqwertyuiopas dfghjklzxcvbnmqwertyuiopasdfghjklz
According to psychologists and psychiatrists, normal behaviour is a behaviour which is useful and satisfying the life with no harm to any other individual or no suffering because of any personal distress. Abnormal behaviour signifies any deviance from the normal behaviour.
On psychological front, it is difficult to exactly decide what is normal. Two broad categories have been used to differentiate between normal and abnormal behaviour: descriptive and explanatory criteria.
Descriptive criterion indicates about the types of abnormal behaviour, and explanatory criterion explains their reasons. Descriptive and explanatory criterion further includes sub categories to define concept of normality and abnormality in an individual. Statistical descriptive criterion tells that any person having IQ level average is considered normal, and individual with any deviance is abnormal. This is not a good basis as a genius IQ level will be above average but he/she can’t be described as an abnormal person.
Non statistical descriptive criterion says that if a person acts in a moral or ethical manner or following social and legal norms or showing perfect ideal behaviour is labelled as normal and who behave unethically or not following ideal behaviour and social and legal norms is considered as abnormal. Explanatory criterion includes pathological (medical), psychological, and adjustment criteria which describes that a person’s behaviour is considered abnormal if there is any defect in nervous system’s functioning or defect in functioning of psychological systems or the one who cannot adjust with their surroundings.
No criterion is completely perfect to differentiate between abnormal and normal behaviour
(Mangal, 2008).
Several models of abnormal behaviour have been developed in an attempt to treat patients suffering from abnormal psychological disorders:
The Biological model- It involves treatment using psychotropic medications, neurosurgery, or electroconvulsive therapy (ECT).
The Psychodynamic model- It involves psychoanalysis which brings the traumatic childhood conflicts into conscious awareness and resolving them that have been suppressed.
The Behavioural model- It involves conditioning and behaviour therapy and patient phobias are treated with this learning process.
The Cognitive model- This model involves treatment sessions to bring change in selfdefeating behaviours and beliefs of client by working through rigidity and irrationality. This develops a more rational method for clients to conceptualize themselves, their world, and their life events.
The Humanistic–existential model- It focuses the therapy on supporting the potential achievements and goals of life of client.
The Sociocultural model- Social networks, communication, family structure, and religious and cultural beliefs are focussed.
The Biopsychosocial model (e.g diathesis-stress model)- Biological, psychological, and societal influences on behaviour are studied in this model and patient is treated according to these influences (Corner, 2006).
To assess mental illness is very hard as the carer do not know what the client is suffering from and how it can be dealt. In some cases it took almost years to diagnose what actually the mental illness is. Care faces problem in finding the type of mental illness the client is suffering with as client can present many symptoms which are similar to many types of mental disorders and in some cases patient have various symptoms of several mental disorders. For instance a person in generally is very shy nature and not communicate well, doctor can take it as if some problem but actually the client is not ill, so doctor may advise patient to talk to psychiatrist which is not required.
Likewise, if a patient is ill and shows lucid behaviour while talking to doctor, so doctor will find it difficult to analyse whether this symptom is due to medical illness or some mental illness and he can only find it at later date. Because of these situations, it becomes difficult for the doctors to label an illness and to prescribe the patient a medication. A psychiatrist finds difficulty in assessing all symptoms because of several circumstances and thus finds difficulty in putting patient on best medication, that’s why psychiatrists often change to different medication later on (Denan, 2008).
Psychosis is a term which states that an individual becomes far from the reality and experience different from others. It is not actually a mental illness but is described as more severe form of mental disorder. It is usually presented with a mental state which is due to severe drug adverse effects causing visual and auditory hallucinations. It can be temporary state or permanent state. It is described as serious condition of distress when an individual is
not able to think for his or her own behalf. “Neurosis” term is given to the condition which is being scrutinized by psychological community.it is also not considered as such as mental illness and is explained as unhealthy aspect of one’s own spectrum personality. It is commonly known as personality disorder. According to Freud, neurotic patients can continue to function normally though they can experience enhanced emotional discomfort at sometimes whereas psychotic patients are those individuals who were completely out of reality and are more emotionally disturbed than neurotic ones (Bauers, 2010)
Combination of biological, psychological, and environmental factors may be responsible for mental disorders. Imbalance of neurotransmitters is considered one of the main etiological factors for mental illness; neurotransmitters help nerve cells in the brain to communicate with each other. So an abnormal balance in these factors may cause psychological disorders. Other biological factors that may include: genetics (mental illness is linked to abnormalities in many genes; stress, abuse or a traumatic event can trigger mental illness in a person who has inherited it); infections (certain bacteria such as streptococcus has been linked to obsessive compulsive disorder and other disorders as will especially in children); brain defects or injury; prenatal damage; and sexual abuse. Psychological trauma in childhood (sexual abuse or early loss of parent or neglect) and Environmental factors include poverty; divorce, dysfunctional family life, changing jobs etc. are also play role in worsening mental illness
(Videbeck, 2010).
Psychotherapy: It is an intervention used interpersonally and usually given by a mental health professional like psychologist which utilizes various range of psychological techniques to treat the client. Cognitive behavioural therapy (like dialectical behaviour therapy) is most commonly used for variety of mental disorders. Some therapies include families and other relationships which are based on humanistic approach. Some specific disorders are treated with interpersonal and social rhythm therapy. Psychotherapists sometimes choose techniques employing an integrative or eclectic approach to deal with a particular mental disorder.
(Repper & Perkins, 2006)
Medication: Medication is another intervention used widely to treat mental disorders.
Psychoactive drugs like antidepressants (for depressive and anxiety disorders), anxiolytics
(anxiety disorders and insomnia), mood stabilizers (bipolar disorders especially mania), stimulants, and antipsychotics (for psychotic disorders) are usually prescribed by the psychiatrist (Repper & Perkins 2006).
Electroconvulsive therapy (known as ECT) or Transcranial magnetic stimulation: It is used in a prolonged mood disorder not treated by any other interventions (Lake & Spiegel, 2007).
Other therapy modalities include psychosurgery such as deep brain stimulation; creative therapies like music therapy, drama therapy, or art therapy; somatic manipulation methods including massage and exercises; mind body approaches like yoga, qigong, reiki and prayers; and lifestyle adjustments and supportive measures like self-help, peer support, dietary supplements, and placebo (Lake & Spiegel, 2007).
Individual treatment intervention to treat mental disorder faces its own ethical problems.
Ethical issues of confidentiality and trust effects the therapeutic relationship. Ethical issues related to psychotherapy includes complicated matters related to informed consent, miss or hit techniques of not properly trained therapist, privacy consideration, sexual misconduct by therapists, or special approach for child-adolescent (Nishizono, 1994).
Ethical issues related to treatment occur in choice of treatment as it is difficult to diagnose a mental disorderand its relationship with treatment is often poor, so consequences of inappropriate treatment may be considerable. Evaluation of duration of treatment is also considered as an ethical necessity. Medication given for long period of time predispose client to other medical problems.
REFRENECES
Bauers, D., 2010, The difference between psychosis and neurosis , viewed June 14, 2011, from < http://www.helium.com/items/1358314-how-to-understand-the-difference-betweenpsychosis-and-neurosis?>
Comer, R., 2006, Abnormal Psychology , Worth Publishers, NewYork
Denan, K., 2008, Why is There Difficulty in Diagnosing a Mental Illness ?, viewed June 16,
2011, from <http://ezinearticles.com/?Why-is-There-Difficulty-in-Diagnosing-a-Mental-
Illness?&id=1312286>
Lake, J. & Spiegel, D., 2007, Complementary and alternative treatments in mental health care , American Psychiatric Pub, USA
Mangal, S.K., 2008, Abnormal Psychology , Sterling Publishers Pvt. Ltd, India
Nishizono, M., 1994, Ethical Issues in Psychotherapy, Psychiatry and Clinical
Neurosciences, vol.48, no.1, pp.33-38
Repper, J. & Perkins, R., 2006, Social Inclusion and Recovery: A Model for Mental Health
Practice, BailliereTindall, UK
Videbeck, S.L., 2010, Psychiatric-Mental Health Nursing , Lippincott Williams & Wilkins,
USA