Managing Aggression And Violence
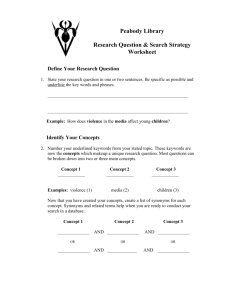
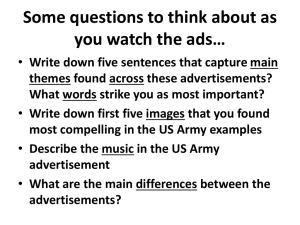
advertisement

Document name: Management of Aggression and Violence: Personal Safety and Violence Reduction policy, procedures and guidance Document type: Clinical Policy Staff group to whom it applies: All staff within the Trust Distribution: Trust wide How to access: Intranet and Internet Issue date: September 2015 Version: Version 4; updated in response to safety alert NHS/PSA/W/2015/011, Jan 2016 Next review: September 2017 Approved by: Executive Management Team Developed by: Managing Aggression and Violence Network Director leads: Director of Nursing Clinical Governance and Safety Contact for advice: Mark Kidder Network Leader Managing Aggression and Violence 01924 327064 Mark.kidder@swyt.nhs.uk 1 Contents 1 Introduction ................................................................................................... .3 2 Purpose ............................................................................................................3 3 Duties ................................................................................................................4 4 Definitions ........................................................................................................6 5 Development of Policy ....................................................................................7 6 Review and revision arrangements including version control .....................7 7 Dissemination and implementation ................................................................8 8 Monitoring Compliance.................................................................................. .9 9 Guidance ........................................................................................................ 10 9.1 Legal issues .................................................................................................... 10 9.2 Ethical issues .................................................................................................. 12 9.3 Mental Capacity Act (MCA) 2005 ..................................................................... 12 9.4 Human Rights Act (1998) ................................................................................ 13 9.5 Public health model ......................................................................................... 13 9.6 Primary prevention .......................................................................................... 14 9.7 Secondary interventions .................................................................................. 16 9.8 Tertiary interventions ....................................................................................... 17 9.9 Restraint .......................................................................................................... 18 9.10 Mechanical restraint ......................................................................................... 22 9.11 Restraint in order to administer treatment ....................................................... 23 9.12 Taking blood without consent .......................................................................... 23 9.13 Rapid tranquillisation ....................................................................................... 23 9.14 Seclusion ......................................................................................................... 23 9.15 Setting incident thresholds for frequent challenging behaviour ....................... 23 9.16 Arrangements for ensuring the safety of lone workers .................................... 23 9.17 Weapons ......................................................................................................... 24 9.18 Situations in which Police involvement may be requested .............................. 24 9.19 Training ........................................................................................................... 25 10 Procedures .................................................................................................... 26 10.1 De-Escalation techniques ................................................................................ 26 10.2 Restraint General principles ............................................................................ 26 10.3 Restraint Procedure………………………………………………… …….....………27 10.4 Post incident support and learning .................................................................. 28 10.5 Evaluation and review ..................................................................................... 29 10.6 Specialist advice .............................................................................................. 29 11 References ..................................................................................................... 29 12 Association documentation ......................................................................... 30 Appendix A What MAV course should I attend ....................................................... 32 Appendix B Equality Impact Assessment Tool ....................................................... 33 Appendix C Version Control Sheet ......................................................................... 35 2 1. INTRODUCTION This policy supports a consistent and positive approach to the management of aggression and violence within South West Yorkshire Partnership NHS Foundation Trust (SWYPFT). While recognising incidents of violence may occur within the course of clinical work, it aims to support staff in effectively managing such incidents safely and effectively. Another key aim of this policy, and its associated procedures and guidance, is reducing the number and severity of incidents of aggression and violence through shaping practice and addressing environmental factors which may contribute to these episodes. It also aims to reduce the frequency of the use of restrictive physical interventions. 2. PURPOSE 2.1 Purpose of the policy Provides guidance on how situations can be minimises the risk to users of the service. Promote safety of staff Identify best practice Set the standards across the organisation Support training packages in place Ensure safeguards in place to aggression Reduce the use of physical intervention in the organisation Safe use of restrictive physical intervention as last resort 2.2 Rationale for development dealt with in a way that manage episodes of violence and The Trust aims to balance the rights and responsibilities of people using its services with those of employees, with a clear approach to therapeutic risk taking. It also aims to support staff, by ensuring that working environments are as safe and pleasant to work in as possible. This document outlines how these aims will be addressed and indicates the Trust’s responsibilities and those of its staff. Risks from aggression and violence are assessed by use of the Trust’s recognised risk assessments (clinical and non clinical) in order to develop safe and supportive systems including the development of personal safety precautions and the development of appropriate skills by its employees. 2.3 Objectives and intended outcome of the policy To provide the Trust and Trust staff with a framework to effectively reduce and manage the risk from aggression and violence. The objectives are to: Support the reduction of violence and aggression by identifying causes and by utilising proactive approaches to reducing incidents; 3 Reduce the use of restrictive physical intervention Clarify responsibilities in relation to Managing Aggression and Violence within the Trust as well as the remit and scope of roles; Outline / describe the Trust’s commitment to training and risk continuum Appendix A); Ensure SWYPFT employees are aware of and can access Managing Aggression and Violence specialist advice. 3. DUTIES The Chief Executive has overall responsibility for the implementation of this policy. The Director of Nursing, Clinical Governance and Safety has lead responsibility for the management of aggression and violence, and is the identified board member for increasing the use of recovery-based approaches including, where appropriate, positive behavioural support planning, and reducing restrictive interventions, reporting regularly to the Trust board on performance. The Network Leader for the Management of Aggression and Violence is responsible for managing and maintaining a network of Personal Safety Specialist Advisors and Trainers. The Network Leader will ensure that network staff supports the Business Delivery Units and support services, in identifying training and development needs with reference to current legislation and best practice. The Network Leader will assist the Trust in reviewing incidents and recommend appropriate action. The Personal Safety Specialist Advisers are responsible for supporting the development and maintenance of a strategic approach to personal safety throughout the Trust. They will support and advise the Business Delivery Units in providing safe and effective care in line with current policy and best practice. The Specialist Advisers also deliver the training for SWYPFT alongside the MAV trainers. The Service Managers will ensure : Staff are aware of and familiar with this and related policies; Incidents of aggression and violence are managed to ensure the immediate safety of those involved; Liaison with clinical teams, managers, Specialist Advisors, and the police as necessary All incidents of aggression and violence are reported factually in clinical records and entered on to the Incident Management Database (DATIX) or via DATIXWEB; Incidents of violence are investigated in line with the Incident Reporting and Management (including Serious Untoward Incidents) Policy and Procedures; Learning from reviews are brought to the attention of the relevant Business Delivery Unit or sub group, the Trust Group responsible for 4 managing aggression and violence and Personal Safety and Aggression Management Specialist Advisers or relevant other Specialist Advisers for further analysis and for sharing more widely across the Trust; Appropriate clinical risk assessments are undertaken and clinical risk assessment tools relating to aggression, violence and personal safety are used; suitable management plans are devised to prevent and manage such incidents. The information will be communicated via multi disciplinary team meetings and Care Programme Approach (CPA) meetings; The generic risk assessment for personal safety contained in the Health and Safety Risk assessment folder is completed. A risk management plan and local procedures should be developed to minimise the risk of violence to staff, service users and the public. These will be evaluated at least annually. Personal safety risk assessment Staff are made aware of the risks within the work place and their personal responsibilities at local and Trust induction. They should also receive information, instruction and education to enable them to work safely; All staff attend their mandatory training and updates appropriate to their area of work commensurate with the level of potential risk, identified with reference Appendix 1; Staff trained in physical skills (breakaway/disengagement or team work) attend refresher updates in accordance with training needs analysis Employees with disabilities, ongoing health conditions, or pregnant employees and nursing mothers who may need to work in identified risk areas have a separate risk assessment as appropriate. It may be appropriate to consult with occupational health staff; All those affected by violent/aggressive situations are to be offered appropriate post incident support, including follow up support, which may include prosecution of an offender through liaison with the Local Security Management Specialists (LSMSs). All Employees should: Employees are responsible for taking reasonable care of their own safety and the safety of others who are affected by their acts or omissions; Comply with this policy; Be familiar with related policies and procedures; Access regular training and updates; Follow any advice, systems, procedures or education introduced in order to reduce or eliminate risks identified. Share information with colleagues to minimise aggression; Support colleagues managing potentially aggressive situations; If required, deploy RPI experience Seek ongoing support, supervision and advice; appropriate to their skills, knowledge and 5 Adhere to the principles of good practice and principles of the use of only justifiable, appropriate reasonable and proportionate force when deploying RPI; Ensure that incidents of aggression and violence are reported factually in the service users clinical record (RIO) and on DATIXWEB are completed in accordance with Incident reporting and management (including Serious Untoward Incidents) Policy and Procedures; Be responsible for their own safety by sharing with managers any issue that need to be taken into account by their involvement in managing aggression and violence, e.g. pregnancy, underlying health conditions, etc. and contact Occupational Health if necessary. 4. DEFINITIONS Workplace Violence Any incident where staff are abused, threatened or assaulted in circumstances related to their work, involving an explicit or implicit challenge to their safety, well being or health. Physical assault The intentional application of force to the person of another, without lawful justification, resulting in physical injury or personal discomfort. (NHS Protect) Non physical assault The use of inappropriate words or behaviour causing distress and /or constituting harassment. (NHS Protect) De-escalation The use of techniques (including verbal and non-verbal communication skills) aimed at defusing anger and averting aggression. Challenging Behaviour Behaviour can be described as challenging when it is of such intensity, frequency or duration as to threaten the quality of life and/or the physical safety of the individual or others and is likely to lead to responses that are reactive, aversive or result in exclusion. (Emerson 2011) Restrictive Intervention Deliberate acts on the part of other person(s) that restrict an individual’s movements, liberty and/or freedom to act independently in order to take control of a dangerous situation where there is a real possibility of harm to the person or others if no action is undertaken, end or reduce significantly the danger to person and others, and contain or limit the patient’s freedom for no longer than is necessary.Restrictive practices refer to physical, mechanical and chemical interventions. (Positive and Proactive Care: reducing the need for restrictive interventions, 2014) 6 Physical Restraint Any direct physical contact where the intention is to prevent, restrict or subdue movement of the body (or part of the body) of another person.” Mental Health Act Code of Practice (2015) Prone Restraint The use of restraint in a face down or chest down position. Incidents of restraint that involve a service user being placed face down or chest down for any period (even if briefly prior to being turned over), should be defined as prone restraint. Similarly if a service user falls or places themselves in a face down or chest down position during a restrictive intervention, this should be defined as prone restraint. 5. DEVELOPMENT OF THE POLICY 5.1 Identification of stakeholders The stakeholders for this policy are: the Executive Management Team (EMT), Trust Board, Managing Aggression and Violence Trust Action Group (MAVTAG), Health and Safety Trust Action Group (H&S TAG) Business Delivery Units, service users, carers, police and SWYPFT staff involved in the consultation, approval and implementation of the policy 5.2 Responsibility for document development This policy has been developed by the MAV Network Leader and the Personal Safety and Aggression Management Specialist Advisers supported by the MAVTAG. 5.3 Equality impact assessment The organisation aims to design and implement services, policies and measures that meet the diverse needs of the service, population and workforce, ensuring that none are placed at a disadvantage over others. The Equality Impact Assessment tool is designed to help consider the needs and assess the impact of policies and is contained in Appendix B. 5.4 Consultation process Consultation via the MAVTAG, (which is made up of BDU representatives, safeguarding leads, equality and diversity leads and service user representatives ) Health & Safety TAG, Business Delivery Units, Managers, Policies and Procedures group before approval via the Executive Management Team (EMT). 5.5 Policy approval process The policy has been considered / reviewed / commended by the Managing Aggression and Violence Trust Action Group and has been agreed as an organisation-wide policy by the EMT. 5.6 Ratification process The EMT is responsible for ratifying the contents of the policy and any expenditure associated with implementing control factors against violence and aggression across the Trust. 7 6 REVIEW AND REVISION ARRANGEMENTS INCLUDING VERSION CONTROL 6.1 Process for reviewing the policy This document will be reviewed bi-annually or more frequently if national policy or guideline changes are required to be considered (whichever occurs first), primarily by the organisation-wide MAV TAG following which it will be subject to re-ratification. 6.2 Version control This document is version 4 (Appendix C) 7 DISSEMINATION AND IMPLEMENTATION 7.1 Dissemination of the policy Once approved, the Integrated Governance Manager will be responsible for ensuring the updated version is added to the document store on the intranet and is included in the staff brief. The Integrated Governance Manager is responsible for ensuring the document being replaced is removed from the document store and that electronic and paper copies, clearly marked with version details, are retained as a corporate record. If local teams down load and keep a paper version of procedural documents, the manager must identify someone within the team who is responsible for updating the paper version when a policy change is communicated All managing aggression and violence training will refer to the current version of this policy 7.2 Implementation of the policy Directors and Business Delivery Units The responsibility to ensure compliance with this Policy rests with the Chief Executive who delegates the operational requirements to each director of a service or Business Delivery Units appropriate to their span of control, who ensure that staff understand and are aware of their responsibilities with regard to this policy. Managers Ensure all staff, including temporary, agency and locum staff, are aware of this policy, complies with it and carry out their responsibilities identified within it, including attendance on training. Ensure the initiation, development and approval of local procedures that support this policy and dissemination of these procedures to their relevant staff. Plan and resource measures to facilitate effectiveness of this policy Employees Employees must ensure they are aware of this policy and work within it, as well as any local procedures within their workplaces. Volunteers, External Contractors and Visitors/Members of the Public 8 Managers have an important role in ensuring that visitors to Trust premises or their areas of responsibility, whilst undertaking work or visiting patients, have minimum potential to be exposed to aggression or violence. It is the responsibility of the person in charge of an area to make external contractors, volunteers , students vistors and members of the public aware of the safety and security of the area and are expected to comply with the instructions given in order to minimise risk of exposure to aggressive or violent situations. Occupational Health As well as providing support through pre-employment health screening, Occupational Health provides assessments of individuals’ ongoing fitness to work, or attend training, liaising with Specialist Advisers or managers where necessary. Staff who have concerns about health issues and their ability to perform physical interventions and/or MAV training should contact Occupational Health for advice. They also provide a post incident or/and a confidential health counselling service, when staff need further advice, support or information. 8 MONITORING COMPLIANCE 8.1 Responsibilities The Executive Management Team (EMT) is responsible for the overall management of incidents within the Trust where Trust-wide incident reports and individual Serious Untoward Incidents are reviewed and through individual Director accountabilities Risk Management Strategy. Business Delivery Units monitor incidents and commission investigations within operational services which includes: Managing issues in relation to incident management, reporting and recording, including inputting on the Datix system.’ Receiving quarterly reports about incident, complaints, claims and legal issues, analysing trends and identifying learning to be shared both across services and with other care groups. Receiving information pertaining to “learning from incidents” within the care group, in other care groups and from specialist advisers and commissioning work to address the identified risk issues. Incidents of clinical aggression and violence are reviewed and monitored through the Management of Violence and Aggression Trust Action Group (MAVTAG) and through the Health and Safety Trust Action Group. The TAGs ensure reporting occurs from all service areas, analyses the incidents looking for trends, develops work streams to act on those trends. They monitor training uptake and evaluation of training. Risk assessments for the prevention and clinical management of violence and aggression and, timescales for review of risk assessments and how action plans are developed as a result of risk assessments are reviewed and formally audited through RiO. 9 Arrangements for the making sure lone workers are safe is by the Head of Health, Safety & Security and the Health & Safety Manager providing reports to the SWYPFT Clinical Governance & Clinical Safety Group and Health and Safety Trust Action Group detailing all incidents/accidents and identifying trends and exceptions. The Clinical Governance and Clinical Safety Committee are responsible for the scrutiny of this process. 8.2 Standards/key performance indicators The Trust reports to NHS Protect Violence Against Staff (VAS) and figures are benchmarked against other organisations. Key performance indicators for physical violence against staff by patient and physical violence against patient by patient, restraint, individuals secluded, and aggression management training are collected monthly or quartly as required on the Compliance Data Capture forms and available on the performance dashboards on the Trust intranet. Key performance indicators for physical violence against staff by patient and physical violence against patient by patient, use of seclusion and use of restraint are collected quarterly for the High Level Summary – Compliance and reported to the Trust board. Audit priorities including managing aggression and violence audits are monitored by the Clinical Audit and Practice Evaluation Group and approved by the Clinical Governance and Safety Committee. Training performance is recorded on the Trust iintranet site. The level of compliance is mandated by the Trust Board and information is collected at Trust, BDU and individual staff levels 9 GUIDANCE Managing aggression and violence The intention of this guidance is to give staff an understanding of the broad spectrum of issues relating to the management of aggression and violence. This guidance supports the training and specialist advice provision available from the South West Yorkshire Partnership NHS Foundation Trust (SWYPFT), Management of Aggression and Violence (MAV) Network. This guidance covers a range of interventions which may be considered for the safe and therapeutic management of people, whose behaviour may present a particular risk to themselves or to others, including staff This guidance applies to all service users, whether or not they are detained under the Mental Health Act (1983 amended 2007). It also accepts that carers, relatives, staff and others may be the source of disturbed or aggressive behaviour . 9.1LEGAL ISSUES Staff need to be aware of the legal and ethical issues which are pertinent in the management of aggression and violence. The management of aggression and violence training courses consider both non physical techniques and physical 10 techniques to manage an aggressive episode and, whether staff are working alone or as part of a team. The physical management of aggression and violence may result in a restriction of the liberty (e.g. in relation to restraint) and autonomy of the person and may be unlawful, Criminal charges such as false imprisonment and assault & battery may arise from the unlawful use of restrictive physical interventions (RPI’s) . The management of aggression and violence must therefore always be justified in law. Lawful Defence and Reasonable Force To enable the application of force and/or the restriction of liberty of a person to be recognised as legitimate there are two criteria which must be satisfied: A legitimate reason to use force or restrict liberty must exist The force and / or restriction used must be Justifiable, Appropriate, Reasonable and Proportionate. Reasonable Force Definition: “The force used should be no more than was necessary to accomplish the object for which it is allowed (so that retaliation, revenge and punishment are not permitted). Secondly, the reaction must be in proportion to the harm which is threatened in both degree and duration” (Dimond B., Legal Aspects of Nursing 2011) The action will be judged with consideration to the facts as the individual perceived them to be at the time, even if he or she later realises it was wrong or unreasonable i.e. If you have an honestly held belief that you or another are in imminent danger, then you may use such force that is necessary to avert that danger. Other Legitimate Defences Exercise of statutory powers and duties. These mainly come from the authority to use force under the Mental Health Act (1983). Self Defence. The law imposes duty on a potential victim to retreat and escape and it is only when there is no opportunity to disengage that self-defence is likely to be considered legitimate. To Prevent a Breach of the Peace. This is defined as a situation where “harm is done or likely to be done to a person or in his presence, to his property: or harm is feared through an affray, riot, assault or other disturbance”. To Prevent a Crime. Section 3 of the Criminal Law Act 1967 states that “A person may use such force as is reasonable in the circumstances in the prevention of a crime or in effecting or assisting in the lawful arrest of offenders or of persons unlawfully at large” This provision applies to both informal and detained patients enables staff to use reasonable force to restrain or breakaway from a person in self defence of others or to protect property. 11 9.2 ETHICAL ISSUES There are ethical issues which are implicit in all decision making, the issues which require particular consideration in this context are: Obligations and duties; Avoiding harm; Assessing the consequences of action; Autonomy and rights; Best interests; Values and beliefs. Duty of Care Staff working in a care environment have a duty of care towards the people they are supporting. Duty of care has been defined as the ‘obligation placed on an individual requiring that they exercise a reasonable standard of care while doing something (or possibly omitting to do something) that could forseeably harm others’. 9.3 MENTAL CAPACITY ACT (MCA) 2005 The MCA came fully into force on 1 October 2007. It is designed to protect people who lack the capacity to take decisions for themselves. There are 5 Key Principles of the MCA (2005) these are: A person is assumed to have capacity; People must be helped to make decisions; Unwise decisions do not necessarily mean lack of capacity; Decisions on behalf of a person who lacks capacity must be taken in the person’s best interests; Decisions must entail the least possible restriction of freedom. The MCA defines restraint and gives criteria that need to be met for restraint to legally occur, they are: The person lacks capacity and it will be in the person’s best interests and; It is reasonable to believe that it is necessary to restrain the person to prevent harm to them and; Any restraint is a proportionate response to the likelihood of the person suffering harm and the seriousness of that harm. Best Interests: The term ‘best interests’ is used in care provision and for the purposes of this document it refers to: 12 ‘Any action taken to preserve the life, or health, or well being. Patients ‘best interest’ include medical as well as wider welfare considerations including: dressing, washing, assisting with the consumption of food and drink’. In the assessing of best interest discussions should include where possible, the service user, family, friends, health professionals carers and advocate. Considerations should include; ethical and religious issues, any previously stated preferences and beliefs and information should be shared to inform the whole team. It should be recorded why any treatment / care is in the service users best interest and the process used to reach the decision.. Staff should consider: Which action would best promote the persons autonomy; Who would benefit from the outcome; What would the least invasive approach or is a reversible approach available; Does everyone agree with the planned outcome The Mental Capacity Act Deprivation of Liberty Safeguards (DoLS) ‘The Mental Capacity Act Deprivation of Liberty safeguards were introduced into the Mental Capacity Act 2005 through the Mental Health Act 2007 The safeguards provide a framework for considering the deprivation of liberty for people who lack the capacity to consent to treatment or care in either a hospital or care home that, in their own best interests, can only be provided in circumstances that amount to a deprivation of liberty’ 9.4 HUMAN RIGHTS ACT (1998) Any use of restrictive interventions must be compliant with the Human Rights Act 1998 (HRA), which gives effect in the UK to certain rights and freedoms guaranteed under the European Convention on Human Rights (ECHR). No restrictive intervention should be used unless it is medically necessary to do so in all the circumstances of the case. Action that is not medically necessary may well breach a patient’s rights under article 3, which prohibits inhuman or degradingtreatment. ‘Inhuman or degrading treatment does not have to be deliberate’ Article 8 of the ECHR protects the right to respect for private and family life. Restrictive intervention that does not meet the minimum level of severity for article 3 may nevertheless breach a patient’s article 8 rights if it has a sufficiently adverse effect on the patient’s private life, including their moral and physical integrity. Restrictions that alone, or in combination, deprive a patient of their liberty without lawful authority will breach article 5 of the ECHR (the right to liberty). 9.5 PUBLIC HEALTH MODEL 13 The model of violence reduction in the Mental Health Act Code of Practice (2015) sees prevention as having three dimensions: primary, secondary and tertiary. The focus is on proactive, preventative measures. Primary Prevention is the action to prevent violence before it occurs and it is a proactive strategy. E.g. risk management, provision of a therapeutic environment Secondary Prevention is the action taken when violence is perceived to be imminent and is a reactive strategy. Tertiary Prevention is the action taken when violence is occurring and provides opportunity for learning for the future. 9.6 PRIMARY PREVENTION Prevention Prevention of aggression and violence is best achieved through effective systems of organisational, environmental and clinical risk assessment and 14 management. Such risk assessment and risk management approaches should also promote therapeutic engagement and collaboration with service users. Fostering and Developing Positive Relationships The principles of establishing positive relationships and clear communication with other organisations, service users, and carers must be a priority. Developing positive relationships can reduce the potential for aggression and violence and consequently the need to deploy RPI’s. Staff must try to develop sound trusting therapeutic relationships with service users so that they can learn to recognise potential danger signs. Staff should understand when to intervene to prevent harm from occurring. Continuity of staffing is an important factor both in the development of professional skills and consistency in managing service users. Services and staff should demonstrate and encourage respect for racial and cultural diversity, and recognise the need for privacy and dignity. These are essential values that are asserted in policy, educational material, training and practice initiatives related to the safe and therapeutic management of service users. Staff should also recognise that, due to the nature of their contact with service users, they may experience disturbed behaviour as intermittent, while fellow service users or carers experience it as persistent. Particular care needs to be taken to ensure that negative and stigmatising judgements about certain behaviours, diagnoses or personal characteristics do not obscure a rigorous assessment of the degree of risk or the potential benefits of appropriate treatment to people in severe distress. Providing Information Service users should have access to information about the following in a suitable format: Which staff are on duty, including any assigned to support them personally Why they have been admitted (and if detained, the reason for detention, the powers used and their extent, and rights of appeal); What their rights are with regard to consent to treatments, complaints procedures, and access to independent help and advocacy and What may happen if they pose a danger to themselves or others . This information needs to be provided at admission, repeated as necessary and recorded in the clinical record.. Other Strategies In addition to individual care plans incorporating positive behaviour support which are fundamental to the appropriate management of challenging behaviour, problems may be minimised by considering the environments and identifying and managing problem areas. Among such general measures are: Engaging service users and keeping them fully informed of what is happening and why; 15 Giving each service user a defined personal space for the safe keeping of possessions; Organising the unit on in patient areas, to provide, for example, quiet rooms, recreation rooms, single sex areas, visitors' rooms and access to fresh air; Ensuring service users are able to make telephone calls in private, wherever possible; Involving service users in identifying their own trigger factors, early warning signs of disturbed or violent behaviour and the management of these; Providing appropriate activities for all service users, including exercise areas and encouraging service users to take part in appropriate activities Managing the skill mix of staff and responding to changes in clinical environment Consistent application and monitoring of any individual programme (care plan) ; Ensuring that service users' concerns are dealt with quickly and fairly. Safe Place of Work To establish a safe place of work and to encourage a pro-security safety culture; risk assessment and risk management plans need to be formulated and implemented . In exploring preventive methods staff should be aware of some possible factors which may contribute to challenging behaviour. Such as: Boredom and lack of environmental stimulation; Too much stimulation, overheating, noise and general disruption; Overcrowding, lack of access to external space; Personal frustrations associated with being contained within a restricted environment; antagonism, aggression or provocation on the part of others; Influence of alcohol or substance abuse; An unsuitable mix of service users 9.7 SECONDARY INTERVENTIONS Risk assessment Thorough evidence-based clinical risk assessment and management is an essential and on-going element of good care planning, and effective and safe practice. The key principle is that all service users will have a risk assessment completed and documented, where necessary leading to the development of a documented risk management plan Clinical risk assessment, management and training policy Cues to aggression Warning signs or cues often precede acts of aggression . The more observant you are the more likely you are to pick up on these cues. The earlier the subtle signs are identified the more options may be available to de-escalate the situation. 16 Cues to aggression vary from person to person, one of the most indicative is a change in behaviour that varies from the individuals ‘norm’. The following list, which is not exhaustive, may help to indicate that a service user is at increased risk of becoming aggressive . Cues identified that are known to an individuals aggression precede a known persons violence should be included in their care plans and risk management plans; Tense / angry facial expressions; Increased prolonged restlessness, pacing, body tension; Increased breathing, muscle twitching and dilated pupils; Increased volume of speech; Refusal to communicate, withdrawal, irritability; Prolonged eye contact; Thought processes unclear, poor concentration; Delusions or hallucinations with violent content; Threats or gesture; Reporting anger or violent feelings. Use of Electronic Alarms and Call Systems These systems are usually ward / unit based and designed to call for assistance and or to activate in the case of an emergency. Managers should ensure that there are enough units for all staff who require one and everyone is instructed in there use and what to expect as a response. A local protocol giving staff guidance on what to do in the event of an alarm being activated such as identifying specific individuals to attend incidents or the formation of a response team should be in place and all staff aware of. More guidance is a available from Operational Guidance for the Pinpoint Alarm System http://nww.swyt.nhs.uk/docs/Documents/1016.doc 9.8 TERTIARY INTERVENTIONS Tertiary interventions may be required when violence is occurring; the main purpose of this section and the techniques are to effectively manage the incident and to enable learning from incidents to take place. Individuals in need of care and treatment may, as a consequence of their presentation , present particular risks to themselves or others. Such risks are usually associated with behaviours that challenge Staff should also be aware of other risks , such as self-neglect or sexual vulnerability. The primary focus for managing people who may present with disturbed or violent behaviour (or both) should be the establishment of a culture which focuses on early recognition, prevention and de-escalation of potential 17 aggression, using a wide range of techniques to minimise the risk of its occurrence; Ensure that the techniques and methods used to restrict a service user: are proportionate to the risk and potential seriousness of harm are the least restrictive option to meet the need are used for no longer than necessary take account of the service user’s preferences, if known and it is possible to do so take account of the service user’s physical health, degree of frailty and developmental age.. 9.9 RESTRAINT Interventions such as restraint, seclusion, or rapid tranquilisation should only be considered if de-escalation and other strategies have failed to manage the individual . Where such interventions are necessary, clinical need and the safety of the service users and others is the primary consideration. Any interventions employed to manage disturbed behaviour must be seen as Justifiable, Appropriate, Reasonable and Proportionate, taking into account the risks posed by the behaviour or potential behaviour. The choice of appropriate restrictive intervention will depend on various factors, but should be guided by: The duty to protect other service users, visitors and staff; and Service user preference, if known; The clinical needs of the service user; The needs of other people affected by the disturbed behaviour; The availability of resources within the environment of care; The justification for physical responses. Physical responses, , are no substitute for identifying and addressing the problem before it reaches a crisis. The Managing Aggression and Violence Network is available to support staff and the specialist advisors can provide support with any aspect of the MAV. Safety of Others (When Staff Member is on Their Own) A dilemma occurs for staff when faced with a situation, where an aggressor may be inflicting injury on themselves or another. It is important that the staff member does not lose regard for their own safety. The desire to protect a vulnerable individual is understood, staff must: Always judge their ability to manage the intervention in a way that produces best outcome; Summon assistance if they cannot manage the intervention; 18 Unless exceptional circumstances exist, not attempt to restrain the individual on their own. Restraint (Mental Health Act 1983 - Code of Practice revised 2015) Restraint may take many forms. It may be both verbal and physical and may vary in degrees from an instruction to seclusion. The purpose of restraint as a response to immediate risk is: take immediate control of a dangerous situation where there is a real possibility of harm to the person or others if no action is undertaken, and end or reduce significantly the danger to the patient or others. The most common reasons for restraint are: The most common reasons for needing to consider the use of restrictive interventions are: physical assault by the patient dangerous, threatening or destructive behaviour self-harm or risk of physical injury by accident extreme and prolonged over-activity that is likely to lead to physical exhaustion, or attempts to escape or abscond (where the patient is detained under the Act or deprived of their liberty under the MCA). Any restraint used should: be used for no longer than necessary to prevent harm to the person or to others be a proportionate response to that harm, and be the least restrictive option use least restrictive level of hold Using Physical Interventions (Restraint) as Part of a Team Approach Physical intervention describes a conscious or reactive decision by a person or persons to assist, support, hold or restrain another person. This will be either a: Pre-arranged intervention (Planned). This should be documented in the service user’s positive behaviour support plan or individual care-plan. The procedure should be reviewed regularly by the multi-disciplinary team and where possible, include the views of the service user or, A reactive response (Unplanned). This will always depend on all the circumstance of the situation. Following a reactive response a review should take place to determine what if anything can be done to prevent the intervention becoming necessary in the future. If a positive behaviour support plan is not already in place then one should be started. 19 Restrictive Interventions No restrictive intervention should be carried out unless it is medically necessary to do so. Action that is not medically necessary may breach the patient’s human rights under article 3, which prohibits inhuman or degrading treatment. It may also breach their article 8 rights to a private and family life or article 5 rights to liberty. Any individual who may exhibit behaviours which may present a risk to themselves or other people should have a full risk assessment of their potential and their needs. This should be incorporated into a positive behaviour support plan / care plan. All individuals should be evaluated to identify any physical or psychological risks and any religious, cultural or gender issues that may require restraint techniques to be modified. These may include: Musculoskeletal problems that limit joint movement, decrease bone strength, cause deformity or cause pain. This includes limb loss and the presence of prosthetics (false limbs) or orthotics (splints). Neuromuscular problems that may include high muscle tone, low muscle tone, ataxia or athetosis. Cardiovascular problems such as angina, heart conditions, hypertension or hypotension and history of heart attack. This should include presence of blood disorders that affect clotting. Respiratory disease such as asthma, chronic obstructive pulmonary disease or any condition affecting the patient’s breathing. Pregnancy or post-partum. Altered sensory systems that affect pain or touch sensation, positioning the body in space, hearing or speech. Previous psychological trauma that may have resulted from abuse or assault. Use of drugs and/or alcohol If physical or psychological risk factors are identified consideration should be given to contacting the MAV team for specialist advice. Any individual who presents with behaviours that are challenging must have a behaviour support plan that covers: what is usual for them , what triggers unwanted behaviours, what the behaviours are, 20 the desired outcomes for the individual and how they should be managed at primary, secondary and tertiary levels. This should be produced in collaboration with the individual , their family, carers and advocate. All restrictive interventions must be applied using principles and methods taught on the trust training syllabus, by staff that are competent to do so. Due regard must be taken of the risks to life and health identified as part of the training. Restrictive interventions should be used in a way that minimises any risk to the patient’s health and safety and that causes the minimum interference to their autonomy, privacy and dignity, while being sufficient to protect the patient and other people. The patient’s freedom should be contained or limited for no longer than is necessary. Unless there are cogent reasons for doing so, staff must not cause deliberate pain to a patient in an attempt to force compliance with their instructions(for example, to mitigate an immediate risk to life). In areas where restrictive interventions occur there must be access to life support equipment as described in the trust resuscitation policy. In exceptional circumstances when staff are unable to safely manage a violent situation using the techniques and facilities that are available to them, the assistance of the police may be requested. In these cases staff remain responsible for the health and safety of the individual . The emotional and psychological wellbeing of patients must be properly managed. This should be done by involving the patient in the planning of restrictive interventions whenever possible, reassuring them and explaining what is happening during the restrictive intervention and post-incident counselling as soon after the incident as is appropriate. Individuals should be medically assessed following physical restraint. If staff are concerned and no doctor is immediately available arrangements should be made to transfer the patient to A&E. All instances of restrictive interventions must be fully recorded in the patient’s clinical record and on the trust incident system. Records must include an account of: The lead up to the intervention How staff attempted to de-escalate the incident A detailed description of the restrictive intervention, including all positions and holds used, which staff were involved and what they 21 were doing, the length of the restrictive intervention and the conditions under which it was discontinued. The post-incident counselling offered to the patient Any changes made to the positive behaviour support plan. Staff involved in the incident should be involved in a post-incident review which analyses the effectiveness of the de-escalation and the intervention. All staff working in clinical areas must undertake training around the management of aggression and violence that has been identified as appropriate to their role and work area. (see Trust mandatory training) 9.10 MECHANICAL RESTRAINT Mechanical restraint is a form of restrictive intervention that refers to the use of a device to prevent, restrict or subdue movement of a person’s body, or part of the body, for the primary purpose of behavioural control Mechanical restraints are not routinely used within the Trust for any of our service users except in extraordinary and/or urgent situations, and then only for the shortest possible time and when all other less restrictive options have been considered/exhausted by the team and senior managers. The use of any mechanical restraint must be based on a comprehensive risk assessment by the RC and MDT and a care plan and safeguards need to be in place to protect the service user and others, which are regularly reviewed. Those using mechanical restraints must be trained and experienced in their use. The use of mechanical restraints is usually limited to patients identified as requiring this level of intervention when off the ward. These will be patients most likely subject to Ministry of Justice overview. The use of mechanical restraints will be included in the risk management and associated care plans for the patient. The use of mechanical restraints in other situations is subject to an MDT meeting, consisting of the patient’s Responsible Clinician, the nurse in charge of the ward, the patient’s named nurse, any other clinician significantly involved in the patient’s care, an IMHA, an IMCA if applicable and if possible. The decision must be communicated to the relevant General Manager and the BDU director or the Director of Nursing in their absence. This plan should detail the circumstances which might warrant mechanical restraint, the type of device to be applied, how continued attempts should be made to de-escalate the situation and any special 22 measures that are required to reduce the likelihood of physical or emotional trauma resulting. Where the care plan allows the nurse in charge to authorise the use of mechanical restraint, the patient’s Responsible Clinician or on call consultant should be informed immediately. When mechanical restraint is used to manage violent behaviour rather than as a security measure, the patient must remain under continuous observation throughout, be reviewed by a registered nurse every 15 minutes and be examined by a doctor after one hour and at four hourly intervals. Reviews should ensure that the individual is as comfortable as possible and should include a full evaluation of the patient’s physical and mental health condition. Reviews should be undertaken more frequently if requested by nursing staff. At all times the MHA Code of Practice and the MAV Specialist Advisor should be referred to when considering and using mechanical restraint. The application and use of materials or equipment (which may include prescribed therapeutic aids) such as belts, helmets, clothing, straps, cuffs, splints and specialised equipment, which are designed to specifically restrict the free movement of an individual but must be considered as a restrictive practice as described in the MCA (2005) and the necessary safeguards for use of mechanical restraints must be applied. 9.11 RESTRAINT IN ORDER TO ADMINISTER TREATMENT Restraint can also be used in order to administer medication (or other forms of treatment) , where there is legal authority1 to treat the individual without consent. It should not be used unless there is such legal authority. The use of restraint to administer treatment in non-emergency circumstances should be properly documented in the service user’s notes, along with the justification for it. It should, where possible follow the restraint procedure and be care planned. Medication should never be used to as a substitute for adequate staffing. Other than in exceptional circumstances, the management of behaviour by medication should only be used after careful consideration, and as part of a treatment plan. 9.12 TAKING BLOOD WITHOUT CONSENT The CQC issued guidance on the taking of blood under the Mental Health Act as a treatment “ancillary” to treatment with medications such as clozapine and 1 Legal Authority refers to either consent as in the case of a person with capacity or that they are detained Mental Health Act (1983). Those who lack capacity and are not detained MHA would require the decision of a MDT, may be an IMCA involved and possibly Court of Protection involvement depending on the gravity of the decision 23 lithium and agreed that it could be enforced for detained service users who do not consent to blood testing. The degree of resistance and its origins (e.g. religious objections) to the blood sampling should be taken into consideration. Any other blood testing without consent should only occur after consideration of the criteria that need to be met for restraint to legally occur under the Mental Capacity Act The person lacks capacity and it will be in the person’s best interests and; It is reasonable to believe that it is necessary to restrain the person to prevent harm to them and: Any restraint is a proportionate response to the likelihood of the person suffering harm and the seriousness of that harm Advice should be sought from the MAV team where it is anticipated that resistance and restraint might occur. 9.13 RAPID TRANQUILLISATION The Rapid Tranquilisation Policy should be consulted. 9.14 SECLUSION The Seclusion Policy should be consulted 9.15 SETTING INCIDENT THRESHOLDS FOR FREQUENT CHALLENGING BEHAVIOUR In some clinical situations staff may find it difficult to know when to record certain events or behaviours as an incident. For example, if an individual service user has a frequent pattern of behaviour such as self harming, verbal aggression or challenging behaviour, which could be seen as the usual presentation of their condition. It is impossible to give a definitive guide for recording these incidents, but a process is suggested in the Incident reporting and management (including Serious Untoward Incidents) Policy and Procedures; 9.16 ARRANGEMENTS WORKERS FOR ENSURING THE SAFETY OF LONE The trust must ensure that they have adequate arrangements in place to asses risk to their staff. A risk assessment is carried out to identify the risks to workers and any others who may be affected by their work. Proper conduct of the assessment must identify how the risks arise and how they impact on those affected. This information is needed to make decisions on how to manage those risks so that the decisions are made in an informed, rational and structured manner and that the action taken is proportionate. Arrangements also need to be put in place to monitor and review the findings. Lone Working Policy 9.17 WEAPONS 24 Throughout this document, the term ‘weapon’ means any object that could be used to threaten or injure another person. 2 This guidance does not cover guns, other firearms or similar weapons (including replicas). All incidents involving firearms should be immediately reported to the police in line with locally agreed protocols It is essential that managers develop strategies for managing difficult situations. The Trust has a policy on searching patients and their property to promote a safe and secure environment. This should be applied with caution if there is a reasonable suspicion that the service user is carrying a weapon and there is an risk to the service user, staff or others. If a weapon is used or threatened Staff should attempt to isolate the individual . Occasionally people may use a weapon during an act of violence. Staff should not attempt to disarm the person. Service users or visitors will be isolated where possible and a 999 call made to the Police and a call for assistance made. Consider the use of barriers, space and knowledge of the environment such as keeping access to exits to maintain personal safety. If safe attempt to maintain dialogue with the potential assailant, with the aim of getting the assailant to stop threatening with the weapon, whilst maintaining a safe distance. Where life is threatened, do as the person demands, try persuasion and try to get help. If this is not possible then staff should use any justifiable, appropriate reasonable and proportionate measures to defend themselves and others in order to escape and call for assistance. 9.18 SITUATIONS IN WHICH POLICE INVOLVEMENT MAY BE REQUESTED Police involvement may be requested in relation to: Preventing a breach of the peace on Trust premises; Assisting in an incident when staff and or patients are threatened and staff are unable to safely manage or contain the situation; In response to risks to individuals or the public identified in the course of assessment and treatment; Evidence or suspicion of environment. illegal drugs or weapons into the ward It is acknowledged that once the police have been summoned to an incident, they will assume operational control and staff should do as directed by officers. Staff remain responsible for the patient’s health & safety. 2 NHS Counter Fraud and Security Management Service. (2006).Offensive weapons NHS Security Management Service guidance. NHS CFSMS 25 If the police have been called to an incident, the nurse in charge of the ward should provide an orientation of the ward, brief description of circumstances leading up to the incident, the type of weapon, where patient is located and how the patient is currently presenting. Any known medical conditions, drugs and alcohol. (See Violence, Abuse, Harassment and Aggression at Work Policy Violence, Abuse, Harassment and Aggression at Work Policy) 9.19 TRAINING The Trust provides training for staff to ensure they can fulfil their responsibilities under the policy and take measures to protect themselves, service users and members of the public from aggression or violence at work. All staff must attend managing aggression and violence training where it has been identified as being mandatory. Staff can obtain details of the types of training available, training dates / venues and course information via the SWYPFT Learning & Development Portfolio or the Managing aggression and violence network. Tel: 01924 327064 Training needs are prioritised according to risk (Appendix A). The level of training required by staff is determined by their post and area of work. This information is reflected on ESR as a competence requirement of each post and ESR reporting arrangements will reflect this. Staff will be introduced to this policy at initial work-based Induction training and are made aware of their departmental procedures on the control of aggression /personal safety and violence. The Trust provides bespoke training for staff who works in areas where they may be exposed to aggression or violence, or may need to become involved in the restraint of service users. This includes recognising anger, potential aggression, antecedents and risk factors of disturbed or violent behaviour and how to monitor their own verbal and non-verbal behaviour. Training includes methods of anticipating, de-escalating or coping with disturbed/violent behaviour. Where staff have been unable to access training prior to commencing work , managers, as an interim measure, must ensure that systems are in place to ensure that recognition, prevention and de-escalation of aggression and violence awareness forms part of the ward/unit induction programme and is underpinned by a robust risk assessment. This should make clear what the staff member’s response and role should be when faced with incidents involving aggression and violence. These principles should also be applied to bank, agency and all staff unfamiliar to the ward/unit. All staff who undertake training in the management of aggression and violence and physical interventions training should attend .refreshers at intervals commensurate with their post and area of work. 10 PROCEDURES 26 10.1 De-Escalation techniques The response to aggression would depend on whether the aggression was directed toward the staff member on a one to one basis (i.e. lone working or isolated) or whether the aggression was in an environment where assistance could be summoned if required. One staff member should lead the response – unless they are alone with potential aggressor where they may have to consider exiting. That staff member should consider which de-escalation techniques are appropriate. Appropriate de-escalation techniques should have been identified through risk assessment and care planning. The staff member should give clear explanations and instructions to the service user regarding what they intend to do, and relevant options. Separate agitated service users from others (using quiet areas of the ward, bedrooms, comfort rooms, gardens or other available spaces) to aid deescalation, ensuring that staff do not become isolated. Use a designated area or room to reduce emotional arousal or agitation and support the service user to become calm. In services where seclusion is practised, do not routinely use the seclusion room for this purpose because the service user may perceive this as threatening. The staff member who coordinates the response should attempt to clarify the issue and attempt collaborative problem solving. This will involve: Establishing rapport and emphasising the need for mutual co-operation. Negotiating realistic options. Asking open questions. Ensuring that non-verbal and verbal responses indicate concern and attentiveness. Using empathic and non-judgemental listening. Paying attention to the non-verbal communication of the service user. Paying attention to staffs own non-verbal communication, respecting personal space and avoiding confrontational eye contact. Adopting a non-threatening but safe stance, safe distance, side on. Appearing to be calm and in control. (It is difficult to be calm due to the effect of adrenaline although an appearance of calm gives some reassurance to the agitated person). 10.2 Restraint General principles Is an emergency response or there seems to be a real possibility that significant harm would occur if no intervention is made; One staff member should coordinate response to the incident; 27 Move others not involved; Approach and ask individual to stop the behaviour or comply with a request; Give explanations of possible outcomes; Any initial attempt to restrain aggressive behaviour should, as far as the situation will allow, be non-physical; A balanced judgement should be made between the need to promote autonomy and the duty to protect individuals from likely harm; The specific needs of service users with sensory impairments should be taken into account - approaches to deaf and hearing impaired service users should be made within their visual field (not from behind) and gestures used to engage them in calm communication; 10.3 Restraint Procedure Assistance should be sought by call system or verbally; Where possible only staff trained on the MAV Teamwork course should be involved in restraint; Staff not trained on the MAV Teamwork course should not be placed on response teams or participate in prearranged physical interventions, unless in an emergency ; Large numbers of staff acting in a uncoordinated way can be counter productive. Organise a well briefed team of staff (The team approach demonstrated in MAV training); Make a visual check for weapons; Once committed, act decisively; Patients should not be deliberately restrained in a way that impacts on their airway breathing or circulation. The mouth and/or nose should never be covered and there should be no pressure to the neck region, rib cage and/or abdomen. Unless there are cogent reasons for doing so, there must be no planned or intentional restraint of a person in a prone position on any surface, not just the floor. Therefore, wherever possible, restraining service users on the floor should be avoided. If, however, the floor is used, then this should be for the shortest period of time and for the central reason of gaining control of a highly risky or dangerous situation. In exceptional situations where the service user needs to be placed in the prone position, this should be for the shortest possible period of time. Do not routinely use manual restraint for more than 10 minutes. Consider rapid tranquillisation or seclusion as alternatives to prolonged manual restraint (longer than 10 minutes). 28 During restraint against active resistance or if a restraint ends up on the floor, one team member should be responsible for protecting and supporting the head and neck; All team members should take responsibility for ensuring the health and wellbeing of the service user during restraint; Don’t be distracted from your allocated task as part of the team; Ensure that airway and breathing are not compromised; Monitor vital signs, for signs of distress and the physical and psychological health of person. Monitor vital signs using the Early Warning Score or EWS (appendix 1 Cardiopulmonary Resuscitation Policy) and associated documentation and follow the guidance. If vital cannot be monitored, e.g. service user refusal, the reasons why they could not be monitored should be recorded in the clinical record End restraint as soon as it is safe to do so. 10.4 Post incident support and learning After using a restrictive intervention, and when the risks of harm have been contained, conduct an immediate post-incident review, including a nurse and a doctor, to identify and address physical harm to service users or staff, ongoing risks and the emotional impact on service users and staff, including witnesses. Discuss the incident with service users, witnesses and staff involved only after they have recovered their composure and aim to: acknowledge the emotional responses to the incident and assess whether there is a need for emotional support for any trauma experienced promote relaxation and feelings of safety support a return to normal patterns of activity ensure that everyone involved in the service user's care, including their carers, has been informed of the event, if the service user agrees. Ensure that the necessary documentation has been completed. Ensure that the service user involved has the opportunity to discuss the incident in a supportive environment with a member of staff or or carer. Offer the service user the opportunity to write their perspective of the event in the notes. A Post Incident Review should: evaluate the physical and emotional impact on everyone involved, including witnesses help service users and staff to identify what led to the incident and what could have been done differently determine whether alternatives, including less restrictive interventions, were discussed 29 determine whether service barriers or constraints make it difficult to avoid the same course of actions in future recommend changes to the service’s philosophy, policies, care environment, treatment approaches, staff education and training, if appropriate avoid a similar incident happening in future, if possible. Further learning for staff can be gained through individual clinical supervision or group supervision sessions. The MAV Network is available for advice on any technical details of the management of violence and aggression or if the review highlights any issues regarding the use of RPI. Any staff member involved in an aggressive or violent incident can access appropriate support and further counselling if necessary through the Staff Counselling Services, Occupational Health Service or Pastoral Care 10.5 Evaluation and review A key part of the evaluation and analysis process is the role of information obtained from the DATIX system. The Trust will use the DATIX system to monitor and analyse aggressive and or violent incidents including “near misses”. This will highlight concerns and emerging trends, which will enable Business Delivery Units and managers to evaluate procedures and practices to be changed, where necessary, to improve the environment for staff and service users. The MAVTAG and the Health and Safety Trust Action Group also monitor incidents of violence and aggression Procedures developed by managers will be reviewed regularly to ensure they remain relevant to the prevailing circumstances. They will also be reviewed in the light of information received about incidents, new published guidelines and the principles of good practice. 10.6 Specialist advice The MAV Team is available to offer training, advice and support to all services and staff across all BDU’s based on national best practice guidance. Contact the team 11 REFERENCES A Positive and Proactive Workforce: a guide to workforce development for commissioners and employers seeking to minimise the use of restrictive practices in social care and health. Skills for Health and Skills for Care.(2014) http://www.skillsforhealth.org.uk/component/docman/doc_download/2423-apositive-andproactive-workforce.html British Institute of Learning Disabilities (2014) Code of Practice forminimising the use and reduction of physical interventions:planning, developing and delivering training (4th Edition) http://www.bild.org.uk/our-services/books/positive-behaviour-support/bildcode-of-practice/ 30 British Institute of Learning Disabilities (2013) Framework for Reducing Restrictive Practices http://www.bild.org.uk/our-services/books/positive-behavioursupport/framework-for-reducing-restrictive/ British Institute of Learning Disabilities (2014) A human risghts perspective on reducing restrictive practices in intellectual disability and autism. http://www.bild.org.uk/our-services/books/positive-behaviour-support/ahuman-rights-perspective/ Department of Health. (2015). Mental Health Act 1983 Code of Practice. London. TSO https://www.gov.uk/government/uploads/system/uploads/attachment_data/f ile/396918/Code_of_Practice.pdf Meeting Needs and Reducing Distress: guidance on the prevention and management of clinically related challenging behaviour in NHS settings. Department of Health, NHS Protect. (2013). http://www.nhsbsa.nhs.uk/Documents/SecurityManagement/Meeting_need s_and_reducing_distress.pdf NHS SMS (2003) A professional Approach to Managing Security in the NHS. London, NHS SMS. http://www.nhsbsa.nhs.uk/SecurityManagement/Documents/sms_strategy. pdf NHS Security Management Service (2005) ‘Not Alone’ A Guide for the Better Protection of Lone Workers in the NHS. London NHS SMS http://www.nhsbsa.nhs.uk/SecurityManagement/Documents/Lone_Working _Guidance_final.pdf NHS Counter Fraud and Security Management Service. (2006).Offensive weapons: NHS Security Management Service guidance. NHS CFSMS http://www.nhsbsa.nhs.uk/SecurityManagement/Documents/offensive_wea pons.pdf NHS Security Management Service (2005) Promoting Safer and Therapeutic Services - Implementing the National Syllabus in Mental Health and Learning Disability Services, NHS Security Management Service. http://www.nhsbsa.nhs.uk/SecurityManagement/Documents/psts_impleme nting_syllabus.pdf NHS Security Management Service (2007) Tackling Violence Against Staff. Explanatory notes for reporting procedures by Secretary of state Directions in November 2003 (updated March 2007) London, NHS SMS. http://www.nhsbsa.nhs.uk/SecurityManagement/Documents/Tackling_viole nce_against_staff_2007.pdf Positive and Proactive Care: reducing the need for restrictive interventions.Department of Health. (2014). https://www.gov.uk/government/publications/positive-and-proactive-carereducing-restrictive-interventions 31 Royal College of Nursing (2007) Lets talk about restraint rights risks and responsibility http://www.rcn.org.uk/__data/assets/pdf_file/0007/157723/003208.pdf Violence and Aggression: Short-term management in mental health, health and community settings. Updated edition. NICE Guideline NG10 (2015) http://www.nice.org.uk/guidance/cg25/resources/cg25-violence-fullguideline 12 ASSOCIATED DOCUMENTATION Clinical risk assessment, management and training policy Care Programme Approach http://nww.swyt.nhs.uk/cpa/Pages/default.aspx Health, Safety, Security and Environment home page http://nww.swyt.nhs.uk/health-safety/Pages/default.aspx Investigating and analysing incidents, complaints and claims to learn from experience http://nww.swyt.nhs.uk/docs/Documents/776.doc Mandatory training home page http://nww.swyt.nhs.uk/learningdevelopment/Pages/Mandatory-training.aspx Managing aggression and violence (MAV) home page http://nww.swyt.nhs.uk/mav/Pages/default.aspx Occupational health home page http://nww.swyt.nhs.uk/wellbeing/occupational-health/Pages/default.aspx Policy for Lone Working http://nww.swyt.nhs.uk/Policies/documents/228.doc Protocol for the Prevention of Abuse of Vulnerable Adults http://nww.swyt.nhs.uk/Policies/documents/417.doc Patient safety home page http://nww.swyt.nhs.uk/incidentreporting/Pages/Contact-the-team.aspx Seclusion policy http://nww.swyt.nhs.uk/docs/Documents/396.docx Staff consultancy and counselling service home page http://nww.swyt.nhs.uk/wellbeing/staff-counselling/Pages/default.aspx 32 APPENDIX A What MAV course should I attend? Aggression Management Teamwork – 4 day initial course and 2 day annual update Staff who work with service users on a clinical basis in areas where restraint has been deemed necessary, require this training. For example clinical staff working inWorking Age Adult, Forensic and Older Peoples inpatient areas. Aggression Management Teamwork -Caring Approaches to Aroused Situations (CAAS) Learning Disability 4 day initial course and 2 day annual update Staff who work with service users on a clinical basis in areas where restraint has been deemed necessary, require this training. For example clinical staff working in inpatient areas. Specifically designed for staff working in Learning Disability service and accredited by the British Institute for Learning Disabilities (BILD) Aggression Management De-escalation and Breakaway (Clinical) – 1 Day – (2 Year Refresher). Staff who are not required to restrain but may be exposed to risk in which they may need to breakaway. For example community based clinical staff, lone workers, allied Health Professionals. Aggression Management Personal Safety and Breakaway (non clinical) – ½ Day – (2 Year Refresher) Staff who enter into service user areas or deal with the public but do not have a direct clinical relationship with service users, require this training. For example porters, domestics, ward clerks, receptionists. It includes training on the responsibilities of staff to ensure they keep themselves safe, do not cause risk to others and inform the lead nurse/ head of department of any incidents. Aggression Management Personal Safety Awareness (E-learning) (3 Year Refresher) Staff who rarely service user areas or deal with the public, require this training. For example office or administrative staff. It includes causes of anger and how to manage work based conflict. 33 Appendix B Equality Impact Assessment Tool Equality Impact Assessment Questions: Evidence based Answers & Actions: 1 Name of the policy that you are Equality Impact Assessing MAV policy 2 Describe the overall aim of your policy and context? Who will benefit from this policy? This policy is to support a consistent and positive approach to the management of aggression and violence within South West Yorkshire Partnership NHS Foundation Trust (SWYPFT). It aims to support staff to effectively manage incidents with the aim of reducing the number and severity of incidents of aggression and violence to a minimum All staff 3 Who is the overall lead for this assessment? Director of Nursing Compliance and Innovation 4 Who else was involved in conducting this assessment? Network Leader Managing Aggression and Violence 5 Have you involved and consulted service users, carers, and staff in developing this policy? Members of the MAV TAG and Health and safety TAG were consulted. Key clinicians and Managers and were asked to comment. Though service users are represented on the above groups the policy will be reviewed by a service user and carer group. What did you find out and how have you used this information? 6 What equality data have you used to inform this equality impact assessment? N/A 7 What does this data say? N/A 8 Have you considered the potential for unlawful direct or indirect discrimination in relation to this policy? Yes 34 9 Taking into account the information gathered. Does this policy affect one group less or more favourably than another on the basis of: Where Negative impact has been identified please explain what action you will take to mitigate this. If no action is to be taken please explain your reasoning. YES 10 NO Race N Disability Y Gender N Age N Sexual Orientation N Religion or Belief N Transgender N What measures are you implementing or already have in place to ensure that this policy: promotes equality of opportunity, promotes good relations between different equality groups, eliminates harassment and discrimination On Teamwork Clinical 2 courses a level of physical ability is required. Occupational health will make a functional assessment of individuals and a judgement made as to whether the condition is permanent or temporary. The MAV Team will attempt to make reasonable adaptations to physical techniques. If no adaptations can be made the individuals manager and Occupational Health will be informed This policy is a standing item for discussion at the MAVTAG where issues can be identified and acted upon. 11 Have you developed an Action Plan arising from this assessment? If yes, then please attach any plans at the back of this template N/A 12 Who will approve this assessment and when will you publish this assessment. Executive Management Team When revised policy is approved by Trust Board 35 Version Control Sheet This sheet should provide a history of previous versions of the policy and changes made Version Date Author Status Comment / changes 1 6th October 2008 Mark Kidder Final New Policy 2 7th October 2010 Mark Kidder Final Revision - Addition of Restraint Monitoring Form Equality Impact Assessment Conversion to Business Delivery Units Update of training risk continuum and addition of E – learning package. 3 1st October 2012 MAV tag Final Synthesised with BBDU 4 Sept 15 MAV Tag Final Revision in relation to Department of Health. (2015). Mental Health Act 1983 Code of Practice. Meeting Needs and Reducing Distress: guidance on the prevention and management of clinically related challenging behaviour in NHS settings. Department of Health, NHS Protect. (2013). Positive and Proactive Care: reducing the need for restrictive interventions.Department of Health. (2014). Violence and Aggression: Short-term management in mental health, health and community settings. Updated edition. NICE Guideline NG10 (2015) British Institute of Learning Disabilities Code of Practice forminimising the use and reduction of physical interventions:planning, developing and delivering training (2014) A Positive and Proactive 36 Workforce: a guide to workforce development for commissioners and employers seeking to minimise the use of restrictive practices in social care and health. Skills for Health and Skills for Care.(2014) These include guidance to the use of prone restraint and high level holds. The use of mechanical restraint Use of individual support plans 37